Background and Objectives: Proficiency in procedural care achieved during residency is a major driver of family physician scope of practice. To date, no inventory exists of the advanced procedures and clinical skills performed by teaching family physicians. This study comprises the first such survey and assesses the attitude of respondents toward the importance of family physicians performing procedures.
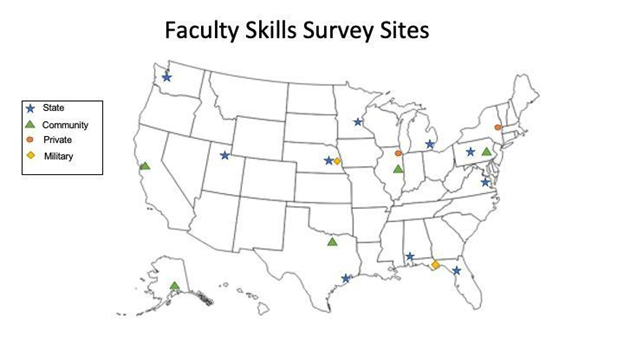
Methods: We sent a clinical skills inventory to a convenience sample of teaching family physicians employed at 18 medical school-affiliated, community, and military residency programs across the United States.
Results: The overall response rate was 46% (N=337). Respondents performed a median of 12 advanced procedures and clinical skills (IQR: 8-18). Endorsed procedures ranged from skin biopsy (n=316, 93.8%) and joint injection (n=279, 82.8%) to colonoscopy (n=21, 6.2%) and cesarean delivery (n=23, 6.8%), and reported skills ranged from medication-assisted treatment (n=181, 53.7%) to highly active antiretrovial therapy (n=35, 10.4%). Gender and career stage were associated with statistically significant differences in endorsement of specific procedures. For example, fracture management was more likely to be performed by late- versus early-career faculty (54.1% vs 24.2%, P<.001) and by male versus female respondents (54.9% vs 24.2%, P<.001). Most respondents (84.3%) agreed that future family physicians should learn procedures and advanced clinical skills.
Conclusions: Family medicine teaching faculty perform a wide array of procedures and advanced skills. Apparent differences by career stage and gender identity in the performance of some of the procedural and skill areas may portend a shift in the procedural training of future family physicians.
Since its inception as a novel medical field with unique board certification in 1969, family medicine has included in its scope many office- and hospital-based procedures to meet the varying needs of patients. Within a family medicine practice, basic procedural skills, such as simple laceration repair, are expected to be mastered by the time of graduation from residency. Family physicians also acquire advanced procedural and clinical skills that require supplemental training or fulfillment of special credentialing processes to practice, such as cesarean delivery, joint injections, colonoscopy, and medication-assisted therapy.
The benefits of a broad scope of practice identified in previous studies include enhanced physician well-being, burnout prevention,1, 2 and optimization of quality of care in the form of reduced health care costs and decreased hospitalization rates.3 Several studies have highlighted concern that the scope of family medicine may be narrowing; clearly, the actual procedures and advanced clinical skills performed by family physicians have changed over time.4-11 For example, the number of family physicians who deliver babies has dropped considerably over the past 40 years.12 Nevertheless, new graduates anticipate providing a broader scope of services than current practitioners, including inpatient and obstetrical procedures. 9, 13
American Academy of Family Physicians (AAFP) policy calls for residencies to “strive to teach residents all procedures within the scope of family practice” and to “have faculty who practice a broad array of procedures and skills.”14 The Accreditation Council for Graduate Medical Education’s program requirements for family medicine align, stipulating that “Residents must receive training to perform clinical procedures required for their future practices in ambulatory and hospital environments. 15” Practice scope is commonly determined by skills attained during residency. Knowledge of what family medicine residency graduates plan to incorporate in their future practice is paramount to predict their actual scope within 5 years after graduation.16-19 Thus, growing a broad set of skills in residency through working with procedurally proficient faculty likely increases a graduate’s potential scope of practice. Yet, while published data are available on the skill sets of practicing family physicians,20 to date no reports exist on the scope of practice of family medicine teaching faculty.
Our study addressed this knowledge gap through surveying a broad geographic range of family medicine faculty from academic, community-based, and military residency programs. Our findings offer preliminary data that may help guide resident training and future scope of practice for family physicians.
