Background and Objectives: The proportion of family physicians caring for children is decreasing. At the same time, US family medicine residency training requirements have increased flexibility in how to train future family physicians in caring for this population. Our objective was to evaluate the correlation between residency program structures and curriculum with graduates caring for children.
Methods: We conducted a prospective cohort study of family medicine graduates using the 2018 Council of Academic Family Medicine Education Research Alliance program director study to measure program characteristics and pediatric curricular elements, and the 2021 family medicine National Graduate Survey (NGS) of residents who graduated in 2018 to measure outcomes. We used logistic regression to determine associations between residency elements and graduate practice of outpatient pediatrics, inpatients pediatrics, or newborn hospital care.
Results: After data from the two sources were merged, our final sample was 779 family medicine graduates (48% of the NGS sample), where 74.7% reported practicing outpatient pediatrics, 16.8% inpatient pediatrics, and 25.9% newborn care. In multivariate analyses, residency processes associated with the care of children in one or more settings included having more than 10% of continuity clinic patients under the age of 10 and having two or more family medicine faculty supervising inpatient pediatrics or newborn care.
Conclusions: In a large national cohort study, we found that residency processes—especially faculty role modeling care of children and the inclusion of children in continuity clinic—are positively associated with residency graduates providing care for children. With residency training requirements changing, these results offer evidence-based interventions for programs to produce graduates who will care for children.
Despite having the historically broadest scope among medical specialties, 1- 3 the proportion of family physicians providing care to children is declining in the United States. 4, 5 This trend has significant implications for equitable access to health care delivery for one of the most vulnerable populations, children, at a time when infant mortality is on the rise 6 and receipt of child preventive services like vaccines, historically delivered in primary care, is falling. 7, 8 In fact, between 2012 and 2021, children without a usual source of primary care rose by 36%. 9 This trend progresses, despite high levels of declared intention of most graduating family physicians to care for children in their eventual practice. 10, 11
The new Accreditation Council for Graduate Medical Education (ACGME) family medicine training requirements offer increased flexibility in residency training requirements for pediatric care. 12 The requirements broadened the age range defining pediatric patients in continuity practice from under 10 to under 18 while keeping the minimum percentage at 10%, effectively reducing the requirements for experience caring for young children in continuity practice. The new requirements also reduced the minimum required time rotating on inpatient pediatrics and removed the requirement that at least one family medicine faculty member sees newborns or children in a hospital setting. And while factors such as younger age, female gender, and rural practice location have been associated with the likelihood of including care of children in actual practice, 13 we know far less about how structural and curricular elements of family medicine residency programs influence, impact, and interact with demographic and geographic factors in training.
If educators, leaders, and funders of graduate medical education are to effectively address growing deficiencies in access to pediatric primary care, we critically need to understand how such elements in family medicine residency training correlate with downstream graduate care of children, both outpatient and inpatient. Historically, linking residency program characteristics and graduate clinical behaviors in practice, specifically their engagement in pediatric care, has been difficult. To overcome this challenge, in 2018, the Family Medicine Residency Outcomes Project (FM-ROP) was created to leverage and combine the data sources required to inform associations between residency training and downstream practice. 14 In this study, our objective was to determine whether residency training structure and curricular elements are associated with graduates caring for children in practice.
