Background and Objectives: Social determinants of health (SDoH) education has gained popularity in undergraduate medical education; however, emphasis varies, and the curricula or assessment methods are not uniform. This study sought to examine the current SDoH teaching and assessment methods within family medicine clerkships and to identify characteristics associated with SDoH curriculum with multicomponent (two or more) teaching strategies and higher Kirkpatrick levels of assessment (Level 3-behavior change and Level 4-results).
Methods: An online survey was conducted through the 2023 Council of Academic Family Medicine Educational Research Alliance (CERA) Clerkship Directors Survey.
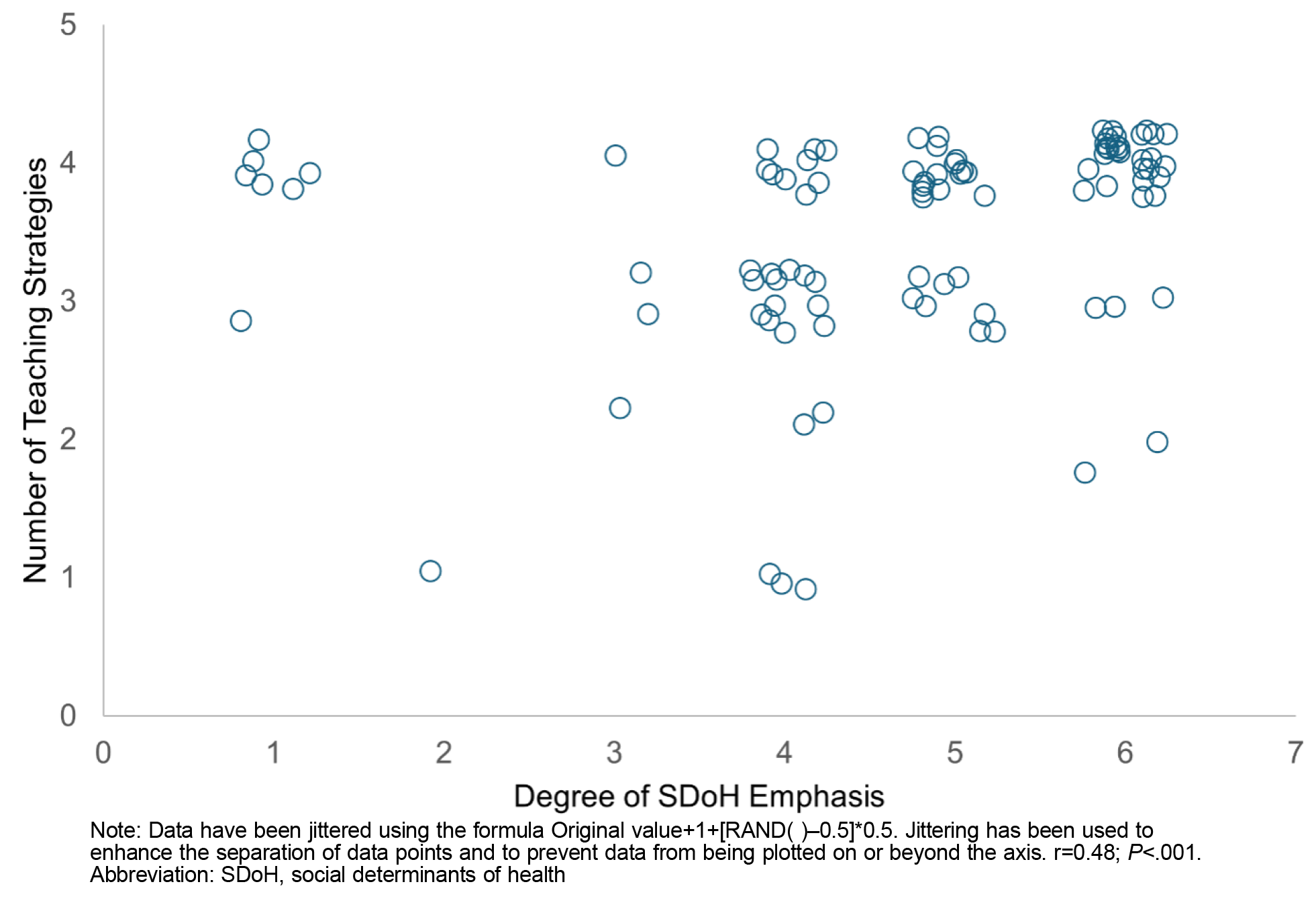
Results: The survey response rate was 56.8% (96/169). The degree of SDoH emphasis in the medical school was positively associated with the number of teaching strategies (r=0.48; P<.001). We found a trend toward degree of SDoH emphasis being associated with higher Kirkpatrick levels of assessment (H[3]=7.83; P=.05). Having an SDoH faculty champion was associated with more teaching strategies (F[1,77]=8.73; P=.004), more types of assessments (F[1,78]=5.88; P=.018), and higher Kirkpatrick levels of assessment (H[1]=4.46; P=.035). Underrepresented in medicine clerkship director identity was not associated with the number of teaching strategies or higher Kirkpatrick levels of assessment.
