Background and Objectives: Musculoskeletal (MSK) complaints comprise more than 20% of all visits to health care providers each year. Despite required experiences in MSK care, family physicians report low confidence in diagnosing and treating MSK conditions. The purpose of this study was to analyze the effects of early and longitudinal exposure to MSK education on residents’ confidence in and likelihood of performing MSK physical exams and injections in future practice.
Methods: From 2017 to 2019, residents completed an annual survey assessing confidence in, frequency of, and future intentions to perform exams and injections for MSK conditions. We compared responses between family medicine residents who completed a 176-hour longitudinal sports medicine (LSM) curriculum distributed over all 3 years of residency and a comparable cohort of family medicine residents who completed a 188-hour concentrated MSK curriculum primarily in the final year of residency. We made comparisons using the Fisher exact test for categorical variables and an independent samples t test for numeric variables.
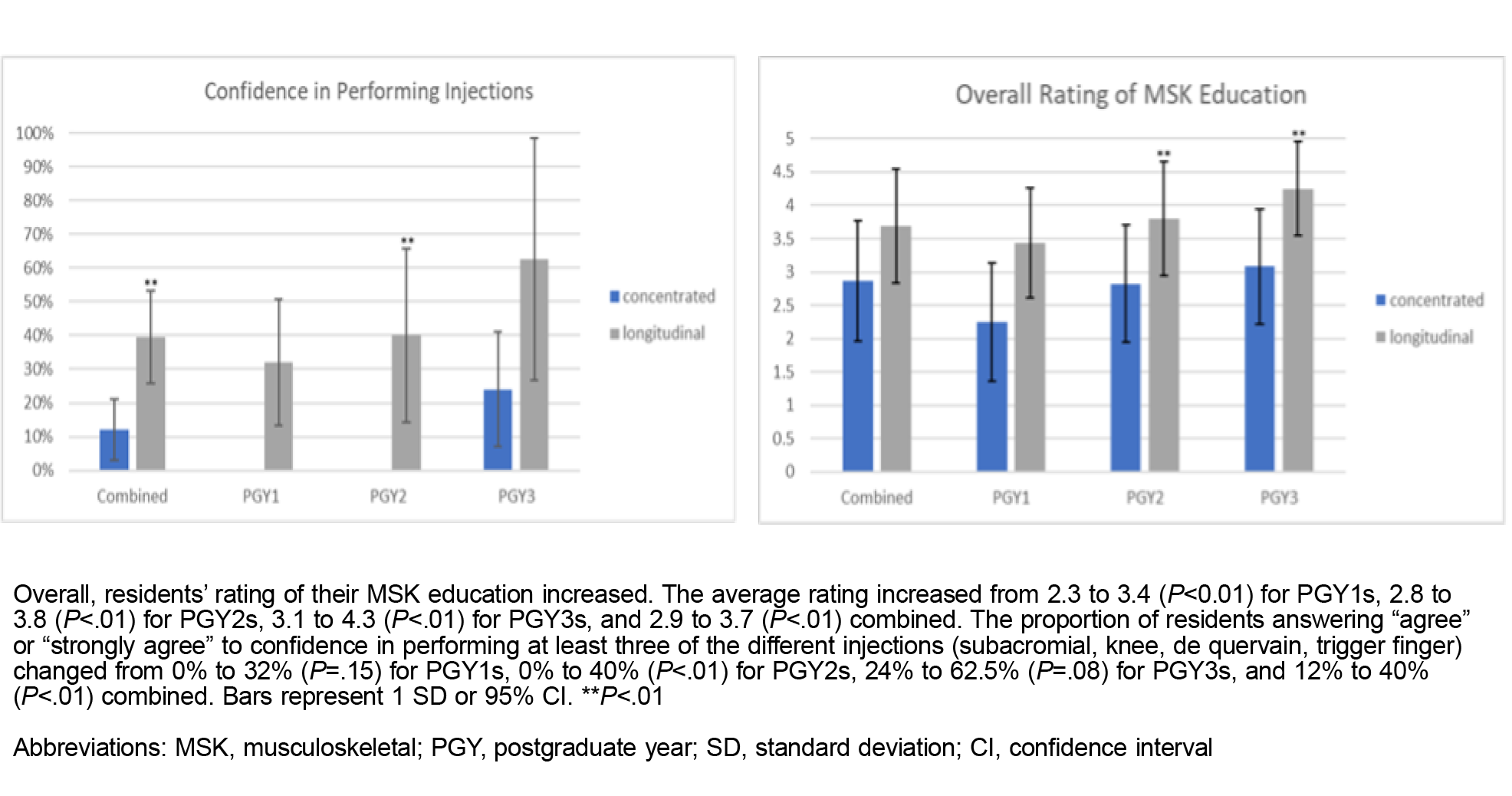
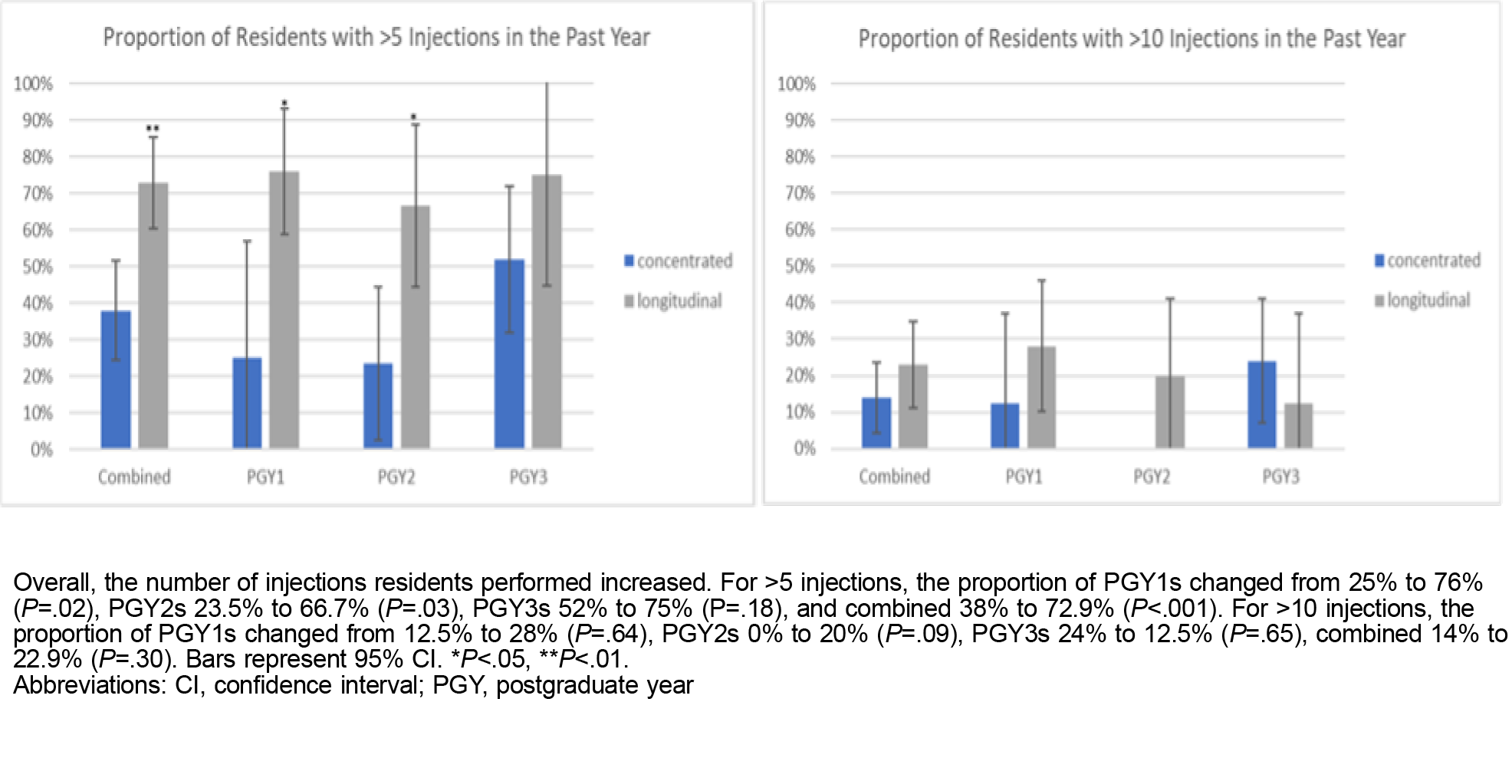
Results: We analyzed the 98 total responses from 50 residents. The proportion of residents reporting high ratings of their residency MSK education (26% to 60%), performing >5 injections (38% to 73%), reporting confidence in performing injections (12% to 40%), and indicating likelihood to perform MSK injections in the future (52% to 65%) were all greater in the LSM versus concentrated MSK curriculum cohorts (P<.05 for all).