Setting and Participants
This prospective cohort study followed the 2018 family medicine residency graduates into practice until they completed the 2021 National Graduate Survey (NGS). To most accurately collect the exposures that these graduates experienced during their residency, we chose to collect exposures not from the graduates themselves (who may not be fully aware of the specific structural or curricular aspects of their training programs) but from their program directors (who may be better reporters of these exposures) through a Council of Academic Family Medicine Educational Research Alliance (CERA) program director study. 15, 16
The sampling frame for the CERA survey was the 586 ACGME-accredited US family medicine residency program directors as identified by the Association of Family Medicine Residency Directors in the summer of 2018. CERA conducted a special omnibus survey where program directors were asked to identify their program using their ACGME identification number, and the questions were asked about the program over the last 3 years (during the time the class of 2018 was in the residency). The CERA survey questions and deidentified results are available on the CERA website. 17
The NGS is administered to American Board of Family Medicine (ABFM) diplomates 3 years after residency graduation. 18, 19 The 2021 survey opened in January 2021 and was originally set to close in December, but it was kept open through June 2022 due to an ABFM programmatic change in response to the COVID-19 pandemic. Resident demographics were gathered from ABFM administrative databases. Race was self-reported by the resident during registration for the 2018 ABFM initial certification examination in response to a “select best” question and is reported here as is, except Native American/Alaska Native and Native Hawaiian or Other Pacific Islander were combined into an Indigenous category due to the small sample size. The 2021 NGS questions and aggregate results are available on the ABFM website. 20 Our primary outcomes of interest—whether the family medicine graduate cared for children in practice—were measured on the NGS. We measured care of children in three settings based on self-reported practice of each by the graduate: outpatient pediatric care, inpatient pediatric care, and newborn care. The exposures of interest were measured on the CERA survey and included program structures and curricular processes. Program structures included the region of the program (Q12), type of community served by the program (urban, urban/suburban, rural; Q14), size of the program (Q16), program type (university, community-university affiliated, community-unaffiliated, military; Q11), program accreditation type (Q20-21), and presence of other training programs (and specifically pediatrics; Q26-27). Program curricular processes included number of faculty practicing inpatient pediatrics or newborn care (Q30), months of pediatrics rotations (Q28), and whether residents had more than 10% of continuity visits with children younger than 10 years old (the ACGME pediatric continuity visit requirement at the time; Q34). Graduate demographics (age, gender, degree type, whether graduated from an international medical school, race/ethnicity) were obtained from the ABFM administrative databases. Practice information on the NGS included practice region and county-level practice rurality using the Rural-Urban Continuum Codes.
For the CERA variables concerning the number of supervising attendings, length of time on various services, and panel makeup, the ACGME requirements (which also were consistent with the natural distribution of responses) were used when choosing the cut points for a binomial variable.
The program director responses in the 2018 CERA survey were merged by ABFM research staff, with the residency graduate responses on the NGS using the ACGME program identification number. The unit of analysis was the residency graduate. The final FM-ROP dataset contained all respondents to the NGS who graduated from a residency program where the program director responded to the CERA survey. 14
Analysis
First, we described our data. Then we conducted bivariate analyses, which were performed with a false discovery rate post hoc test to determine baseline significance. Variables significant in bivariate analysis were included in the multiple logistic regression analyses. In addition, sample size was taken into consideration to prioritize quantitative power for some variables. We did not include the presence of a pediatric residency due to low response rate for this item; instead, we used whether a program was at a single-sponsor institution because this was an a priori hypothesis, and we conducted a separate logistic regression analysis for pediatric continuity volume due to its low response rate. We conducted three separate multiple logistic regressions to determine independent associations between graduate characteristics and residency curricula and structure with our main outcomes: practicing outpatient pediatrics, inpatient pediatrics, and newborn care. In these primary analyses, exposure to pediatric continuity volume in residency was excluded due to low response rate to this item on the CERA survey. We performed a secondary logistic regression analysis for each outcome that included pediatric continuity volume in residency, including only the variables that were statistically significant in the corresponding primary analysis. We used SAS version 9.4 (SAS Institute) for all analyses. The overall project was approved by the American Academy of Family Physicians Institutional Review Board.
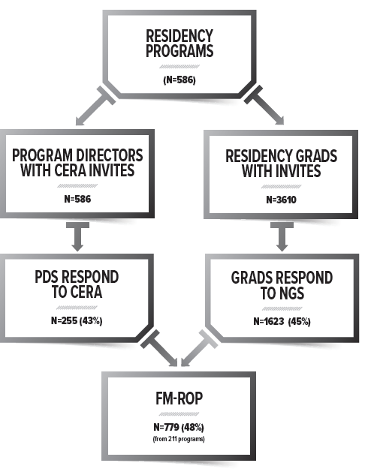
The response rate for the 2018 CERA survey was 43.7% (255/586). The response rate for the 2021 NGS survey was 45.0% (1,623/3,610). After merging the two datasets, we lost 44 programs due to no residents responding to the survey and 844 residents due to their program director not responding. Our final analytic sample included 779 graduates from 211 residencies (Figure 1).