Conclusions: Greater degrees of SDoH emphasis and having a faculty champion were associated, or trended toward association, with multicomponent teaching strategies and higher Kirkpatrick levels of assessment, which prepare students to provide SDoH responsive care that could lead to reduction in health inequities.
Interest in social determinants of health (SDoH) teaching in undergraduate medical education (UME) is growing. However, SDoH emphasis as well as curriculum and assessment methods vary by school. Out of 29 medical schools, 18 (64%) indicated SDoH teaching as extremely high or high priority, whereas 10 (34%) rated it low priority. 1 SDoH teaching may involve longitudinal curriculum throughout medical school; course, module, or single activity during preclerkship or clerkship; or elective or selective. 1, 2 Assessments often rely on self-reported changes in attitudes, knowledge, and skills, with limited performance-based evaluation. 2 Barriers to extensive training and assessment include lack of faculty expertise in teaching SDoH. 1 Faculty expertise is also a barrier to family medicine residents’ acquisition of SDoH knowledge and skills. 3
SDoH curricula with multicomponent teaching methods (eg, didactic, group discussion, clinical sessions, community experience) and performance-based assessments (eg, direct clinical observation, objective structured clinical exam) are associated with improved knowledge and skills. 4-7 Experiential learning is considered important for acquiring skills necessary to provide SDoH responsive care and to reduce health inequities. 8, 9 Longitudinal and multicomponent curriculum focused on care of medically and socially underserved populations is associated with increased primary care or family medicine match, family medicine specialty selection, and future practice in underserved settings. 10, 11 Prioritizing SDoH and having ample training and availability of tools to address SDoH were associated with increased perceived family medicine resident competency in SDoH. 3
SDoH educational outcomes include changes in attitudes, confidence, knowledge, and skills. 2, 4-7 These outcomes can be categorized into Kirkpatrick’s levels of evaluation: mostly Level 1-reaction and Level 2-learning with some Level 3-behavior and limited Level 4-results. 12 Focus on lower Kirkpatrick levels likely reflects the challenges of SDoH education. Changes in behavior (Kirkpatrick Level 3) and patient outcomes (Kirkpatrick Level 4) can be difficult to assess.
Factors associated with the use of more SDoH educational methods and higher Kirkpatrick levels of assessment in family medicine clerkships are unclear. This study examined characteristics associated with SDoH curricula that use multicomponent teaching strategies and higher Kirkpatrick levels of evaluation.
Procedures
Survey questions were electronically distributed with the 2023 Council of Academic Family Medicine Educational Research Alliance (CERA) Clerkship Director Survey. The study sample included 169 family medicine clerkship directors in the United States and Canada. CERA survey methodology has been described elsewhere. 13 Data were collected May 23 to June 9, 2023.