Conclusions: Early and longitudinal exposure to MSK care and sports medicine in family medicine residency led to both an increase in MSK injections during residency training and a greater desire to perform these injections in postresidency practice.
Musculoskeletal (MSK) complaints comprise over 20% of health care visits each year, and more than 50% of adults in the United States suffer from MSK conditions. 1, 2 Notably, MSK conditions are the second leading cause of disability. 3 As the US population ages, more patients will be seeking care for MSK complaints. 1, 4 Thus, receiving comprehensive training to assess and manage MSK issues is imperative for family medicine residents.
Incoming residents often have inadequate MSK training, as nearly 80% of family medicine residency program directors surveyed perceived them as deficient in MSK skills.2, 5-7 This inadequate training likely contributes to family physicians reporting diminished confidence in diagnosing and treating MSK conditions, despite training programs meeting the American Board of Family Medicine requirements. 7,-12
Literature has demonstrated that longitudinal curricula and sequenced and stepped approaches that provide multiple opportunities for effective feedback facilitate the acquisition of new skills.13-18 In 2017, the University of California, Irvine, family medicine residency program transitioned from a predominantly postgraduate year (PGY) 3 focused MSK curriculum to a longitudinally integrated approach spanning the entire 3-year residency period. This adjustment aimed to expose residents to MSK medicine earlier and repeatedly to improve confidence in diagnosing and managing MSK complaints, especially with injections.
Curricular Changes
The concentrated curriculum prior to 2017 allocated 20 clinical hours in PGY1 and 168 in PGY3 (188 total clinical hours) to MSK medicine, with an additional 12 hours per year for MSK didactics. In 2017, a longitudinal sports medicine (LSM) curriculum was implemented with 24 clinical hours in PGY1 and 76 each in PGY2 and PGY3 (176 total clinical hours) and 16 hours per year for MSK didactics. An additional board-certified sports medicine physician also joined the faculty in 2017, increasing the total from one to two.
Data Collection
Between 2017 and 2020, 50 family medicine residents completed a total of four annual surveys evaluating their perceptions of the quality of their MSK education, as well as confidence levels, frequency of practice, and future intentions regarding MSK examinations and injections. Resident procedure logs were not accessible due to multiple changes in collection methods throughout the study period. We studied subacromial, knee, de quervain, and trigger finger injections because they are among the most commonly performed and high-yield injections, and were the most commonly performed in the program. 16, 19 The LSM cohort started with the class of 2020 because that was the first class to have experienced this curricular change. This study was approved by the University of California, Irvine, Institutional Review Board.
Statistical Analysis
We summarized Likert scale responses as the percentage responding “agree” or “strongly agree” to each item. For all percentages, we computed 95% confidence intervals. We compared the proportion of participants responding “yes” or “agree/strongly agree” to each item between the LSM and concentrated curriculum cohorts using the Fisher exact test. We compared mean satisfaction with the training between the two cohorts using independent samples t tests. We repeated all comparisons within each year of training (PGY1, PGY2, and PGY3) and for all years combined.