Among our analytic cohort, 74.7% reported practicing outpatient pediatrics, 16.8% inpatient pediatrics, and 25.9% newborn hospital care (Table 1). Graduate characteristics positively associated with caring for children in all settings included practicing in a rural area, being a US medical graduate, and practicing in the Midwest, while being a woman was associated only with practicing outpatient pediatrics. Program characteristics positively associated with caring for children in the outpatient setting and for newborns included training in the Midwest, caring for children in the inpatient setting, and rural residency training (Table 1). Having a pediatric continuity care volume with young patients (<10 yrs old) was associated with caring for children in all settings; and having at least two faculty members practicing inpatient pediatrics or newborn care was associated with caring for children in outpatient and newborn settings. The amount of time spent on pediatric rotations did not have a significant impact (Table 2).
|
|
Total
|
Practicing outpatient pediatrics
|
Outpatient P values
|
Practicing inpatient pediatrics
|
Inpatient
P values
|
Practicing newborn care
|
Newborn P values
|
|
|
N=779
n (%)
|
N=580
n (%)
|
|
N=131
n (%)
|
|
N=202
n (%)
|
|
|
Graduate demographics
|
|
|
|
|
|
|
|
|
Age: mean (range) {SD}
|
34.8 (29,61) {3.9}
|
34.5 (29,61) {3.5}
|
.0334*
|
34.5 (31,46) {2.95}
|
.3418
|
34.4 (30,46) {2.9}
|
.1060
|
|
Gender (% female)
|
406 (57.2)
|
317 (59.7)
|
.0344*
|
62 (53.0)
|
.3503
|
111 (60.7)
|
.2307
|
|
Degree (% MD)
|
559 (78.7)
|
410 (77.1)
|
.1058
|
96 (82.1)
|
.2307
|
145 (79.2)
|
.5440
|
|
IMG (% IMG)
|
176 (24.8)
|
106 (20.0)
|
<.0001*
|
20 (17.1)*
|
.0989
|
28 (15.3)*
|
.0031*
|
|
Race
|
|
|
.0344*
|
|
.0273*
|
|
.0031*
|
|
White
|
480 (67.6)
|
370 (69.7)
|
|
89 (76.1)*
|
|
137 (74.9)*
|
|
|
Black
|
62 (8.7)
|
39 (7.3)
|
|
8 (6.8)
|
|
12 (5.6)
|
|
|
Asian
|
121 (17.0)
|
83 (15.6)
|
|
9 (7.7)*
|
|
18 (9.8)
|
|
|
Indigenous
|
7 (1.0)
|
7 (1.3)
|
|
3 (2.6)
|
|
5 (2.7)
|
|
|
All others
|
40 (5.6)
|
32 (6.0)
|
|
8 (6.8)
|
|
11 (6.0)
|
|
|
Ethnicity
|
|
|
.1964
|
|
.2091
|
|
.0885
|
|
Hispanic
|
73 (10.3)
|
49 (9.2)
|
|
8 (6.8)
|
|
11 (6.0)
|
|
|