Measures
Seven survey questions asked about the degree of SDoH emphasis (not at all, very little, somewhat, a lot, to a great extent) within the medical school curriculum; availability of a faculty champion; teaching methods (didactic [lectures], experiential [clinic or community-based] and/or participatory [case-based, small group, or peer-led]); and assessment types (attitude change, knowledge and skills acquisition, behavioral change or performance-based). The CERA surveys were approved by the American Academy of Family Medicine Institutional Review Board.
Analysis
We used χ2, Kruskal-Wallis, Pearson correlation coefficients, and analysis of variance to calculate associations among SDoH education emphasis, the number of teaching strategies (two or more=multicomponent), and Kirkpatrick levels of assessment (higher levels=Level 3 and Level 4). SDoH education data included medical school curricula, faculty champions, clerkship directors self-identifying as underrepresented in medicine (URiM), and clerkship length. We established that α=0.05. No corrections were used for multiple analyses. SPSS version 28.0.1.1 (IBM) was used for analysis.
The survey response rate was 56% (96/169). Clerkships were geographically diverse, almost two-thirds were at publicly funded institutions, and family medicine or primary care clerkship was mandatory at almost all institutions (Table 1). Degree of SDoH emphasis (P<.001) and having a faculty champion (P=.004) were associated with the number of teaching strategies (Table 2). Higher Kirkpatrick levels of assessment were associated with having a faculty champion (P=.035) and trended toward an association with degree of SDoH emphasis (P=.05;Table 2). Figure 1 displays the relationship between the number of teaching strategies and the degree of SDoH emphasis. Clerkship length and clerkship director with URiM identity were not associated with the number of teaching strategies or higher Kirkpatrick levels of assessment.
|
Characteristics
|
n (%)
|
|
Funding source
|
|
|
Public
|
65 (68)
|
|
Private
|
30 (31)
|
|
Region
|
|
|
New England (NH, MA, ME, VT, RI, or CT)
|
7 (7.3)
|
|
Middle Atlantic (NY, PA, or NJ)
|
15 (15.6)
|
|
South Atlantic (PR, FL, GA, SC, NC, VA, DC, WV, DE, or MD)
|
17 (17.7)
|
|
East South Central (KY, TN, MS, or AL)
|
2 (2.1)
|
|
East North Central (WI, MI, OH, IN, or IL)
|
17 (17.7)
|
|
West South Central (OK, AR, LA, or TX)
|
8 (8.3)
|
|
West North Central (ND, MN, SD, IA, NE, KS, or MO)
|
8 (8.3)
|
|
Mountain (MT, ID, WY, NV, UT, AZ, CO, or NM)
|
7 (7.3)
|
|
Pacific (WA, OR, CA, AK, or HI)
|
7 (7.3)
|
|
Canada
|
8 (8.3)
|
|
Typical number of students in one class, M (SD)
|
142.7 (72.4)
|
|
Family medicine or primary care clerkship is mandatory?
|
|
|
No
|
1 (1)
|
|
Yes
|
94 (97.9)
|
|
Year(s) of training when medical students participate in family medicine or primary care clerkship?*
|
|
|
M1
|
0 (0)
|
|
M2
|
11 (11.5)
|
|
M3
|
92 (95.8)
|
|
M4
|
7 (7.3)
|
|
Clerkship director self-identified gender*
|
|
|
Female/woman
|
57 (59.4)
|
|
Male/man
|
37 (38.5)
|
|
Genderqueer/gender nonconforming
|
0 (0)
|
|
Nonbinary
|
0 (0)
|
|
Choose not to disclose
|
0 (0)
|
|
Self-described
|
0 (0)
|
|
Clerkship director self-identified race or ethnicity*
|
|
|
Hispanic/Latino/a/Spanish origin
|
2 (2.1)
|
|
American Indian/Alaska Native/Indigenous
|
1 (1.0)
|
|
Asian
|
19 (19.8)
|
|
Black/African American
|
4 (4.2)
|
|
Native Hawaiian/Pacific Islander
|
0 (0)
|
|
White
|
63 (65.6)
|
|
Middle Eastern/North African
|
3 (3.1)
|
|
Choose not to disclose
|
5 (5.2)
|
|
Clerkship director identifies as underrepresented minority?