We analyzed a total of 98 responses, with 50 before and 48 after the introduction of the LSM. Responses were evenly distributed across training levels, with 33 from PGY1s, 32 from PGY2s, and 33 from PGY3s (Table 1).
|
|
Number of responses
|
|
Year
|
Concentrated curriculum
|
Longitudinal sports medicine
|
Total
|
|
PGY1
|
8
|
25
|
33
|
|
PGY2
|
17
|
15
|
32
|
|
PGY3
|
25
|
8
|
33
|
|
Total
|
50
|
48
|
98
|
|
|
All residents
|
|
Rating
|
Concentrated curriculum % (95% CI)
|
Longitudinal sports medicine (SM) % (95% CI)
|
P
|
|
Confidence
|
|
Confidence in the ability to perform exam of the shoulder
|
70.0 (57.3, 82.7)
|
68.8 (55.6, 81.9)
|
.99
|
|
Confidence in the ability to perform exam of the knee
|
78.0 (66.5, 89.5)
|
81.3 (70.2, 92.3)
|
.80
|
|
Confidence in performing subacromial injections (% agree/strongly agree)
|
28.0 (15.6, 40.4)
|
35.4 (21.9, 48.9)
|
.52
|
|
Confidence in performing knee injections (% agree/strongly agree)
|
66.0 (52.9, 79.1)
|
91.7 (83.8, 99.5)
|
.003
|
|
Confidence in performing de quervain tenosynovitis injections (% agree/strongly agree)
|
14.0 (4.4, 23.6)
|
31.3 (18.1, 44.4)
|
.053
|
|
Confidence in performing trigger finger injections (% agree/strongly agree)
|
16.0 (5.8, 26.2)
|
58.3 (44.4, 72.3)
|
<.001
|
|
Frequency of practice
|
|
Percentage reporting >5 injections in the past year
|
38.0 (24.5, 51.5)
|
72.9 (60.3, 85.5)
|
<.001
|
|
Percentage reporting >10 injections in the past year
|
14.0 (4.4, 23.6)
|
22.9 (11.0, 34.8)
|
.30
|
|
Percentage reporting 1 or more subacromial injections in the past year
|
54.0 (40.2, 67.8)
|
68.8 (55.6, 81.9)
|
.151
|
|
Percentage reporting 1 or more knee injections in the past year
|
84.0 (73.8, 94.2)
|
100.0 (100.0, 100.0)
|
.006
|
|
Percentage reporting 1 or more de quervain tenosynovitis injections in the past year
|
24.0 (12.2, 35.8)
|
47.9 (33.8, 62.0)
|
.020
|
|
Percentage reporting 1 or more trigger finger injections in the past year
|
46.0 (32.2, 59.8)
|
81.3 (70.2, 92.3)
|
<.001
|
|
Future intentions
|
|
Likely to perform subacromial injections as a part of your future practice (% agree/strongly agree)
|
58.0 (44.3, 71.7)
|
66.7 (53.3, 80.0)
|
.41
|
|
Likely to perform knee injections as a part of your future practice (% agree/strongly agree)
|
76.0 (64.2, 87.8)
|
95.8 (90.2, 100.0)
|
.008
|
|
Likely to perform de quervains injections as a part of your future practice (% agree/strongly agree)
|
50.0 (36.1, 63.9)
|
62.5 (48.8, 76.2)
|
.23
|
|
Likely to perform trigger finger injections as a part of your future practice (% agree/strongly agree)
|
54.0 (40.2, 67.8)
|
75.0 (62.8, 87.3)
|
.036
|
|
Quality of training
|
|
Rate overall quality of resident MSK education thus far (out of 5), mean (SD).
|
2.9 (0.9)
|
3.7 (0.9)
|
<.001
|
Aggregate responses are presented in Table 1. Overall, we found no difference in residents’ confidence in performing physical exams of the shoulder (70% to 69%, P=.99) or knee (78% to 81%, P=.80). However, we identified an increase in the proportion of residents reporting confidence in performing injections, with knee (66% to 92%, P=.003) and trigger finger (16% to 58%, P<.001) injections being statistically significant. Residents also reported performing more injections in the LSM, with the proportion of residents performing at least one de quervain (24% to 48%, P=.020) or trigger finger (46% to 81%, P<.001) injection almost doubling. We also found increases in the proportion of residents who anticipated incorporating injections into their future practice, with both knee (76% to 96%, P=.008) and trigger finger (54% to 75%, P=.036) injections being statistically significant.