Non-Hispanic
|
637 (89.7)
|
482 (90.8)
|
|
109 (93.2)
|
|
172 (94.0)
|
|
|
Practice metropolitan (RUCC rurality)
|
611 (86.1)
|
449 (84.6)
|
.0748
|
79 (67.5)*
|
<.0001*
|
146 (79.8)*
|
.0145*
|
|
Practice region
|
|
|
.0174*
|
|
.2530
|
|
.0067*
|
|
Northeast
|
84 (11.8)
|
60 (11.3)
|
|
10 (8.6)
|
|
17 (9.3)
|
|
|
South
|
200 (28.2)
|
133 (25.1)
|
|
29 (24.8)
|
|
35 (19.1)*
|
|
|
Midwest
|
189 (26.6)
|
154 (29.0)
|
|
40 (34.2)
|
|
64 (35.0)
|
|
|
West
|
237 (33.4)
|
184 (34.7)
|
|
38 (32.5)
|
|
67 (36.6)
|
|
|
Program demographics
|
|
|
|
|
|
|
|
|
Program region
|
|
|
.0406*
|
|
.4428
|
|
.0242*
|
|
Northeast
|
57 (13.6)
|
43 (13.4)*
|
|
7 (9.9)
|
|
12 (11.4)*
|
|
|
South
|
132 (31.5)
|
93 (28.9)
|
|
25 (35.2)
|
|
29 (27.6)
|
|
|
Midwest
|
102 (24.3)
|
86 (26.7)
|
|
21 (29.6)
|
|
31 (29.5)
|
|
|
West
|
128 (30.6)
|
100 (31.1)
|
|
18 (25.4)
|
|
33 (31.4)
|
|
|
Community served
|
|
|
.1228
|
|
.0242*
|
|
.4373
|
|
Inner city
|
96 (22.9)
|
69 (21.4)
|
|
8 (11.3)*
|
|
16 (15.2)
|
|
|
Rural
|
38 (9.1)
|
27 (8.4)
|
|
15 (21.1)
|
|
14 (13.3)
|
|
|
Suburban
|
110 (26.6)
|
83 (25.8)
|
|
19 (26.8)
|
|
29 (27.7)
|
|
|
Urban/suburban
|
175 (41.8)
|
143 (44.1)
|
|
29 (40.9)
|
|
46 (43.8)
|
|
|
|
Total
|
Practicing outpatient pediatrics
|
Outpatient
P values
|
Practicing inpatient pediatrics
|
Inpatient
P values
|
Practicing newborn care
|
Newborn
P values
|
|
|
N=779
n (%)
|
N=580
n (%)
|
|
N=131
n (%)
|
|
N=202
n (%)
|
|
|
Program Demographics
|
|
|
|
|
|
|
|
|
Residency size
|
|
|
.6512
|
|
.7875
|
|
.0838
|
|
<19 residents
|
74 (17.7)
|
57 (17.7)
|
|
11 (15.5)
|
|
11 (10.5)
|
|
|
19–31 residents
|
181 (43.2)
|
139 (43.2)
|
|
30 (42.3)
|
|
45 (42.9)
|
|
|
>31 residents
|
164 (29.1)
|
126 (39.1)
|
|
30 (42.3)
|
|
49 (46.7)
|
|
|
Residency type
|
|
|
.8242
|
|
.3882
|
|
.4373
|
|
University-based
|
248 (59.2)
|
190 (59.0)
|
|
48 (67.6)
|
|
63 (60.0)
|
|
|
Community-based, university-affiliated
|
225 (53.7)
|
174 (54.0)
|
|
45 (63.5)
|
|
58 (55.2)
|
|
|
Community-based, not affiliated
|
23 (5.5)
|
16 (5.0)
|
|
3 (4.2)
|
|
5 (4.8)
|
|
|
Military
|
23 (5.5)
|
16 (5.0)
|
|
7 (9.9)
|
|
11 (10.5)
|
|
|
Primary clinic training site
|
|
|
.6512
|
|
.4843
|
|
.4843
|
|
Hospital-based
|