|
|
|
No
|
76 (79.2)
|
|
Yes
|
17 (17.7)
|
|
Predictor
|
Outcome
|
Statistic
|
P value
|
|
Degree of SDoH emphasis
|
Number of teaching strategies
|
r=0.48
|
<.001
|
|
|
Kirkpatrick level
|
H(3)=7.83
|
.050
|
|
SDoH faculty champion
|
8+ years of SDoH curriculum
|
χ2=0.40
|
.526
|
|
|
Number of assessment types
|
F(1,78)=5.88
|
.018
|
|
|
Number of teaching strategies
|
F(1,77)=8.73
|
.004
|
|
|
Kirkpatrick levels
|
H(1)=4.46
|
.035
|
|
Clerkship length (4+ weeks)
|
Number of teaching strategies
|
F(1,73)=0.01
|
.910
|
|
|
Kirkpatrick levels
|
H(1)=0.00
|
.971
|
|
Clerkship length (5+ weeks)
|
Number of teaching strategies
|
F(1,73)=0.01
|
.941
|
|
|
Kirkpatrick levels
|
H(1)=0.33
|
.567
|
|
Clerkship director self-identifies as URiM
|
Number of teaching strategies
|
F(1,92)=0.89
|
.348
|
|
|
Kirkpatrick levels
|
H(1)=0.08
|
.776
|
Greater SDoH emphasis, having a longitudinal SDoH curriculum, and having a faculty champion were associated with multicomponent teaching strategies and trended toward association with higher Kirkpatrick levels of assessment. Presumably, exposure to multicomponent teaching strategies and higher Kirkpatrick assessment levels would lead to higher levels of SDoH knowledge and skills. 4-7 Barriers to optimal SDoH education include time, funding, faculty expertise, and availability of meaningful experiential learning. 2, 3
The National Academies of Sciences, Engineering, and Medicine recommends that SDoH education should be “experiential, integrated, and collaborative across the learning continuum.” 14 This goal requires appropriate leadership backing and sufficient funding to provide meaningful education that goes beyond fulfilling accreditation requirements and “inspires desire for lifelong learning in how to mitigate the root causes of ill health and disease.” 14 One such root cause is systemic racism, an upstream structural driver and a SDoH. 15 The majority of family medicine clerkships do not have a curriculum on systemic racism. 16
Medical school leadership is essential for greater SDoH emphasis. Emphasis could mean more curricular time and teaching resources, faculty development, and/or efforts to inspire interest among faculty and students. With no standard SDoH curriculum, creating a customized SDoH curriculum consisting of structural drivers such as systemic racism is required. Development of such curriculum needs an invested faculty member with content expertise.
Clerkship director with URiM identity was not associated with multicomponent teaching strategies or higher Kirkpatrick levels of assessment. Similarly, we found no association between URiM identity and having a curriculum on systemic racism in family medicine clerkships. 16 Additionally, proportions of URiM family medicine faculty or residents were not associated with perceived resident competency in SDoH. 3 Faculty expertise, alongside leadership support for dedicated time and resources, is needed to create a curriculum with multicomponent teaching strategies and higher Kirkpatrick levels of assessment. Leadership should be careful not to increase the minority tax of URiM faculty through the assignment of SDoH directors without proper support or expertise. 17
Our study may have had response bias. Some clerkship directors may not have been knowledgeable about the medical school curriculum and inaccurately answered questions. Clerkship directors also could have inaccurately estimated the time spent on each teaching strategy and/or inaccurately reported the forms of assessment used. The results were not corrected for multiple analyses being conducted, possibly increasing the risk of Type 1 error (ie, false positive). Lastly, our study may have had selection bias, with participation of only clerkship directors interested in the topic.
Greater degrees of SDoH emphasis, having a longitudinal SDoH curriculum, and having a faculty champion were associated with multicomponent teaching strategies and trended toward association with higher Kirkpatrick levels of assessment. SDoH education consisting of experiential learning and assessment that evaluates behavior change and outcomes is important in ensuring that students develop the skills to provide SDoH responsive care that could lead to reduction in health inequities.