Survey
Our anonymous survey consisted of a narrative introduction explaining the purpose of the study and an inclusion question to verify respondents’ completion of a family medicine residency. Table 1 highlights additional surveyed demographic information.
|
|
Total
N
=337
n (%)
|
Early career (n=120),
n (%)
|
Midcareer (n=106),
n (%)
|
Late career (n=111),
n (%)
|
|
Credentials
|
|
MD
|
302 (89.6)
|
103 (85.8)
|
96 (90.6)
|
103 (92.8)
|
|
DO
|
29 (8.6)
|
17 (14.2)
|
7 (6.6)
|
5 (4.5)
|
|
MBBS
|
6 (1.8)
|
0 (0.0)
|
3 (2.8)
|
3 (2.7)
|
|
Fellowship
|
|
Yes
|
114 (33.8)
|
37 (30.8)
|
38 (35.8)
|
39 (35.1)
|
|
No
|
223 (66.2)
|
83 (69.2)
|
68 (64.2)
|
72 (64.9)
|
|
Gender identity
|
|
Female
|
186 (55.2)
|
86 (71.7)
|
66 (62.3)
|
34 (30.6)
|
|
Male
|
144 (42.7)
|
33 (27.5)
|
37 (34.9)
|
74 (66.7)
|
|
Transgender
|
0 (0.0)
|
0 (0.0)
|
0 (0.0)
|
0 (0.0)
|
|
Gender nonbinary, genderqueer, or gender nonconforming
|
1 (0.3)
|
0 (0.0)
|
1 (0.9)
|
0 (0.0)
|
|
Two spirit
|
1 (0.3)
|
0 (0.0)
|
0 (0.0)
|
1 (0.9)
|
|
Prefer not to say
|
4 (1.2)
|
0 (0.0)
|
2 (1.9)
|
2 (1.8)
|
|
Other
|
1 (0.3)
|
1 (0.8)
|
0 (0.0)
|
0 (0.0)
|
|
Race and ethnicity
|
|
Asian or Asian American
|
23 (6.8)
|
8 (6.7)
|
12 (11.3)
|
3 (2.7)
|
|
Hispanic or Latino/a/x
|
19 (5.6)
|
8 (6.7)
|
6 (5.7)
|
5 (4.5)
|
|
Black or African American
|
10 (3.0)
|
5 (4.2)
|
4 (3.8)
|
1(0.9)
|
|
American Indian or Alaska Native
|
2 (0.6)
|
1 (0.8)
|
1 (0.9)
|
0 (0)
|
|
Middle Eastern
|
7 (2.1)
|
5 (4.2)
|
2 (1.9)
|
0 (0)
|
|
Pacific Islander
|
0 (0)
|
0 (0)
|
0 (0)
|
0 (0)
|
|
Mixed race
|
3 (0.9)
|
1 (0.8)
|
1 (0.9)
|
1 (0.9)
|
|
White
|
266 (78.9)
|
96 (80.0)
|
73 (68.9)
|
97 (87.4)
|
|
Prefer not to say
|
12 (3.6)
|
1 (0.8)
|
8 (7.5)
|
3 (2.7)
|
|
Other
|
4 (1.2)
|
0 (0)
|
3 (2.8)
|
1 (0.9)
|
|
Total
|
346 (102.7)
|
125 (104.2)
|
110 (103.7)
|
111 (100.0)
|
A preliminary literature review yielded no validated, contemporary inventory of advanced procedures and skills performed by family physicians. Therefore, we modified a list of procedures published on the AAFP website (originating from a 2018 AAFP member census) to produce a list of 47 procedures and skills we consider to reflect contemporary advanced clinical skills or procedures known to be performed by some family physicians.20 For each skill, respondents were asked whether they “would comfortably perform [the particular skill] independently with a patient” (Appendix Table 1). We deliberately selected the language of “comfortably perform” to allow a physician to respond in the affirmative if they would still offer this service to a patient, even if they had not recently performed that procedure, on the grounds that they could therefore role model or teach this skill to a learner. A small group of physician respondents performed pilot and cognitive testing on the draft survey, and their feedback was incorporated into the final survey instrument.
We included two open-ended questions to allow participants to report skills not included in the survey list and to submit any additional comments about the survey. We additionally asked respondents to globally rate the importance of teaching advanced procedural skills to future family physicians through a five-point Likert scale of attitude measurement. The scale options were very unimportant, unimportant, neutral, important, very important.
