Background and Objectives: Student-run free clinics (SRFCs) have been proposed as one educational strategy to increase medical students’ interest in primary care careers. We sought to overcome gaps in the literature by investigating the effect of opening an SRFC at different institutions on institution-level match rates into family medicine, the largest source of primary care physicians in the United States.
Methods: We connected a list of SRFCs from primary care clerkship directors and the Society of Student-Run Free Clinics with a database of institution-level match rates into family medicine from 2000 to 2018. Using regression discontinuity analysis, we assessed whether opening an SRFC would increase family medicine match rates.
Results: Across a sample of 58 medical schools in the United States, we found that SRFCs did not significantly change the number (P=.44) or percentage of medical graduates (P=.42) entering family medicine residency. We also found no significant effects of SRFCs on the number of students entering family medicine in different contexts, including public/private institutions (P=.47), geographic areas (P=.26), departmental administrative structures (P=.69), and institutions with higher historical rates of producing graduates entering family medicine (P=.22).
Conclusions: Though SRFCs may potentially support other aspects of undergraduate medical training, they should not be used as a singular strategy for addressing shortages in the primary care workforce in the United States. Further educational research should examine multipronged strategies to increase the supply of early-career primary care physicians in the United States.
Currently, a large mismatch exists between the number of primary care physicians available in the United States and the need for primary care services. This situation is worsening over time due to a growing and aging population, more chronic illness, and the expansion of health insurance. 1, 2 Unfortunately, this gap is further exacerbated by declining interest in entering primary care practice among US medical school graduates. For example, after surging interest in family medicine in the 1990s among US medical school graduates to a peak of nearly 20%, interest has sharply decreased, with medical school graduates matching into family medicine at a rate of only 8.1% by 2021. 3
Because the demand for primary care services is relatively difficult to change, many efforts to address this mismatch have focused on addressing declining interest in primary care practice among medical students. Attempts to do so have spanned multiple levels, including policy, curricular design, clerkships, and extracurricular activities such as student-run free clinics (SRFCs). 4, 5 However, evidence of these myriad interventions increasing medical student interest in entering primary care has been limited. 6 As a result, many have called for higher quality research studies to identify how to attract students to family medicine. 3, 4, 5, 7-13
One of the areas where significant investment has been made to potentially increase students’ interest in primary care has been the expansion of SRFCs. SRFCs have become common in US medical education today, with their presence now at more than 75% of allopathic medical schools across the country. 14 Though these clinics are sometimes touted as ways both to complete service learning and to deepen interest in primary care, 5, 15, 16 few high-quality studies have examined the effect of SRFCs on primary care career outcomes. In one recent review by Sairenji and colleagues, of seven identified articles examining the impact of SRFCs on students’ interest in primary care, only two reported a positive association with primary care interest. 7 Of those two studies, one study conducted in the 1980s found a relationship between participating in an SRFC and matching into family medicine, 17 while the other found that SRFC involvement was associated with higher self-reported interest in primary care but did not investigate actual specialty choice. 15 In studies finding no association between SRFCs and medical student interest in primary care, all were conducted in single institutions with limited generalizability. 16, 18, 19 The only study noted to date that examined patterns of SRFCs across institutions was conducted in 2005 and researched the relationship between the presence of SRFCs and overall match rates into family medicine, finding no significant association. 20 In a broader review of the impact of SRFCs on a variety of specialty choice and other educational outcomes, McCray and colleagues found similar results: no association between participation in SRFCs and primary care match rates. 21
This study addresses three main limitations of the extant literature on SRFCs and specialty choice: (a) generalizability across institutions, (b) actual specialty career choice, and (c) methods that account for other potential confounding variables. Using a sample of SRFCs at medical schools across the country, we sought to answer a simple but important question: If a medical school opens a student-run free clinic, will it produce more family medicine physicians?
We performed this analysis by collecting data on SRFCs at both osteopathic and allopathic medical schools throughout the United States and linking that data to family medicine resident data collected by the American Academy of Family Physicians (AAFP).
To collect data about SRFCs around the country, we first designed and distributed a survey asking multiple questions about existing clinics at each respondent’s institution. This survey required respondents to supply four variables: the name of the medical school, the name of the SRFC being reported, the position of the respondent, and the year in which the SRFC opened. The survey also asked respondents to report additional characteristics about the clinic, if available, including the number of annual student volunteers, whether the clinic offers primary care and specialty services, the approximate number of patients seen each year, and the frequency that the clinic is open to see patients. This survey was initially circulated to student leaders of SRFCs affiliated with the national Society of Student-Run Free Clinics in the fall of 2022. However, due to low response rates, we also distributed the survey to a national list of primary care clerkship directors and obtained a list of all affiliated SRFCs from the Society of Student-Run Free Clinics to increase our sample size. In total, approximately 87% of identified SRFCs were members of the Society of Student-Run Free Clinics, while 30% of clinics were identified using our surveys, with many SRFCs identified through both methods.
