Background and Objectives: Cesarean section (c-section) rates among nulliparous, term, singleton, and vertex (NTSV) pregnancies are increasing, posing risk to the infant and birthing parent. To reach the Healthy People 2030 goal of an NTSV c-section rate below 23.6%, teams must remain aware of their NTSV c-section rate and implement mechanisms to reduce it. This project was conducted to assess the impact of quality improvement interventions implemented by family medicine residents to reduce a hospital’s NTSV rate.
Methods: From 2021 to 2023, family medicine residents were educated on evidenced-based diagnosis of labor dystocia, failed induction of labor, arrest of dilation, and arrest of descent in first-time birthing parents. Learning was reinforced by implementing the Colorado Perinatal Care Quality Collaborative’s labor dystocia checklist. Quarterly assessment of the hospital’s NTSV rate and checklist utilization were monitored and widely reported.
Results: After the implementation of a standard checklist, the NTSV c-section rate at the tertiary care center declined from 35.6% in 2020 to a sustained rate below the 2030 Healthy People goal of 23.6%. Notably, patients with public insurance saw the greatest reduction in NTSV c-section rates. Hospital staff highlighted the benefits of using the checklist, including more effective electronic documentation of labor progression, improvement in team dynamics, and increased team communication.
Conclusions: Using a labor dystocia checklist is a successful method for teams to reduce NTSV c-section rates and can be used as a training tool for family medicine and obstetrics and gynecology residency programs that care for laboring persons.
Despite decades of evidence of effective interventions, 1 cesarean section (c-section) rates are increasing globally.2 Though c-sections can be lifesaving procedures when medically indicated, rates are increasing among nulliparous, term, singleton, vertex (NTSV) pregnancies without clear evidence of need.3 C-sections pose a greater risk to the infant, including risks of admission to the neonatal intensive care unit,4 asphyxia, and lacerations.5 C-section births also cost more6 and pose risks to the birthing parent, including increased rates of death, admission to the intensive care unit, blood transfusion, hysterectomy, 7 and other risks connected with subsequent births (whether by repeat surgery, placental anomalies, uterine perforation, or other causes). The NTSV population has been identified as the most important group to focus on for c-section reduction because this group has been the largest contributor to the rise in c-sections. 8
The Healthy People 2030 goal for NTSV c-sections has been set at 23.6% or less.9 To achieve and maintain this goal, birthing unit teams need mechanisms to track and reduce their NTSV c-section rates.
To achieve this goal in our contemporary context requires renewed vigilance. Evidence-based strategies to reduce NTSV c-section rates include active management of labor, provider accountability, patient-centered care, health system collaboration, incentives for care quality, education, and care standardization.
The Banner North Colorado Medical Center (NCMC), based in Greeley, Colorado, is a 378-bed tertiary center that delivers between 1,200 and 1,400 babies annually. NCMC is the site of the North Colorado family medicine residency training program where residents attend all deliveries and provide primary care for the safety net population, which includes community members who experience the greatest inequities and barriers to accessing care. In 2019, NCMC joined the Colorado Perinatal Care Quality Collaborative (CPCQC) Supporting Vaginal Delivery for Low-Risk Mothers (SOAR) initiative. SOAR aims to reduce unnecessary NTSV c-sections by implementing a labor dystocia checklist, which can be found at https://cpcqc.org/wp-content/uploads/2024/04/CPCQC-Labor-Dystocia_2023_24.pdf. Participation in CPCQC’s SOAR initiative included educating staff, implementing the CPCQC’s labor dystocia checklist, submitting quarterly data from all NTSV deliveries that occurred, reviewing all NTSV c-sections quarterly, attending quarterly educational webinars, and participating in biannual meetings with CPCQC to review NTSV data. Checklists missing responses to half or more of the required fields were marked as “dystocia checklist not completed” prior to coding. To ensure agreement, two separate reviewers assessed the exclusion of data. These data were deemed a quality improvement initiative and did not require institutional review board review.