Survey Distribution
The survey was distributed to a convenience sample of 18 family medicine departments across the United States between November 2021 and September 2022 (Figure 1). We selected the sites from among those with which we had a faculty contact who agreed to be site lead and with a goal of including a diverse geographic range of institution types and locations. Sites encompassed academic, military, and community residency settings representing approximately 739 faculty members. An email from the research team with a direct link to the survey was distributed to teaching faculty in 14 departments of family medicine and residency programs. Four departments could not provide individual faculty email addresses; therefore, the site lead forwarded an email with an embedded link via internal communication channels.
Data Analysis
We collected and managed survey data in a Research Electronic Data Capture (REDCap [Vanderbilt]) database21, 22 and analyzed the data using SPSS version 28 (IBM Corp).
We reported descriptive counts and percentages for demographic and skill endorsement data. We defined career stages by reported residency graduation year: early (2012-2021), mid (2002-2011), and late (1972-2001) career. We performed χ2 tests to explore associations between the endorsement of individual skills and demographic variables of interest (ie, gender and career stage). Because we performed many exploratory tests on the same data set, we employed conservative Bonferroni correction to identify endorsed skills that were significantly different across groups. The adjusted P value for statistical significance was P<.001. All of us reviewed the additional write-in comments, discussed them, and agreed on themes. Individual responses were exported into Nvivo (Lumivero).
Institutional Review Board
This study was reviewed by the Institutional Review Board of the University of Minnesota and was determined to not be human subjects research, as defined by Department of Health and Human Services and Food and Drug Administration regulations.
Survey Response Rate
We received completed responses from 337 eligible family medicine faculty members across 18 institutions. An additional 21 surveys were received from faculty who had not completed a family medicine residency and were not eligible for the study (ie, PharmD and behavioral health faculty). Among the 14 departments that received individualized invitations, we received 272 (48%) of a possible 563 responses. We received a total of 65 responses from 176 faculty from the four departments that used a generic survey link for a total response rate of 337 (46%) out of an estimated possible 739.
Survey Population
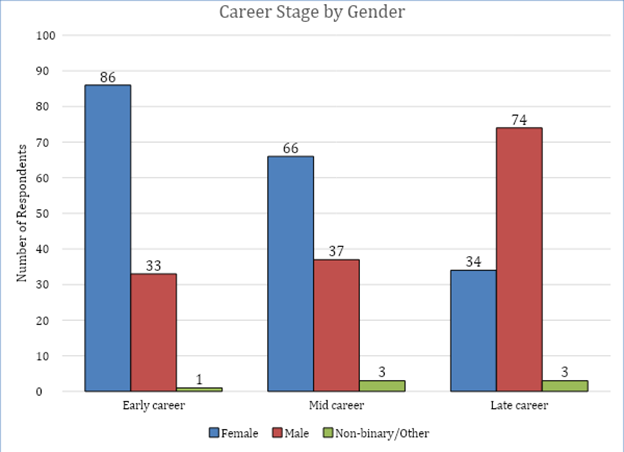
Responding institutions included nine state medical schools (n=226, 67.1%), two private medical schools (n=21, 6.2%), two military residency programs (n=22, 6.5%), and five community residency programs (n=68, 20.2%; Figure 1 ). Table 1 and Figure 2 provide the respondents’ demographic information. Participants graduated from family medicine residency between 1972 and 2021, with a median graduation year of 2008. Approximately one-third of the survey participants completed additional postresidency fellowship training (n=114, 33.8%).
While more than than 65% of respondents who graduated from family medicine residency more than 30 years ago identified as male, more than 70% of those who graduated from residency less than 10 years ago identified as female. Nearly 80% of respondents self-identified as White, with minimal differences between the career stages.
Skill and Procedure Endorsement
We presented participants with an inventory of 47 skills and asked them to check all skills or procedures that “you would comfortably perform independently with a patient” (Appendix Table 1). A total of 4,553 items were endorsed, with a median of 12 skills and procedures per respondent (IQR: 8-18). From the entire survey sample, the top 10 skills that faculty were comfortable performing independently with a patient were skin biopsy (93.8%), sebaceous cyst excision (84.3%), joint injections (82.8%), insertion/removal of intrauterine device (IUD, 77.7%), ingrown toenail removal (75.4%), insertion/removal of subcutaneous contraceptive (74.2%), endometrial biopsy (66.2%), anoscopy (56.1%), medication-assisted therapy for opioid use disorder (53.7%), and circumcision (51.0%). The remaining skills and procedures polled were endorsed by fewer than 50% of the participants.