Using this combined list of clinics, we searched the internet to try to identify when the clinic was opened. This information was collected from various sources, including the clinic website, information pages on the medical school’s main website, and news articles about the opening of the clinic. If multiple clinics were reported at a single institution, the earliest clinic opened was included.
Finally, we linked the SRFC data to an AAFP dataset reporting the number of medical graduates employed as first-year family medicine residents from each medical school across the country from 2000 to 2018. That database also included categorizations of each medical school by location, public/private funding status, and administrative structure of family medicine physicians at the institution based on publicly available data.
To estimate the causal effect of opening an SRFC on match rates into family medicine, we created linear regression discontinuity models for two outcomes: (a) the number of graduates entering family medicine, and (b) the percentage of graduates entering family medicine. The benefit of using this method was that it allowed us to identify whether, compared to the years preceding the creation of the SRFC, any subsequent increases in primary care match rates at each medical school had taken place. This approach allowed us to create a quasi-experimental trial, where each school immediately before the creation of the SRFC could serve as a control group to compare to that same school after the creation of the SRFC. In such designs, the need to control for confounding is limited, because the implementation of an SFRC is unlikely to be contemporaneous with other interventions across schools; that some other intervention occurred at precisely the same time as the creation of each SRFC across all schools and could explain the findings would be highly unlikely. We also included the time relative to the opening of the SRFC for each graduation year within each school to assess time-varying effects; this inclusion allowed us to examine the effect of SRFCs as both immediate and gradual effects, because some SRFCs may have taken time to ramp up.
We further investigated the effect of opening an SRFC on match rates of graduates into family medicine across four different educational contexts: (a) private or publicly funded medical schools, (b) schools east or west of the Mississippi River, (c) departmental or nondepartmental family medicine administrative structures, and (d) schools with a history of producing low numbers (fewer than 10 per year, on average) or high numbers (10 or more per year, on average) of graduates entering family medicine. To do this analysis, we estimated linear models with each factor separately interacted with the regression discontinuity variable (ie, presence or absence of SRFC). Thus, these models allowed us to explore whether any specific contexts could account for SRFCs to be more or less effective.
