Background and Objectives: Having a limited number of trained faculty is a barrier to successful incorporation of ultrasound into undergraduate medical education. We evaluated the effectiveness of a resident-led extended focused assessment with sonography in trauma (eFAST) session administered to fourth-year medical students during their emergency medicine clerkship by measuring students’ end-of-year eFAST performance and confidence.
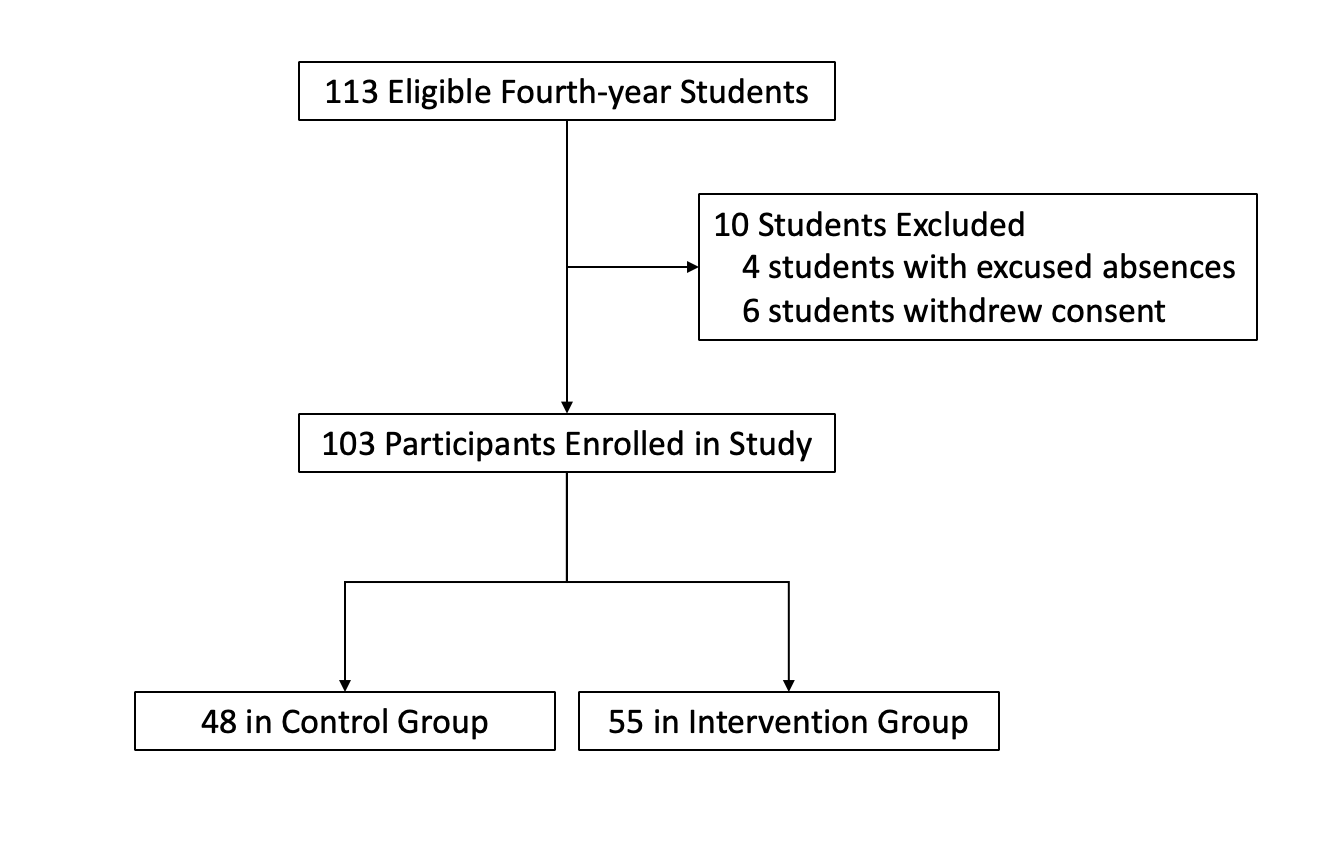
Methods: This was a single-site cross-sectional study of all graduating medical students enrolled in fourth-year clerkships between May 1, 2022 and April 30, 2023. A 60-minute, team-based eFAST session (intervention), taught by emergency medicine residents, was added to students’ fourth-year emergency medicine clerkship in September 2022. All students were assigned to review an eFAST video (control). End-of-year performance and self-reported confidence assessments used a 20-point objective structured clinical examination (OSCE) and a 5-point Likert scale, respectively. The mean OSCE and confidence scores for control and intervention groups were compared using two-sample t tests and repeated after removing students exposed to additional US experiences.