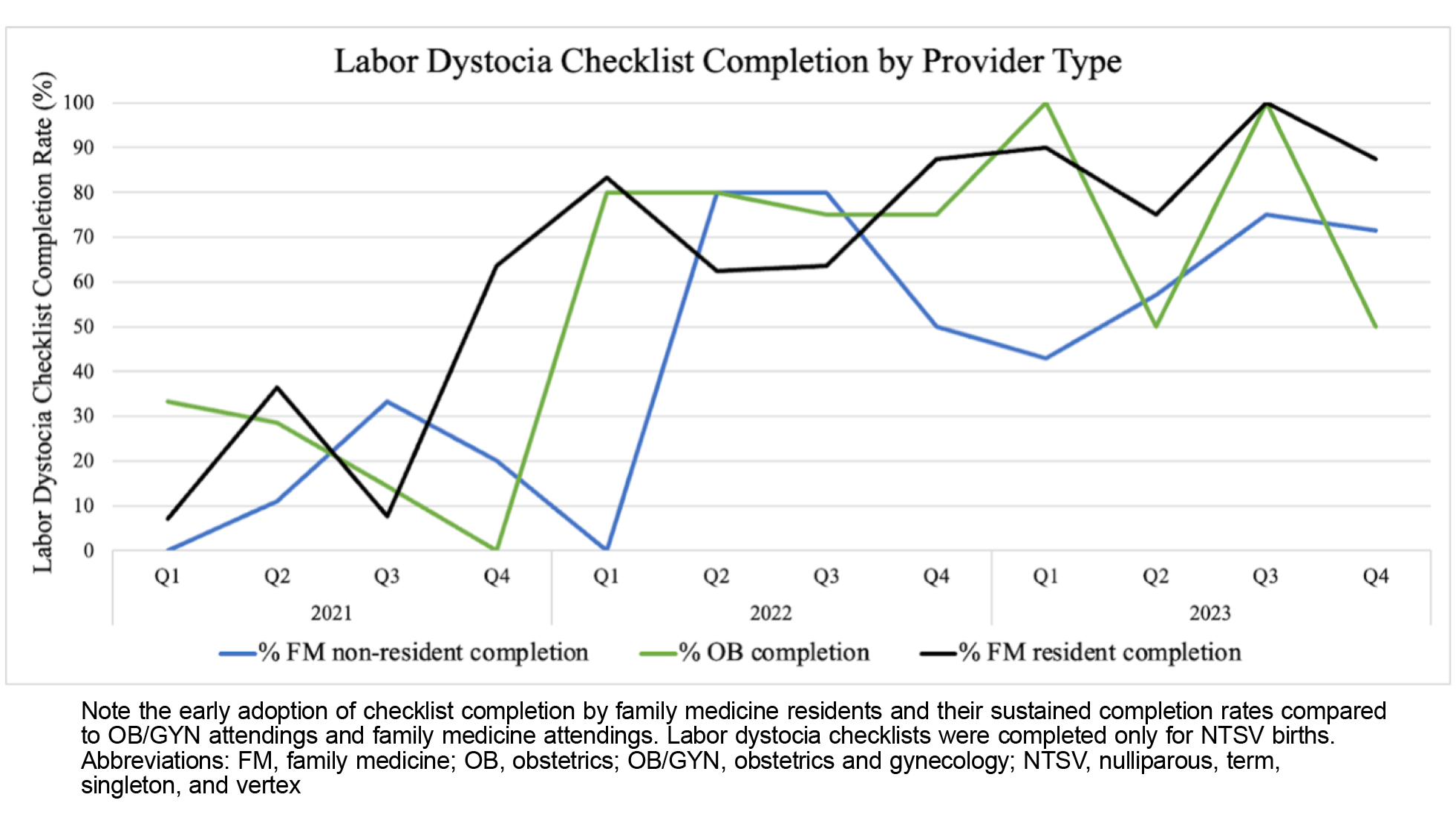
Between 2021 and 2023, NCMC managed 3,901 deliveries. For each delivery, providers made entries in a delivery log with NTSV criteria and outcomes, method of delivery, delivery provider, patient age and gestation length, and labor dystociachecklist completion. Manual chart reviews occurred monthly for patients who met NTSV criteria; age was not a differentiating factor for vaginal versus c-section deliveries. Provider group checklist completion (Figure 1), which was monitored over time, highlighted residents as the early adopters of change. NTSV rates, elective delivery rates, and unexpected complications in term newborns per 1,000 live births also were monitored, reported monthly, and summarized quarterly and yearly.