All statistical analysis was conducted in R (The R Foundation). Significance was interpreted relative to a cutoff of P=.05, with marginal significance reported in some cases when P<.10. This study was reviewed and determined to be exempt by the Columbia University Institutional Review Board in 2022.
We obtained data for 58 medical schools in 31 states across the United States. Nearly all medical schools were allopathic (n=56 [96.6%]). Schools varied by geography, funding status, family medicine administrative structure, contributions to family medicine resident workforce, and year in which the earliest SRFC opened (Table 1).
|
|
n (%)
|
|
Type of medical school
|
|
|
Allopathic
|
56 (96.6)
|
|
Osteopathic
|
2 (3.4)
|
|
Census region
|
|
|
New England
|
2 (3.4)
|
|
Middle Atlantic
|
12 (20.7)
|
|
South Atlantic
|
5 (8.6)
|
|
East North Central
|
11 (19.0)
|
|
East South Central
|
2 (3.4)
|
|
West North Central
|
8 (13.8)
|
|
West South Central
|
8 (13.8)
|
|
Mountain
|
3 (5.2)
|
|
Pacific
|
7 (12.1)
|
|
Funding status
|
|
|
Private
|
19 (32.8)
|
|
Public
|
39 (67.2)
|
|
Family medicine administrative structure
|
|
|
Department
|
51 (87.9)
|
|
Center
|
2 (3.4)
|
|
None
|
5 (8.6)
|
|
Medical graduates (yearly average)
|
|
|
Less than 100
|
15 (25.9)
|
|
100 to 199
|
34 (58.5)
|
|
200 or more
|
9 (15.5)
|
|
Number of graduates entering family medicine (yearly average)
|
|
|
Less than 10
|
22 (37.9)
|
|
10 to 19
|
28 (48.3)
|
|
25 or more
|
8 (13.8)
|
|
Proportion of graduates entering family medicine (yearly average)
|
|
|
Less than 5%
|
12 (20.7)
|
|
5% to 9.9%
|
23 (39.7)
|
|
10% or more
|
23 (39.7)
|
|
Year that earliest SRFC opened
|
|
|
Before 2000
|
15 (25.9)
|
|
2000 to 2009
|
22 (37.9)
|
|
2010 or later
|
21 (36.2)
|
Effect of Opening SRFC on Medical Graduates Entering Family Medicine
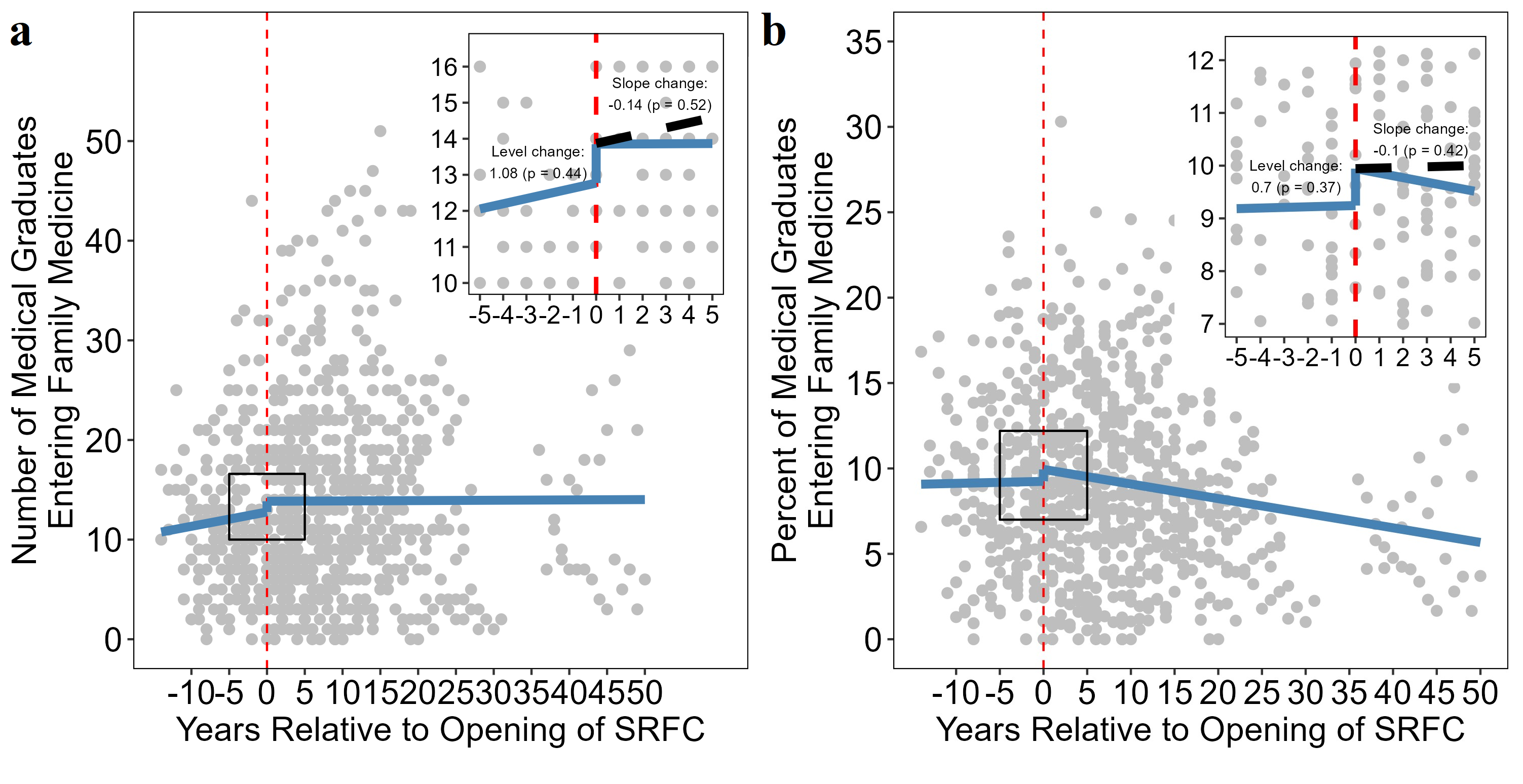
Opening an SRFC was not associated with a significant increase in the number of medical graduates (b=+1.08, 95% CI: [–1.6, 3.8], P=.44; Figure 1a) or percentage of medical graduates (b=+0.70%, 95% CI: [–0.2%, 2.2%], P=.37; Figure 1b) entering family medicine residency. Further, the opening of an SRFC did not significantly affect temporal trends in the number medical graduates (b=–0.14, 95% CI: [–0.6, 0.3], P=.52) or percentage of medical graduates (b=–0.10%, 95% CI: [–0.1, 0.3], P=.42) entering family medicine residency. Accordingly, we further identified that the opening of an SRFC had no significant nonlinear effects on absolute and temporal trends for graduates entering family medicine; this finding suggests that gradual effects of SRFCs on the number of graduates entering family medicine are unlikely. Finally, in sensitivity analyses, these null findings were robust to models in which we varied the observations included based on how close the graduation years were relative to the opening of the SRFC.