Results: Of 113 eligible students, 103 students participated: 48 in the control group, 55 in the intervention group. The intervention group scored higher on the OSCE than the control group (11.9 ±4.6 vs 9.9 ±5.1, P=.04) and reported similar confidence (3.2 ±1.0 vs 2.8 ±1.2; P=.09). After removing the 28 students with additional US experiences, the intervention group scored higher (10.8 ± 4.4 vs 8.2 ± 4.0; P=.01) and reported higher confidence (3.0 ±1.0 vs. 2.3 ±1.0, P=.01).
Conclusions: Resident-taught eFAST instruction during emergency medicine clerkships led to improved end-of-year fourth-year medical student eFAST performance and confidence.
Point-of-care ultrasound (POCUS) is an important competency for undergraduate medical education 1,2 and graduate medical education programs. 3-5 The technique and clinical utility of the extended focused assessment with sonography in trauma (eFAST) span multiple organ systems, 6 making it integral to any POCUS trainee and a popular target for ultrasound education. 1,2 In addition to detecting traumatic injuries, the eFAST detects nontraumatic fluid accumulation in the thorax and abdomen; and components of eFAST overlap POCUS techniques for pregnancy and renal assessments. This versatility likely is why the American Academy of Family Physicians (AAFP) included eFAST proficiency as a practice-based learning and improvement competency in its curriculum guidelines. 5
However, effective POCUS requires hands-on learning, 2 which can be faculty intensive. 1 Using residents as near-peer teachers offers a solution. 1, 2, 7, 8, 9, 10, 11 In this study, we evaluated the effectiveness of a resident-taught eFAST session for fourth-year medical students during their required fourth-year emergency medicine (EM) clerkship.
Study Design
This was a single-site, cross-sectional, assessor-blinded study of medical students’ end-of-year eFAST performance during the required fourth-year course “Transition to Residency” (TTR). All students enrolled in their EM clerkship and TTR between May 1, 2022 and April 30, 2023 were included. Students with an excused absence from TTR or failure to consent to the study were excluded. The site’s institutional review board deemed the study exempt (IRB #: 23X-133-1).
A 60-minute, resident-led, team-based, hands-on eFAST educational session (intervention) was implemented in September 2022. Students with EM clerkships scheduled after implementation who attended the session were in the intervention group, and all others were in the control group. During the session, students performed the eFAST on one another while receiving real-time feedback from residents on technique and image interpretation. The student-to-resident ratio was 3:1.
Second- and third-year EM residents from a 3-year program with 10 or more hours of eFAST training taught the students during academic time protected from other residency obligations. A checklist, encompassing technique and image interpretation, was used to assess student performance and dually served as a guide for the residents teaching the session.
All students participated in a 34-hour vertical ultrasound curriculum9 and reviewed an eFAST video the week before TTR.
Evaluation and Data Collection
Proficiency in performing the eFAST was assessed using an objective structured clinical examination (OSCE) administered during TTR; scores of nonconsenting students were excluded from analysis. Just before the OSCE, students completed a survey reporting their eFAST experience and confidence. A random numerical identifier was used throughout the data collection process to link students’ survey results with their OSCE scores.
OSCE
A 20-point, previously validated 12 OSCE (Appendix) was administered by first-year medical student volunteers (“proctors”) who served simultaneously as models with step-by-step instructions. Proctors were blinded to the study purpose and group assignment and were not familiar with the eFAST.