230 (54.9)
|
184 (57.1)
|
|
40 (56.3)
|
|
64 (61.0)
|
|
|
Nonhospital, nonprofit
|
100 (23.9)
|
80 (24.8)
|
|
15 (21.1)
|
|
20 (19.0)
|
|
|
Nonhospital, for-profit
|
23 (5.5)
|
12 (3.7)
|
|
2 (2.8)
|
|
5 (4.8)
|
|
|
FQHC
|
47 (11.2)
|
32 (9.9)
|
|
8 (11.3)
|
|
9 (8.6)
|
|
|
Military
|
17 (4.1)
|
12 (3.7)
|
|
5 (7.0)
|
|
6 (5.7)
|
|
|
Other
|
2 (0.5)
|
2 (0.6)
|
|
1 (1.4)
|
|
1 (1.0)
|
|
|
Accreditation in 2015
|
|
|
.7875
|
|
.3855
|
|
.7111
|
|
ACGME
|
554 (75.2)
|
411 (76.3)
|
|
102 (82.0)
|
|
146 (76.4)
|
|
|
Dual ACGME/AOA
|
180 (24.4)
|
126 (23.4)
|
|
21 (17.1)
|
|
45 (23.6)
|
|
|
AOA only
|
3 (0.4)
|
2 (0.4)
|
|
-
|
|
-
|
|
|
Presence of a pediatrics residency
|
222 (49.2)
|
165 (49.3)
|
.7558
|
34 (45.9)
|
.6512
|
48 (43.6)
|
.3882
|
|
Single-residency institution (%)
|
273 (37.0)
|
195 (36.1)
|
.4843
|
45 (36.3)
|
.8242
|
79 (41.1)
|
.4373
|
|
|
Total (%)
|
Have >10% of continuity visits with pediatric patients (<10 yrs old), n (%)
|
Have >=4 months total pediatric experience, n (%)
|
Have 2 or more faculty practicing inpatient pediatrics or newborn nursery, n (%)
|
|
Practicing outpatient pediatrics
|
540 (75.8)
|
260 (78.6)
|
326 (76.7)
|
495 (77.3)
|
|
Practicing inpatient pediatrics
|
124 (17.4)
|
72 (21.8)
|
76 (17.9)
|
117 (18.2)
|
|
Practice newborn care
|
192 (27.0)
|
109 (32.9)
|
120 (28.2)
|
184 (28.6)
|
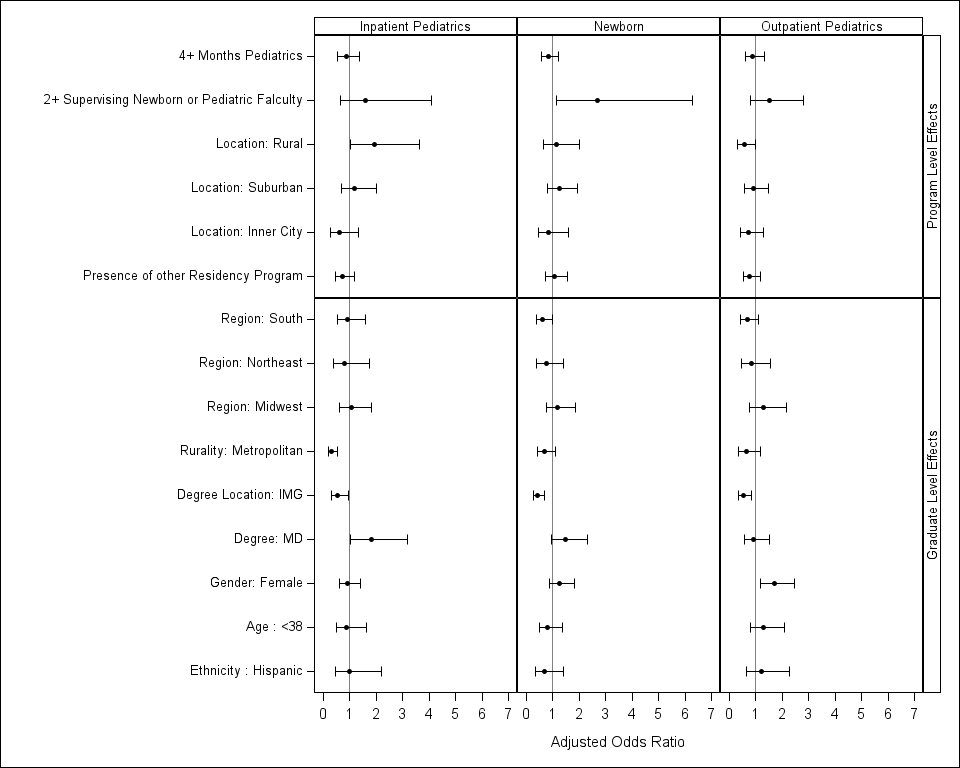
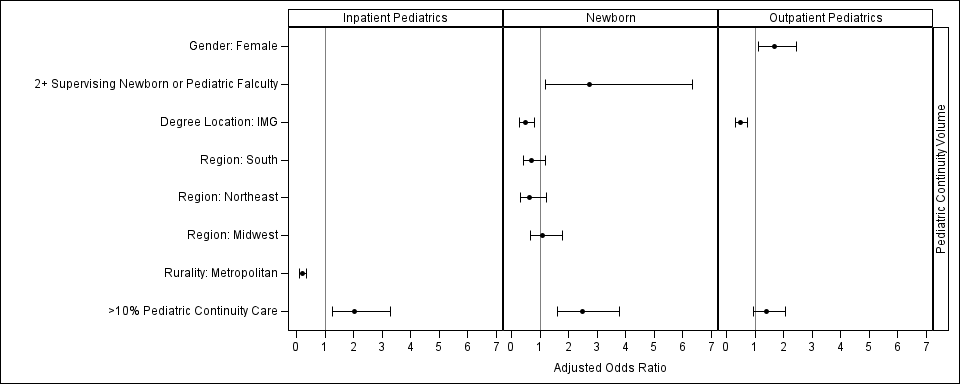
In multivariant analyses (Figure 2), the only personal characteristic positively associated with the care of children was female gender for practicing outpatient pediatrics (OR 1.689 [1.167, 2.449]). Demographics negatively associated included being an international medical graduate for outpatient pediatrics (OR 0.54 [0.347, 0.842]) and newborn care (OR 0.536 [0.293, 0.946]), working in a metropolitan area for inpatient pediatrics (OR 0.309 [0.184, 0.519]), and working in the South for newborn care (OR 0.598 [0.365, 0.98]). Residency processes positively associated with the care of children included having more than 10% of continuity clinic patients under the age of 10 for practicing inpatient pediatrics (OR 2.04 [1.259, 3.305]), and newborn care (OR 2.364 [1.564, 3.572]); in outpatient pediatrics, having a pediatric continuity exposure was not significant (Figure 3 ). Residency program demographics and the number of months of pediatrics in the curriculum were not associated with graduate practice.