Effect of Opening SRFC in Different Institutional Contexts
We found that opening an SRFC was not associated with a significant difference in the number of graduates entering family medicine across schools varying by public/private funding status (P=.47), location east/west of the Mississippi River (P=.26), departmental/nondepartmental family medicine administrative structure (P=.69), or historical production of fewer/more graduates entering family medicine (P=.22).We also found that opening an SRFC was not associated with a significant difference in the percentage of graduates entering family medicine between public/private funding status (P=.07), location east/west of the Mississippi River (P=.09), departmental/nondepartmental family medicine administrative structure (P=.58), or across schools that produce fewer/more graduates entering family medicine (P=.08). Though not significant at our prespecified cutoff of P=.05, public medical schools, medical schools west of the Mississippi River (b=+1.98%), and schools with a history of producing more graduates entering family medicine demonstrated a small increase (1%–2%) in the percentage of graduates entering family medicine residency after the opening of an SRFC.
Using a quasi-experimental design across a diverse sample of more than 50 US medical schools spanning 31 states, we found that the opening of an SRFC was not associated with a significant change in the number or percentage of medical graduates entering family medicine from 2000 to 2018. We further found this lack of effect consistent across different types of schools, including private/public institutions, schools in the eastern or western halves of the country, schools with different family medicine administrative structures, and schools with varying records of producing higher number of graduates entering family medicine. Given the robustness of these results across multiple institutions and contexts, these findings suggest that SRFCs may not be a viable educational strategy, in isolation, to increase medical students’ match rates and careers in primary care.
These results agree with numerous studies suggesting limited efficacy of SRFCs in affecting both interest in and actual match rates into primary care. 7, 15-21 However, this study also addresses many of the limitations of those studies. First, this study focused on actual match/workforce outcomes rather than interest in primary care, the latter of which may not be as reliable for predicting primary care careers. Second, we examined the effect of SRFCs and outcomes across more than 50 schools, adding more reliability to our findings compared to most single-site studies. Third, because of the large sample of medical schools included in this study, we were able to assess school-level factors that could influence the effectiveness of opening an SRFC. Finally, we employed a quasi-experimental method (regression discontinuity) primarily used in economics and political science research to estimate the causal effects of opening an SRFC more accurately. This approach allowed for perhaps the most unbiased estimate of the effect of SRFCs on match rates into family medicine to date.
Our study had several limitations. First, though regression discontinuity is a useful quasi-experimental method, it cannot fully account for the causal effects of SRFCs on family medicine match rates. Second, selection bias might influence the clinics affiliated with the Society for Student-Run Free Clinics, as well as the data we collected separately, potentially omitting clinics that may show an effect of increasing primary care match rates. Also, though this study predominantly evaluated the effects of SRFCs in allopathic medical schools, osteopathic schools are increasingly contributing to the family medicine and overall primary care workforce. Third, we did not explore the effects of different features of SRFCs, such as whether clinics offer primary versus specialty services; different SRFC characteristics possibly may modify the effect of SRFCs on primary care match rates. Fourth, we examined match rates only in family medicine. While family medicine is the specialty with the highest rates of trainees continuing to work in primary care settings, 22, 23 we were not able to assess the potential effect of SRFCs on match rates into other primary care specialties, including internal medicine and pediatrics.
While student-run free clinics may be beneficial for attitudes toward marginalized populations, opportunities to learn clinical and teaching skills, and more, they should not be seen as effective avenues, by themselves, to increase medical students’ interest and match rates into primary care. To increase our supply of primary care physicians in the United States, we should instead focus on interventions that affect broader shares of the medical student population and demonstrate more consistent evidence for changing students’ interest in primary care.
Acknowledgments
The authors acknowledge and thank Shelby Walker, Ada Pariser, Andrea Wendling, and Julie Phillips for their support in collecting family medicine workforce data for this analysis.
References
-
Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians.
Health Aff (Millwood). 2013;32(11):1,881-1,886.
doi:10.1377/hlthaff.2013.0234
-
Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. AAMC; April 2019.
-
-
Ledford CJW, Guard EL, Phillips JP, Morley CP, Prunuske J, Wendling AL. How medical education pathways influence primary care specialty choice.