Exploring relationships between teaching methods and higher Kirkpatrick levels of assessment is essential. Learning about SDoH curricula characteristics throughout medical school would give a complete picture of SDoH education in UME. Moreover, knowing whether family medicine clerkships with SDoH multicomponent teaching strategies and higher Kirkpatrick levels of assessment have higher family medicine match rates is important. Ultimately, future studies need to evaluate whether SDoH teaching in UME leads to decreases in health inequity.
Disclaimer
The opinions and assertions expressed herein are those of the authors and do not necessarily reflect the official policy or position of the Uniformed Services University or the Department of Defense.
References
-
Lewis JH, Lage OG, Grant BK, et al. Addressing the social determinants of health in undergraduate medical education curricula: a survey report.
Adv Med Educ Pract. 2020;11:369-377.
doi:10.2147/AMEP.S243827
-
Doobay-Persaud A, Adler MD, Bartell TR, et al. Teaching the social determinants of health in undergraduate medical education: a scoping review. J Gen Intern Med. 2019;34(5):720-730. doi:10.1007/s11606-019-04876-0
-
Wright KM, Ravenna P, Wheat S, Villarreal CM, Clements DS, Cronholm PF. Social determinants of health in family medicine residency: a national survey of program directors.
Fam Med. 2024;56(2):102-107.
doi:10.22454/FamMed.2023.871989
-
Asgary R, Naderi R, Gaughran M, Sckell B. A collaborative clinical and population-based curriculum for medical students to address primary care needs of the homeless in New York City shelters: teaching homeless healthcare to medical students.
Perspect Med Educ. 2016;5(3):154-162.
doi:10.1007/S40037-016-0270-8
-
Bernstein R, Ruffalo L, Bower D. A multielement community medicine curriculum for the family medicine clerkship.
MedEdPORTAL. 2016;12:10417.
doi:10.15766/mep_2374-8265.10417
-
-
Erlich M, Blake R, Dumenco L, White J, Dollase RH, George P. Health disparity curriculum at the Warren Alpert Medical School of Brown University. R I Med J (2013). 2014;97(9):22-25.
-
Sharma M, Pinto AD, Kumagai AK. Teaching the social determinants of health: a path to equity or a road to nowhere?
Acad Med. 2018;93(1):25-30.
doi:10.1097/ACM.0000000000001689
-
McNeil R, Guirguis-Younger M, Dilley LB, Turnbull J, Hwang SW. Learning to account for the social determinants of health affecting homeless persons.
Med Educ. 2013;47(5):485-494.
doi:10.1111/medu.12132
-
Kost A, Benedict J, Andrilla CH, Osborn J, Dobie SA. Primary care residency choice and participation in an extracurricular longitudinal medical school program to promote practice with medically underserved populations.
Acad Med. 2014;89(1):162-168.
doi:10.1097/ACM.0000000000000075
-
Kost A, Evans D, Dobie S, Sanders E. What is the impact of the underserved pathway program on graduates entering an underserved family medicine residency? five-year findings from the University of Washington School of Medicine.
Acad Med. 2018;93(7):1,042-1,047.
doi:10.1097/ACM.0000000000002073
-
Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick Four Levels of Training Evaluation. Association for Talent Development; 2016.
-
-
Committee on Educating Health Professionals to Address the Social Determinants of Health; Board on Global Health; Institute of Medicine; National Academies of Sciences, Engineering, and Medicine. A Framework for Educating Health Professionals to Address the Social Determinants of Health. National Academies Press (US); October 14, 2016.
-
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions.
Lancet. 2017;389(10,077):1,453-1,463.
doi:10.1016/S0140-6736(17)30569-X
-
Bridges KM, Rampon K, Mabachi N, et al. More than half of family medicine clerkships do not address systemic racism: a CERA study.
Fam Med. 2023;55(4):217-224.
doi:10.22454/FamMed.2023.581155
-
Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax?
BMC Med Educ. 2015;15:6.
doi:10.1186/s12909-015-0290-9



There are no comments for this article.