DISCUSSION AND CONCLUSIONS
In this large national prospective cohort study of residency outcomes, we found that a quarter of family physicians who graduated from residency in 2018 did not care for children as part of their outpatient scope of practice. Controlling for graduate demographics and practice, we found that residency curriculum and processes were independently associated with graduates being more likely to care for children 3 years after graduation. Specifically, graduates from residencies with a higher percentage of children under the age of 10 in a residency continuity clinic and those with two or more faculty caring for newborns or children in a hospital setting were more likely to care for children. These results confirm that residency curricula can influence graduate practice patterns and offer curricula changes for residencies that wish to either increase or maintain their programs’ contribution to child health.
Those who identify as women, graduate from US medical schools, or are practicing in a rural area are more likely to care for children in the outpatient setting. This is consistent with previous reported demographics of family physicians who care for children. 13 Only a quarter of these family physicians reported caring for newborns and 16% reported caring for children in a hospital setting. Similar to outpatient care of children, graduates of US medical schools are more likely to incorporate newborn and inpatient pediatric care into their practice, and those who practice in rural settings are more likely to care for children in the hospital, also consistent with previous studies. 13 Unlike previous studies, in our multivariable analysis, other demographics, such as age and region of practice, were not significantly related to caring for children. This finding suggests that either other factors such as training experience have more of an effect or that the study was not sufficiently powered to detect a difference.