Under the LSM, the proportion of residents characterizing their MSK education as “very good” or “excellent” increased significantly from 26% to 60% (P<.05), with the subset endorsing “excellent” increasing from 2% to 17% (P<.05). Moreover, the average rating of their MSK education improved from 2.86 to 3.69 (P<.05, Figure 1). Additionally, we found a notable increase in the percentage of residents expressing confidence in their ability to administer injections, increasing from 12% to 40% (P<.05; Figure 1). Furthermore, although not statistically significant (P=.23), we identified an increase in the percentage of residents indicating a likelihood to incorporate injections into their future practice, rising from 52% to 65%.
The overall percentage of residents reporting performing at least 5 injections in the preceding year increased significantly from 38% to 73% (P<.05; Figure 2). While the proportion of residents performing a minimum of 10 injections rose from 14% to 23%, this increase was not statistically significant in the aggregate (Figure 2).
DISCUSSION AND CONCLUSIONS
This study underscores the efficacy of a longitudinal MSK curriculum in bolstering residents’ confidence in and perception of their MSK training. This enhanced perception is further validated by the increased proportion of residents expressing an inclination to incorporate injections into their future practices. Furthermore, these enhancements emerged even with a 10% reduction in training hours despite previous studies focusing on incorporating additional dedicated experiences. 11, 16, 20-23
In the LSM, residents engaged in multiple rotations across their 3-year residency, offering ample opportunities to practice MSK exams and injections while receiving constructive feedback. Furthermore, the condensed intervals between learning opportunities likely promoted enhanced consolidation and skill refinement. Moreover, whereas resident exposure in the concentrated curriculum scheduling could be affected by variations such as holidays or vacations overlapping with MSK rotations, such impacts were minimized in the LSM due to a more even rotation distribution.
These findings are significant because programs could potentially reallocate hours to other essential training areas by creating a longitudinal curriculum focused on increasing the number of exposures residents have to MSK medicine with even a decrease in the number of hours.
Limitations of this study include the sample size and reliance on self-reported experiences and confidence levels. The study did not include objective data on performance ratings or follow-up postgraduation. Additionally, we found a lack of significant improvement in exam skills, which may indicate that knowing how and why to perform a procedure are separate skill sets; this should be further explored. Also, some confounding was due to the addition of a second sports faculty member and increase in didactic hours, which were not directly assessed, although qualitatively residents reported the hours change as a significant improvement.
Future studies should measure the sustainability and long-term impact of such curricular changes. Additionally, objective data, such as performance ratings and patient outcomes, should be measured.
This study reveals that a longitudinal curriculum, providing residents with ample opportunities to learn and practice MSK medicine, significantly enhances their confidence in handling these conditions, including incorporating injections in their future practice, even amid an overall reduction in dedicated teaching hours. Strengthening the confidence of family physicians in diagnosing and treating MSK conditions is crucial for fostering a health system that is more effective and efficient, benefiting both payers and patients.
References
-
United States Bone and Joint Initiative.
The Burden of Musculoskeletal Diseases in the United States (BMUS). 4th ed. USBJI; 2016. Accessed on July 12, 2023.
http://www.boneandjointburden.org
-
Lynch TS, Hellwinkel JE, Jobin CM, Levine WN. Curriculum reform and new technology to fill the void of musculoskeletal education in medical school curriculum.
J Am Acad Orthop Surg. 2020;28(23):945-952.
doi:10.5435/JAAOS-D-20-00485
-
-
March L, Smith EU, Hoy DG, et al. Burden of disability due to musculoskeletal (MSK) disorders.
Best Pract Res Clin Rheumatol. 2014;28(3):353-366.
doi:10.1016/j.berh.2014.08.002
-
DiGiovanni BF, Sundem LT, Southgate RD, Lambert DR. Musculoskeletal medicine Is underrepresented in the American medical school clinical curriculum.
Clin Orthop Relat Res. 2016;474(4):901-907.
doi:10.1007/s11999-015-4511-7
-
Petravick ME, Marsh JL, Karam MD, Dirschl DR. A survey on recent medical school graduate comfort with the level 1 milestones.
J Surg Educ. 2018;75(4):911-917.
doi:10.1016/j.jsurg.2017.10.004
-
Wu V, Goto K, Carek S, et al. Family medicine musculoskeletal medicine education: a CERA study.