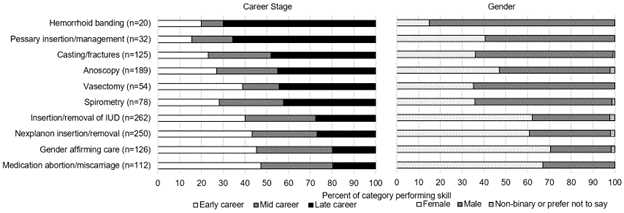
We identified differences by gender and by years since graduation in endorsement of select skills and procedures (Figure 3). Several reproductive health-related skills and procedures were performed more often by female faculty compared to male faculty, and by early- and midcareer faculty compared to late-career faculty. These (all P<.001) included:
-
IUD insertion and removal (male: n=93, 64.6%; female: n=163, 87.6%; early: n=105, 87.5%; mid: n=44, 41.5%; and late: n=25, 22.5%),
-
medication abortion/miscarriage management (male: n=37, 25.7%; female: n=75, 40.3%; early: n=53, 44.2%; mid: n=37, 34.9%; and late: n=22, 19.8%), and
-
gender-affirming care (male: n=35, 24.3%; female: n=89, 47.8%; early: n=57, 47.5%; mid: n=44, 41.5%; and late: n=25, 22.5%).
Conversely, casting and fracture management (P<.001) was more likely to be performed by male faculty (n=79, 54.9%) compared to female faculty (n=45, 24.2%) and more likely to be performed by late-career (n=60, 54.1%) than midcareer (n=36, 34.0%) or early-career faculty (n=29, 24.2%). Additional selected skills with notable differences between career stage and gender are presented in Figure 3.
Additional Skills and Procedures Write-ins
Participants were given an opportunity to report skills and procedures that were not included in the surveyed list. The survey asked, “Please write in an office- or hospital-based skill—that is not listed above—you would comfortably perform independently with a patient.” Participants wrote in a total of 219 additional procedures. Two main skill areas were prominently represented: dermatologic procedures and pain management modalities. A total of 106 dermatologic skills were written in, encompassing 20 different procedures, the most common of which were cryotherapy (n=23), laceration repair (n=23), and abscess incision and drainage (n=21). A total of 40 pain management modalities were reported, encompassing 16 procedures, the most common of which was trigger point injection (n=13). All other write-in skills and procedures were submitted by fewer than 10 participants (Appendix Table 2).
Importance of Skills in Family Medicine
We asked participants to respond to the following statement: “How important is it for future family physicians to learn procedural or additional clinical skills, such as those listed above [in the survey], which may be considered above and beyond the usually expected skills of a family physician?” Most respondents (84.3%) thought that these skills were important or very important.
Write-in Comments
The survey concluded with an open-ended question: “Please share any additional comments you wish on this topic.” Ninety-one participants (27%) provided substantive comments. Three main themes emerged from our review of these responses. Each theme is accompanied by an illustrative quote.
Theme 1. Physicians provide procedures and services needed by their patients and community (36 of 91 comments):
During the pandemic, when all of the specialists shut everything down and primary care was seeing “acute visits” only, we saw many of our patients who needed things that they may have otherwise seen a specialist for but, because we were what was available, they came to us.
Theme 2. Advocacy for continued procedural expertise by family medicine physicians (29 of 91 comments):
As we are all watching the ultra-specialization of medicine rise in the United States despite knowing that we have the worst medical outcomes of any industrialized nation, it is increasingly important that we train fully qualified family medicine physicians to go into the parts of the country that desperately need care, but cannot support a specialty practice.
Theme 3. Performing procedures enhances practice satisfaction (10 of 91 comments):
The job satisfaction provided by doing procedures cannot be underestimated in making sure family physicians are able to maintain their practice and avoid burnout over the long haul. Health care organizations do not count the cost of losing physicians when they view procedures as not worth the time.
To our knowledge, our survey of the scope of practice of more than 300 teachers of family medicine across the United States is the first of its kind and includes faculty from public and private medical schools, community-based residencies, and military programs. Our findings provide initial insight into the procedures being performed by faculty and likely being role modeled for and taught to their family medicine residents. While we built our survey on previously published inventories of skills performed by family physicians, we expanded our survey to include skills more recently incorporated into our field.