Fam Med. 2022;54(7):512-521.
doi:10.22454/FamMed.2022.668498
-
Phillips JP, Wendling AL, Prunuske J, et al. Medical school characteristics, policies, and practices that support primary care specialty choice: a scoping review of 5 decades of research.
Fam Med. 2022;54(7):542-554.
doi:10.22454/FamMed.2022.440132
-
Pfarrwaller E, Sommer J, Chung C, et al. Impact of interventions to increase the proportion of medical students choosing a primary care career: a systematic review.
J Gen Intern Med. 2015;30(9):1,349-1,358.
doi:10.1007/s11606-015-3372-9
-
Sairenji T, Kost A, Prunuske J, et al. The impact of family medicine interest groups and student-run free clinics on primary care career choice: a narrative synthesis.
Fam Med. 2022;54(7):531-535.
doi:10.22454/FamMed.2022.436125
-
Lee AL, Erlich DR, Wendling AL, et al. The relationship between medical school clerkships and primary care specialty choice: a narrative review.
Fam Med. 2022;54(7):564-571.
doi:10.22454/FamMed.2022.857719
-
Nguyen BM, Liaw W, Polverento ME, et al. Impact of curricula and electives on primary care specialty choice: a narrative synthesis.
Fam Med. 2022;54(7):572-577.
doi:10.22454/FamMed.2022.638811
-
Seehusen DA, Raleigh MF, Phillips JP, et al. Institutional characteristics influencing medical student selection of primary care careers: a narrative review and synthesis.
Fam Med. 2022;54(7):522-530.
doi:10.22454/FamMed.2022.837424
-
Weidner A. Reflections on the four pillars and our progress toward increased student interest in family medicine.
Fam Med. 2022;54(7):509-511.
doi:10.22454/FamMed.2022.996892
-
Kost A, Phillips JP, Polverento ME, et al. The influence of role modeling and mentorship on primary care career choice: what can be gleaned from 30 years of research?
Fam Med. 2022;54(7):555-563.
doi:10.22454/FamMed.2022.980735
-
Raleigh MF, Seehusen DA, Phillips JP, et al. Influences of medical school admissions practices on primary care career choice.
Fam Med. 2022;54(7):536-541.
doi:10.22454/FamMed.2022.260434
-
Smith S, Thomas R III, Cruz M, Griggs R, Moscato B, Ferrara A. Presence and characteristics of student-run free clinics in medical schools.
JAMA. 2014;312(22):2,407-2,410.
doi:10.1001/jama.2014.16066
-
Smith SD, Yoon R, Johnson ML, Natarajan L, Beck E. The effect of involvement in a student-run free clinic project on attitudes toward the underserved and interest in primary care.
J Health Care Poor Underserved. 2014;25(2):877-889.
doi:10.1353/hpu.2014.0083
-
Weinreich M, Kafer I, Tahara D, Frishman W. Participants in a medical student-run clinic and career choice.
J Contemp Med Educ. 2015;3(1):6-13.
doi:10.5455/jcme.20150321111913
-
Campos-Outcalt DE. Specialties chosen by medical students who participated in a student-run, community-based free clinic.
Am J Prev Med. 1985;1(4):50-51.
doi:10.1016/S0749-3797(18)31400-4
-
Brown A, Ismail R, Gookin G, Hernandez C, Logan G, Pasarica M. The effect of medical student volunteering in a student-run clinic on specialty choice for residency.
Cureus. 2017;9(1):e967.
doi:10.7759/cureus.967
-
Vaikunth SS, Cesari WA, Norwood KV, et al. Academic achievement and primary care specialty selection of volunteers at a student-run free clinic.
Teach Learn Med. 2014;26(2):129-134.
doi:10.1080/10401334.2014.883980
-
Tong STC, Phillips RL, Berman R. Is exposure to a student-run clinic associated with future primary care practice? Fam Med. 2012;44(8):579-581.
-
McCray E, Atkinson WR, McCray CE, et al. Impact of medical student participation in student-run clinics on education, residency selection, and patient care: a review of selected articles.
Cureus. 2022;14(6):e26183.
doi:10.7759/cureus.26183
-
Li J, Zhang Y, Shen Y, Yao J, Grinspan Z. Selection or education? Medical school ranking and medical students’ speciality choice preferences in the United States.
Educ Prim Care. 2019;30(4):202-211.
doi:10.1080/14739879.2019.1603083
-
Choi PA, Xu S, Ayanian JZ. Primary care careers among recent graduates of research-intensive private and public medical schools.
J Gen Intern Med. 2013;28(6):787-792.
doi:10.1007/s11606-012-2286-z



There are no comments for this article.