Fam Med. 2022;54(5):369-375.
doi:10.22454/FamMed.2022.975755
-
Amoako AO, Amoako AB, Pujalte GG. Family medicine residents’ perceived level of comfort in treating common sports injuries across residency programs in the United States.
Open Access J Sports Med. 2015;6:81-86.
doi:10.2147/OAJSM.S71457
-
Lynch JR, Schmale GA, Schaad DC, Leopold SS. Important demographic variables impact the musculoskeletal knowledge and confidence of academic primary care physicians.
J Bone Joint Surg Am. 2006;88(7):1,589-1,595.
doi:10.2106/JBJS.E.01365
-
Matzkin E, Smith EL, Freccero D, Richardson AB. Adequacy of education in musculoskeletal medicine.
J Bone Joint Surg Am. 2005;87(2):310-314.
doi:10.2106/JBJS.D.01779
-
Ladurner A, Nijman T, Gill TK, Smitham PJ. The impact of a hands-on arthrocentesis workshop in undergraduate medical education.
BMC Med Educ. 2020;20(1):260.
doi:10.1186/s12909-020-02174-6
-
Matheny JM, Brinker MR, Elliott MN, Blake R, Rowane MP. Confidence of graduating family practice residents in their management of musculoskeletal conditions. Am J Orthop. 2000;29(12):945-952.
-
Pohl SD, Van Hala S, Ose D, Tingey B, Leiser JP. A longitudinal curriculum for quality improvement, leadership experience, and scholarship in a family medicine residency program.
Fam Med. 2020;52(8):570-575.
doi:10.22454/FamMed.2020.679626
-
Rowat J, Johnson K, Antes L, White K, Rosenbaum M, Suneja M. Successful implementation of a longitudinal skill-based teaching curriculum for residents.
BMC Med Educ. 2021;21(1):346.
doi:10.1186/s12909-021-02765-x
-
Kelm DJ, Ratelle JT, Azeem N, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents.
J Grad Med Educ. 2015;7(3):454-457.
doi:10.4300/JGME-14-00284.1
-
Bakewell CJ, Gardner GC. A survey of arthrocentesis and soft-tissue injection procedures performed in primary care practice: effect of resident training and using data to shape curriculum.
J Rheumatol. 2011;38(9):1,986-1,989.
doi:10.3899/jrheum.110041
-
Burgess A, van Diggele C, Roberts C, Mellis C. Tips for teaching procedural skills.
BMC Med Educ. 2020;20(Suppl 2):458.
doi:10.1186/s12909-020-02284-1
-
Routt E, Mansouri Y, de Moll EH, Bernstein DM, Bernardo SG, Levitt J. Teaching the simple suture to medical students for long-term retention of skill.
JAMA Dermatol. 2015;151(7):761-765.
doi:10.1001/jamadermatol.2015.118
-
-
Ferderber ML, Adams A, Urbanek CW, Cummings DM. Musculoskeletal injections performed by family medicine residents participating in a clinical sports medicine track.
Fam Med. 2022;54(6):452-455.
doi:10.22454/FamMed.2022.626280
-
Kwiatkowski A, Shakoor N, Manadan A, Block JA, Khandelwal S. Incorporating interactive workshops into bedside teaching: completion of a multi-modal rheumatology rotation significantly increases internal medicine residents’ competency and comfort with comprehensive knee examinations.
BMC Med Educ. 2022;22(1):355.
doi:10.1186/s12909-022-03425-4
-
Perrig M, Berendonk C, Rogausch A, Beyeler C. Sustained impact of a short small group course with systematic feedback in addition to regular clinical clerkship activities on musculoskeletal examination skills—a controlled study.
BMC Med Educ. 2016;16:35.
doi:10.1186/s12909-016-0554-z
-
McDaniel CM, Forlenza EM, Kessler MW. Effect of shortened preclinical curriculum on medical student musculoskeletal knowledge and confidence: an institutional survey.
J Surg Educ. 2020;77(6):1,414-1,421.
doi:10.1016/j.jsurg.2020.04.011



There are no comments for this article.