A primary driver of postresidency scope of practice is known to be the range of training that happens during residency, both in terms of care settings and procedures.9, 16 Therefore, for teachers of family medicine to maintain a broad scope of practice is key to ensuring the graduation of family physicians ready and able to engage in a broad scope of care. In addition, full-scope faculty have a substantial opportunity to role model the incorporation of procedures and advanced clinical skills within routine medical practice.
Enhancing physician well-being is a significant benefit of performing a broad scope of care in family medicine and aligns with the widely recognized Quadruple Aim.1, 2, 23 The benefits of broad scope of practice extend also to optimizing quality of care; patients treated by physicians who practice a broad scope of care have reduced health care costs and decreased hospitalization rates.3 Whether primary care physicians are present and ready to provide advanced services, such as those needed in maternity care deserts, impacts health equity in underserved regions of the country. 24
The responses to our study demonstrated that teachers of family medicine nationwide agree or strongly agree that learning procedural or advanced clinical skills is important for family physicians. Themes identified within the written responses qualitatively support what has been posited by multiple other studies: teaching family physicians understand that the provision of procedural care must meet the needs of their community and that performance of procedures as part of clinical practice improves career satisfaction.
In keeping with these values, the types of advanced procedures being performed by teachers of family medicine span a broad range. The percentage of respondents performing several of the surveyed procedures is substantially higher than their practicing community physician counterparts and is more closely aligned with the proportion of residents performing these procedures.9, 12 This finding sends a hopeful signal that teachers of family medicine can continue to adequately train those residents whose future practice requires a broad skill set. Yet, given the known benefits of maintenance of a broad scope, this finding is also concerning in that most physicians in general practice cease to use many of the skills they learned in residency. 9
While we observed a wide scope of practice and richness of skills reported, we also saw that skills were sometimes concentrated in groups based on gender or years since graduation from residency. One of the most notable skills being performed by late career and male faculty much more frequently than early career and female faculty was casting and fracture management—once a mainstay of family medicine, now a skill that may have largely shifted to orthopedic urgent care centers.25
If the observed differences in fracture management by years since graduation and gender are reflective of practice trends among teachers of family medicine as a whole, this skill—along with others disproportionally less reported by early career respondents—may be at risk of being lost to the field of family medicine if not more intentionally and equitably taught to early- and midcareer faculty. Moving forward, family medicine residents and training programs ought to work together to leverage the interests of individual physicians to meet the needs of the specialty, building a comprehensive training network that fosters competence in as many procedural and clinical skills as possible.
Limitations of this study included a low response rate from some programs and insufficient power of the survey to make comparisons between types of programs. Because our study was intended to be an initial effort to characterize the scope of practice of teachers of family medicine, we collected only a convenience sample. This convenience sample may not be representative of all family medicine teaching faculty. Additionally, while our survey appeared to oversample women and White-identifying physicians, to date no published representative surveys of the demographics of family medicine faculty are available.
A larger future study with broader sampling would be needed to establish baseline demographics and procedure performance norms for teaching physicians. Such a future study could be designed to measure differences in skill set by gender identity, years since graduation, and practice setting, as well as control for interactions among these variables, such as the higher percentage of male late-career physicians and the higher percentage of female early-career physicians. Additionally, we did not assess whether faculty actively teach the skills surveyed to their learners or whether procedural skills may cluster within institutions, both of which also could be addressed in a follow-up study.
Finally, while we presented a wide array of procedures from which survey respondents could select, many more were added by respondents to an open-ended question. These write-ins precluded us from surveying all respondents on their performance of those skills and is evidence of a wide-ranging difference in understanding of what constitutes an advanced procedural or clinical skill. The write-in skills were possibly more widely performed than we captured.
Family medicine teaching faculty perform a wide array of procedures and advanced skills. Differences are apparent by career stage and gender identification in the performance of some of these procedures and skills. Family physicians in practice are likely to perform mostly the procedures and advanced clinical skills they were taught in residency. Therefore, imperative to the future of the specialty is that teaching family physicians practice, role model, and teach a broad array of procedural and advanced clinical skills.
-
Society of Teachers of Family Medicine Conference on Medical Student Education, New Orleans, LA, January 28, 2023.
Acknowledgments
We appreciate the support of Sherri Fong, MPH, and Derek Hersch, MPH, along with the Research Services Hub in the Department of Family Medicine and Community Health, University of Minnesota Medical School, and all the teaching family physicians who completed our survey.
References
-
Weidner AKH, Phillips RL Jr, Fang B, Peterson LE. Burnout and scope of practice in new family physicians.