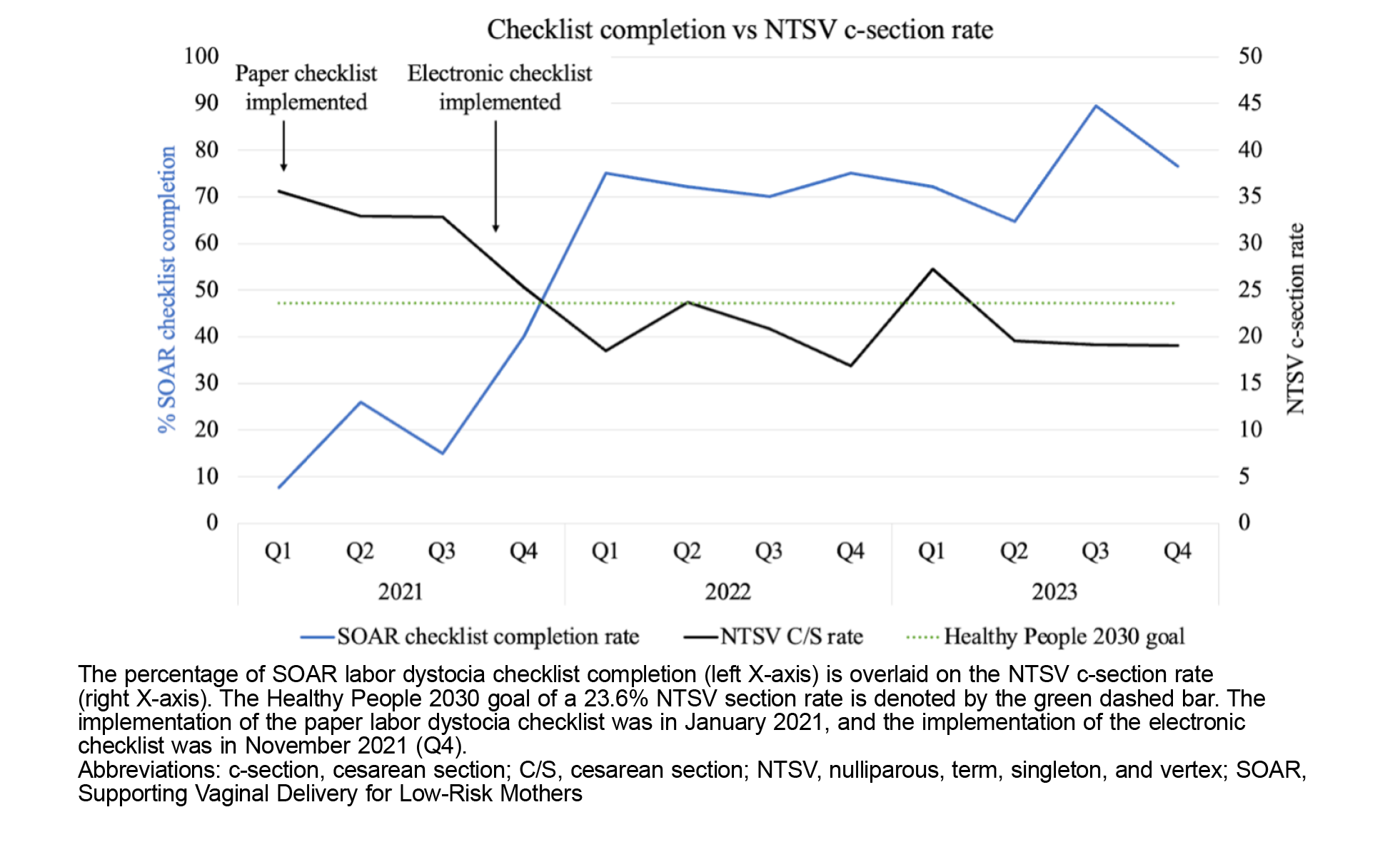
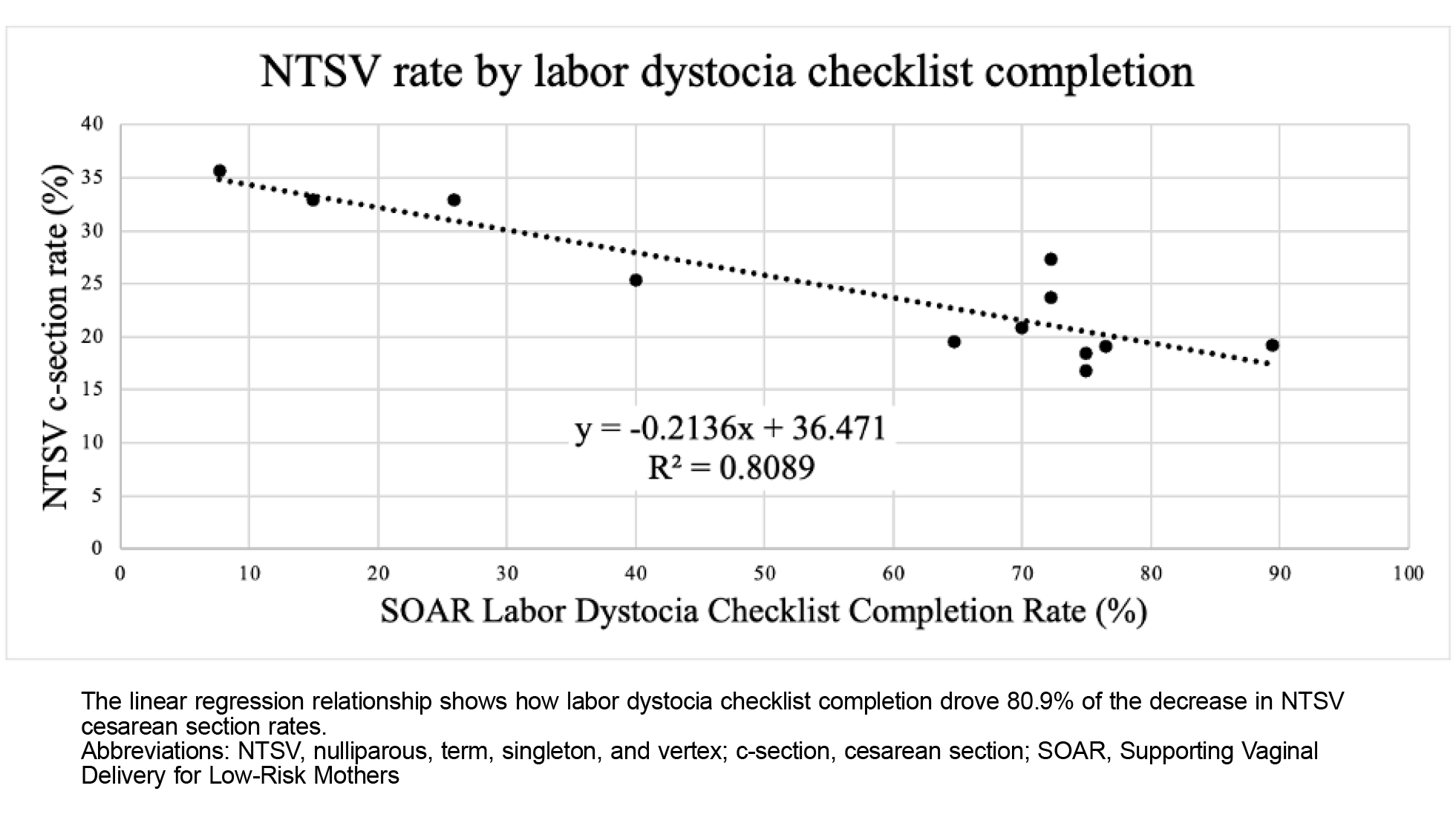
Between 2021 and 2023, the labor dystocia checklist completion rates were shown to be inversely correlated with NTSV c-section reduction rates over time (Figure 2). Linear regression analysis demonstrated that for every 10% increase in labor dystocia checklist completion, the NTSV c-section rate decreased by 2.1% (significance F of 0.00081; Figure 3).
Interestingly, in 2023 when checklist completion was at its highest, NTSV c-section rates were lower for patients on public insurance (17.65%) or no insurance (18.42%) compared to those with private insurance (29.76%) among all provider groups combined, which also held true within each group independently. Further investigation is needed to understand the impact other social determinants of health have on c-section rates.
These data demonstrate that implementing a labor dystocia checklist successfully decreased NTSV c-section rates in a medium to high volume suburban medical center. Before joining the CPCQC SOAR initiative, the NTSV c-section rate at NCMC in 2020 was 35.6% with wide variation in the NTSV rate from month to month. NCMC did not have a system for regular NTSV data review, and NTSV quality measures were not being met.
When enrolled in the CPCQC SOAR initiative, NCMC first implemented a printed labor dystocia checklist and instructed staff to complete it for every NTSV labor. As demonstrated in Figure 2, completion of the checklist initially was relatively limited because the first iteration required printing, manual completion, and then data entry. In November 2021, the resident-driven team incorporated the checklist into the electronic medical record (EMR), which increased rates of completion due to ease of use. The labor dystocia checklist served as a clinical decision-making and data-collection tool to support quality improvement efforts. Blinded provider rates were shared at quarterly provider meetings.
An unintended positive secondary outcome was resident, physician, and nursing satisfaction with the checklist. Subjectively, when discussing the effectiveness of the labor dystocia checklist, family medicine residents commented on the benefit of creating a standardized approach to discuss and diagnose labor dystocia, which led to improved team communication (among attending, chief, intern, primary RN, and charge RN) about the indication for an NTSV c-section and improved rapport at care conferences with the shared goal of a safe and healthy delivery. The nursing staff also commented on the improved communication between nurses and physicians, including during care conferences and postdelivery debriefs, which allowed teams to identify workflow gaps. Physicians who were initially hesitant about the checklist have begun implementing it as a teaching tool retrospectively in didactics and morbidity and mortality conferences.