Program curricula processes that we were able to examine with this study included dedicated instructional time (number of months of dedicated pediatric experience), faculty role modeling (number of family medicine faculty supervising newborn care or inpatient pediatrics), and clinic as the curriculum (% of continuity clinic visit with children <10 yrs old). In univariant analyses, clinic as the curriculum was significantly associated with being more likely to care for children in both outpatient and inpatient settings and caring for newborns. Due to a higher nonresponse rate for this item on the program director survey, this variable was underpowered so could not be included in the full multivariable regression analysis; but when controlled for significant graduate and program demographic variables, it remained a significant predictor of inpatient pediatrics and newborn practice. This continued association with inpatient scope of practice suggests the power of longitudinal continuity care experiences on future clinical practice across settings. In univariant analysis, faculty role modeling of caring for sick and young infants was significantly associated with outpatient care of children and newborn care. Faculty role modeling remained significant for newborn care in the full multivariant model. We found no associations for instructional time (having a higher number of dedicated months of pediatric experience). This finding suggests that time alone in a particular area of practice may not predict clinical competency to practice in the future. This result may be related to the highly variable pediatric experiences during these rotations. As more rural and urban nonteaching hospitals close and more pediatric care is delivered in specialized pediatric hospitals, 21 family medicine residencies face significant challenges to provide high-quality, high-volume pediatric experiences that are not already saturated with other learners. Therefore, more of these experiences may include significant shadowing time, which may not support developing increasing competency to care for children in the same way as caring for them in a residency continuity clinic.
Caring for children as part of continuity practice appeared to be the most powerful residency process associated with graduates caring for children, particularly in the inpatient setting. This finding suggests that developing a general comfort for caring for children as part of clinical practice is an important way for family physicians to develop not only the competence but also the comfort and confidence to take care of children. Unfortunately, the new ACGME family medicine training requirements have deemphasized the care of children in the continuity clinic setting by changing the requirements from greater than 10% of patients under the age of 10 years to greater than 10% of patients under the age of 18 years. On a practical level, this change decreases pediatric exposure, particularly to the youngest children in many programs. Our results suggest that these changes in training requirements will likely be followed by a decrease in the number of graduates caring for children in their future practices.
This study had several limitations. First, the overall response rates for both the CERA survey (43.7%) and the NGS (45.0%) were lower than expected, leading to a smaller-than-anticipated final cohort of 779 graduates from 211 residency programs. This reduced sample size potentially limited the study's statistical power and generalizability. Moreover, the exclusion of 844 residents due to nonresponse from program directors highlights a significant gap in data collection, which could introduce bias. Respondents to the NGS were representative of the class of 2018 and the programs with graduates that year; however, merging with the CERA data caused graduates from smaller programs to be underrepresented in the analytic sample, 14 which may have impacted the study’s findings, particularly those related to pediatric care in smaller or rural settings. Second, this study was based on a single cohort of 2018 family medicine residency graduates, which limited the ability to assess trends over time or the impact of evolving residency training requirements. Longitudinal studies with multiple cohorts would be needed to confirm the associations observed here. Lastly, the study relied heavily on program director–reported data via the CERA survey. In particular, the pediatric continuity care question had a lower response rate from program directors, which cut the sample size in half. Nearly half of program directors did not answer this item, which required them to estimate continuity clinic volumes and patient demographics. This is a limitation of CERA surveys that are based on program director impressions and not specific clinic data. Given the potential importance of this variable, we worked to address this issue by not including it in the original multiple regression analysis and analyzing it in a separate multivariant regression with items that were strongly correlated in the original regression analysis. Variability in program director participation suggests a need for improved engagement and reporting accuracy. Strengthening the importance of this survey within the program director community is essential for capturing comprehensive residency characteristics that can inform future training requirements and policies, particularly those set by ACGME.
If we want family physicians to continue to be competent and confident in their ability to care for children, and for health systems to feel confident that they can hire family physicians to provide primary care to all ages, then we need to make sure that our program requirements support what is needed to achieve this outcome. Our study suggests that strengthening requirements to ensure a higher volume of children seen in continuity practice and having faculty who model the care of young and sick children are more important than having a set number of pediatric rotations, which do not appear to influence scope of practice. The recent loosening of family medicine residency training requirements for pediatric care may risk exacerbating the decline in family physicians providing care to children, worsening access to primary care for children amidst a primary care access crisis. To address this issue, the ACGME Family Medicine Review Committee, federal training policy, and financing should emphasize stronger pediatric experience in continuity care and faculty role modeling to ensure that family physicians are prepared to provide essential child health care.