Ann Fam Med. 2018;16(3):200-205.
doi:10.1370/afm.2221
-
Zomahoun HTV, Samson I, Sawadogo J, et al. Effects of the scope of practice on family physicians: a systematic review.
BMC Fam Pract. 2021;22(1):12.
doi:10.1186/s12875-020-01328-1
-
Bazemore A, Petterson S, Peterson LE, Phillips RL Jr. More comprehensive care among family physicians is associated with lower costs and fewer hospitalizations.
Ann Fam Med. 2015;13(3):206-213.
doi:10.1370/afm.1787
-
Eden AR, Morgan ZJ, Jetty A, Peterson LE. Proportion of family physicians caring for children is declining.
J Am Board Fam Med. 2020;33(6):830-831.
doi:10.3122/jabfm.2020.06.200089
-
Jetty A, Jabbarpour Y, Petterson S, Eden A, Bazemore A. The declining presence of family physicians in hospital-based care.
J Am Board Fam Med. 2019;32(6):771-772.
doi:10.3122/jabfm.2019.06.190152
-
Barreto T, Peterson LE, Petterson S, Bazemore AW. Family physicians practicing high-volume obstetric care have recently dropped by one-half. Am Fam Physician. 2017;95(12):762-762.
-
Tong ST, Makaroff LA, Xierali IM, Puffer JC, Newton WP, Bazemore AW. Family physicians in the maternity care workforce: factors influencing declining trends.
Matern Child Health J. 2013;17(9):1,576-1,581.
doi:10.1007/s10995-012-1159-8
-
Peterson LE, Nasim U, Madabhushi V. Declining endoscopic care by family physicians in both rural and urban areas.
J Am Board Fam Med. 2019;32(4):460-461.
doi:10.3122/jabfm.2019.04.190064
-
Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians.
JAMA. 2015;314(22):2,364-2,372.
doi:10.1001/jama.2015.13734
-
Bensken WP, Dong W, Gullett H, Etz RS, Stange KC. Changing reasons for visiting primary care over a 35-year period.
J Am Board Fam Med. 2021;34(2):442-448.
doi:10.3122/jabfm.2021.02.200145
-
Peabody MR, O’Neill TR, Stelter KL, Puffer JC. Frequency and criticality of diagnoses in family medicine practices: from the National Ambulatory Medical Care Survey (NAMCS).
J Am Board Fam Med. 2018;31(1):126-138.
doi:10.3122/jabfm.2018.01.170209
-
-
Ludden-Schlatter A, Wells J, Kruse RL. Perspectives on procedure importance: residents, faculty, and community practitioners.
Fam Med. 2018;50(6):450-454.
doi:10.22454/FamMed.2018.779054
-
-
-
Russell A, Fromewick J, Macdonald B, et al. Drivers of scope of practice in family medicine: a conceptual model.
Ann Fam Med. 2021;19(3):217-223.
doi:10.1370/afm.2669
-
Reitz R, Horst K, Davenport M, Klemmetsen S, Clark M. Factors influencing family physician scope of practice: a grounded theory study.
Fam Med. 2018;50(4):269-274.
doi:10.22454/FamMed.2018.602663
-
Peterson LE, Blackburn B, Phillips RL Jr, Mainous AG III. Family medicine department chairs’ opinions regarding scope of practice.
Acad Med. 2015;90(12):1,691-1,697.
doi:10.1097/ACM.0000000000000774
-
Coutinho AJ, Levin Z, Petterson S, Phillips RL Jr, Peterson LE. Residency program characteristics and individual physician practice characteristics associated with family physician scope of practice.
Acad Med. 2019;94(10):1,561-1,566.
doi:10.1097/ACM.0000000000002838
-
-
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support.
J Biomed Inform. 2009;42(2):377-381.
doi:10.1016/j.jbi.2008.08.010
-
Harris PA, Taylor R, Minor BL, et al; REDCap Consortium. The REDCap Consortium: building an international community of software platform partners.
J Biomed Inform. 2019;95:103208.
doi:10.1016/j.jbi.2019.103208
-
Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider.
Ann Fam Med. 2014;12(6):573-576.
doi:10.1370/afm.1713
-
-
Geyman JP, Gordon MJ. Orthopedic problems in family practice: incidence, distribution, and curricular implications. J Fam Pract. 1979;8(4):759-765.



There are no comments for this article.