Replication Processes
Teams interested in replicating this process can obtain the labor dystocia checklist at https://cpcqc.org/wp-content/uploads/2024/04/CPCQC-Labor-Dystocia_2023_24.pdf and the EMR integration template at https://cpcqc.org/wp-content/uploads/2024/05/SOAR-labor-dystocia-EMR-Template-.pdf, and are encouraged to include a summary of checklist conclusions in the patient’s record for those who proceed with a primary c-section. Unit champions should be identified to lead quality improvement processes, and nurses and providers should be educated on the usefulness of team huddles before c-sections. For teams interested in reviewing their data, we recommend that you appoint an auditor to review each primary c-section, export the EMR checklist, and create a document with delivering provider name, clinic, checklist completion, patient age, payor information, and race/ethnicity.
This pilot study was limited to one regional medical center and therefore relies on relatively low birth volumes. Implementation of the checklist was initially difficult, and data collection processes were limited and especially burdensome during the COVID-19 pandemic. Other confounding factors may have affected NTSV c-section rates, such as variability in patient health, provider discretion, and hospital policy changes; these factors were outside the scope of this analysis. During the study period (in November 2021), the checklist was integrated into the EMR system, which allowed providers to easily complete it, reducing any potential risk to patient care.
Next Steps
Now that overall NTSV c-section rates are reduced, NCMC is (a) working to understand whether sociodemographic factors of each patient impact NTSV c-section rates; (b) implementing multidisciplinary review to better understand indications for NTSV c-section; (c) continuing targeted education on the value of checklist completion, especially for those who remain hesitant; and (d) amending the checklist to allow two indications to be chosen simultaneously with added commentary.
This study showed that NTSV c-sections can be reduced when strategies are specific to the needs of each hospital and aimed at improving outcomes through a standardized and patient-centered approach. At NCMC, the implementation of the labor dystocia checklist drove 80.9% of the reduction of NTSV c-sections, from an NTSV rate of 35.6% in 2020 to remaining below the Healthy People 2030 goal of 23.6% at an average of 19% in 2023. Incorporation of a labor dystocia checklist may be useful for teams to decrease their NTSV c-section rates below the Healthy People 2023 goal of 23.6%, especially for teams with residents or trainees.
Acknowledgments
The authors thank their many collaborators and supporters of this work, Dr Karlie Urbach, Dr Casey Weiser, Dr Garrett Mayo, and Dr Drake Sisneros, for their implementation of this project and their continued investment of time and energy to decrease NTSV c-section rates, and Ms Katie Breen for her editing and guidance.
References
-
O’Driscoll K, Foley M, MacDonald D. Active management of labor as an alternative to cesarean section for dystocia. Obstet Gynecol. 1984;63(4):485-490
-
Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014.
PLOS One. 2016;11(2):e0148343.
doi:10.1371/journal.pone.0148343
-
Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal–Fetal Medicine. Safe prevention of the primary cesarean delivery.
Am J Obstet Gynecol. 2014;210(3):179-193.
doi:10.1016/j.ajog.2014.01.026
-
Negrini R, da Silva Ferreira RD, Guimarães DZ. Value-based care in obstetrics: comparison between vaginal birth and caesarean section.
BMC Pregnancy Childbirth. 2021;21(1):333.
doi:10.1186/s12884-021-03798-2
-
Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits?
Am J Perinatol. 2012;29(1):7-18.
doi:10.1055/s-0031-1285829
-
Souza JP, Gülmezoglu A, Lumbiganon P, et al; WHO Global Survey on Maternal and Perinatal Health Research Group. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health.
BMC Med. 2010;8(1):71.
doi:10.1186/1741-7015-8-71
-
Debbink MP, Ugwu LG, Grobman WA, et al; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal–Fetal Medicine Units (MFMU) Network. Racial and ethnic inequities in cesarean birth and maternal morbidity in a low-risk, nulliparous cohort.
Obstet Gynecol. 2022;139(1):73-82.
doi:10.1097/AOG.0000000000004620
-
-
Sinclair LB, Fox MH, Jonas BS, et al. Considering disability and health: reflections on the
Healthy People 2020 Midcourse Review. Disabil Health J. 2018;11(3):333-338.
doi:10.1016/j.dhjo.2018.04.001



There are no comments for this article.