Fourth-year students had 6 minutes to complete the OSCE, with instructions (communicated by the proctors) to obtain a 4- to 6-second video of each eFAST view using a Butterfly iQ (Butterfly Network) handheld unit and iPad tablet (Apple, Inc). Proctors were responsible for timing videos, labeling them with student numerical identifiers, and saving them to a cloud.
OSCEs were scored after video review by a single ultrasound fellowship-trained emergency physician blinded to student identity. Points were scored for adequate image acquisition of all six views of the eFAST.
EFAST Survey
Students answered five questions regarding their perceived confidence in performing the eFAST (5-point Likert scale: 1=not confident, 3=neutral, 5=confident), participation in the resident-led eFAST session (yes/no; verified using session attendance sheets), performance of five or more eFAST exams during their clerkships (yes/no), and participation in ultrasound electives or extracurriculars (shadowing, research, or teaching) during medical school (yes/no).
Outcome Measures
Primary outcomes were student eFAST performance (OSCE score) and student self-reported confidence in eFAST performance (5-point Likert scale), according to whether they received the resident-led eFAST session during their EM clerkship.
Statistical Analysis
We used Microsoft Excel (Microsoft Corp) for descriptive statistics and SAS version 9.4 (SAS Institute) for statistical analyses. We compared mean OSCE and confidence scores, with subgroup analyses, between the control and intervention groups using two-sample t tests. We calculated a Pearson correlation coefficient (R) to determine whether the time duration between the student’s EM clerkship and TTR session was associated with outcome.
We conducted power analysis for the primary outcome using two-sample t tests and a two-sided α of 0.05 using the POWER procedure in SAS (SAS Institute, Inc). Assuming a 2-point difference in mean OSCE score between groups was significant (the minimum needed to draw a conclusion about an eFAST finding) and with a predicted standard deviation of 2.5 points, a minimum of 26 subjects per group were needed.
|
|
Total
|
Control
|
Intervention
|
|
Number of
students
|
103
|
48
|
55
|
|
Ultrasound
experience o
utside
r
equired
curriculum
|
|
None
|
75
|
33
|
42
|
|
Ultrasound elective only
|
12
|
6
|
6
|
|
Performed 5 or more eFAST only
|
8
|
4
|
4
|
|
Both ultrasound elective and performed 5 or more eFAST
|
8
|
5
|
3
|
Scores are summarized in Table 2. The student mean OSCE score was 11.0 ± 4.9 out of 20 points. Students who received resident-taught instruction had higher OSCE scores than students who did not (11.9 ± 4.6 vs 9.9 ± 5.1; P=.04). This remained true after removing students with additional ultrasound experiences and repeating the analysis (10.8 ± 4.4 vs 8.2 ± 4.0; P=.01). Confidence also was higher in this subgroup among students exposed to the resident-taught session than those who were not (3.0 ± 1.0 vs 2.3 ± 1.0; P=.005). We found no association between OSCE score and the time interval since students’ EM clerkship (Pearson R: -0.14; P=.31) or confidence score (Pearson R: 0.06; P=.68).
|
|
All
students
|
Control
|
Intervention
|
P
value
|
|
Mean OSCE
scores
(± SD)
|
|
Entire group (N=103)
|
11.0 ± 4.9
|
9.9 ± 5.1
|
11.9 ± 4.6
|
.04
|
|
Subgroup analysis (n=75)*
|
|
8.2 ± 4.0
|
10.8 ± 4.4
|
.01
|
|
Confidence
scores
(± SD)
|
|
Entire group (N=103)
|
3.0 ± 1.1
|
2.8 ± 1.2
|
3.2 ± 1.0
|
.09
|
|
Subgroup analysis (n=75)*
|
|
2.3 ± 1.0
|
3.0 ± 1.0
|
<.01
|
DISCUSSION AND CONCLUSIONS
Medical schools with ultrasound curricula rely heavily on resident instructors, 1 and residents play a significant role in students’ education. 13 Our results support the merit of resident-led instruction, improving student eFAST performance independent of experiences, outside the core curriculum. This brief resident-led intervention was effective and sustainable.
Teaching opportunities benefit residents through knowledge expansion and precision of technical skills. 14 With AAFP incorporating POCUS into family medicine residencies, undergraduate medical education teaching opportunities may help residents pursue their academic goals. Emulating a curriculum that leverages the role of POCUS in family medicine, where family medicine residents teach pertinent applications such as obstetrics/gynecology, sports medicine, and vascular screening, would balance an otherwise EM-centric undergraduate medical education POCUS curriculum.
Both students and residents in our study had well-established POCUS curricula, potentially limiting the generalizability of our results. Recall bias may have influenced eFAST survey responses, particularly when reporting how many eFAST exams were performed during clerkships. Additionally, students pursuing EM residencies were more likely to have their EM clerkship early in their fourth year, and therefore placed in the study control group. These students may seek more POCUS opportunities than others. However, the intervention group still outperformed the control group. This outcome reflects the positive impact of ultrasound teaching on all students. Future studies evaluating the effectiveness of instruction by residents from other specialties, including family medicine, are needed.
In conclusion, resident-led eFAST instruction during a required fourth-year EM clerkship improved medical student eFAST performance later in their fourth year.
Acknowledgments
The authors thank Dr Matthew Ledford, our undergraduate medical education emergency medicine clerkship director, and Dr Shawn London, our emergency medicine residency program director, for their support of the resident-led eFAST ultrasound curriculum during students’ emergency medicine clerkships. We additionally thank Dr Gail Sullivan for her assistance in reviewing and editing this manuscript.
References
-
Russell FM, Zakeri B, Herbert A, Ferre RM, Leiser A, Wallach PM. The state of point-of-care ultrasound training in undergraduate medical education: findings from a national survey.
Acad Med. 2022;97(5):723-727.
doi:10.1097/ACM.0000000000004512
-
Dietrich CF, Hoffmann B, Abramowicz J, et al. Medical student ultrasound education: a WFUMB position paper, part I.
Ultrasound Med Biol. 2019;45(2):271-281.
doi:10.1016/j.ultrasmedbio.2018.09.017
-
-
-
-
Netherton S, Milenkovic V, Taylor M, Davis PJ. Diagnostic accuracy of eFAST in the trauma patient: a systematic review and meta-analysis.
CJEM. 2019;21(6):727-738.
doi:10.1017/cem.2019.381
-
Siegel-Richman Y, Kendall J. Establishing an ultrasound curriculum in undergraduate medical education: how much time does it take?
J Ultrasound Med. 2018;37(3):569-576.
doi:10.1002/jum.14371
-
Hoffmann B, Blaivas M, Abramowicz J, et al. Medical student ultrasound education, a WFUMB position paper: part II, a consensus statement of ultrasound societies.
Med Ultrason. 2020;22(2):220-229.
doi:10.11152/mu-2599
-
Boivin Z, Carpenter S, Lee G, et al. Evaluation of a required vertical point-of-care ultrasound curriculum for undergraduate medical students.
Cureus. 2022;14(10):e30002.
doi:10.7759/cureus.30002
-
Rong K, Lee G, Herbst MK. Effectiveness of near-peer versus faculty point-of-care ultrasound instruction to third-year medical students.
POCUS J. 2022;7(2):239-244.
doi:10.24908/pocus.v7i2.15746
-
Hall S, Harrison CH, Stephens J, et al. The benefits of being a near-peer teacher.
Clin Teach. 2018;15(5):403-407.
doi:10.1111/tct.12784
-
Monti JD, Perreault MD. Impact of a 4-hour introductory eFAST training intervention among ultrasound-naïve U.S. military medics.
Mil Med. 2020;185(5-6):e601-e608.
doi:10.1093/milmed/usaa014
-
Bing-You RG, Sproul MS. Medical students’ perceptions of themselves and residents as teachers.
Med Teach. 1992;14(2-3):133-138.
doi:10.3109/01421599209079479
-
Weiss V, Needlman R. To teach is to learn twice: resident teachers learn more.
Arch Pediatr Adolesc Med. 1998;152(2):190-192.
doi:10.1001/archpedi.152.2.190



There are no comments for this article.