Support
The American Board of Family Medicine Foundation provided financial support for Dr Barr.
Presentations
North American Primary Care Research Group (NAPCRG) Annual Meeting, October 31–November 3, 2023, San Francisco, CA; Society of Teachers of Family Medicine (STFM) Annual Spring Conference, May 1–4, 2024, Los Angelas, CA.
References
-
Peterson LE, Fang B. Rural family physicians have a broader scope of practice than urban family physicians.
Rural and Underserved Health Research Center Publications. 2018; 5.
https://uknowledge.uky.edu/ruhrc_reports/5
-
Bazemore AW, Petterson S, Johnson N, et al. What services do family physicians provide in a time of primary care transition?
J Am Board Fam Med. 2011;24(6):635-636.
doi:10.3122/jabfm.2011.06.110171
-
Henry TL, Petterson S, Phillips RS, Phillips RL Jr, Bazemore A. Comparing comprehensiveness in primary care specialties and their effects on healthcare costs and hospitalizations in Medicare beneficiaries.
J Gen Intern Med. 2019;34(12):2,708-2,710.
doi:10.1007/s11606-019-05338-3
-
Eden AR, Morgan ZJ, Jetty A, Peterson LE. Proportion of family physicians caring for children is declining.
J Am Board Fam Med. 2020;33(6):830-831.
doi:10.3122/jabfm.2020.06.200089
-
Bazemore AW, Makaroff LA, Puffer JC, et al. Declining numbers of family physicians are caring for children.
J Am Board Fam Med. 2012;25(2):139-140.
doi:10.3122/jabfm.2012.02.110203
-
Ely D, Driscoll A.
Infant Mortality in the United States: Provisional Data from the 2022 Period Linked Birth/Infant Death File. National Center for Health Statistics; November 2023.
doi:10.15620/cdc:133699
-
Teasdale CA, Borrell LN, Shen Y, et al. Missed routine pediatric care and vaccinations in US children during the first year of the COVID-19 pandemic.
Prev Med. 2022;158:107025.
doi:10.1016/j.ypmed.2022.107025
-
Nguyen KH, Nguyen K, Lekshmi D, Corlin L, Niska RW. Delays in children’s preventive health services during the COVID-19 pandemic.
Fam Med. 2022;54(5):350-361.
doi:10.22454/FamMed.2022.922801
-
-
Peterson LE, Fang B, Puffer JC, Bazemore AW. Wide gap between preparation and scope of practice of early career family physicians.
J Am Board Fam Med. 2018;31(2):181-182.
doi:10.3122/jabfm.2018.02.170359
-
Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of intended scope of practice for family medicine residents with reported scope of practice among practicing family physicians.
JAMA. 2015;314(22):2,364-2,372.
doi:10.1001/jama.2015.13734
-
-
Makaroff LA, Xierali IM, Petterson SM, Shipman SA, Puffer JC, Bazemore AW. Factors influencing family physicians’ contribution to the child health care workforce.
Ann Fam Med. 2014;12(5):427-431.
doi:10.1370/afm.1689
-
Barr WB, Peterson LE, Fleischer S, Seehusen DA. National family medicine residency outcomes project methodology.
PRiMER. 2024;8:52.
doi:10.22454/PRiMER.2024.588860
-
-
Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research.
Ann Fam Med. 2018;16(3):257-260.
doi:10.1370/afm.2228
-
-
Peterson LE. Using the family medicine national graduate survey to improve residency education by monitoring training outcomes.
Fam Med. 2021;53(7):622-625.
doi:10.22454/FamMed.2021.719992
-
Weidner AKH, Chen FM, Peterson LE. Developing the national family medicine graduate survey.
J Grad Med Educ. 2017;9(5):570-573.
doi:10.4300/JGME-D-17-00007.1
-
-
Leyenaar JK, Freyleue SD, Arakelyan M, Goodman DC, O’Malley AJ. Pediatric hospitalizations at rural and urban teaching and nonteaching hospitals in the US, 2009-2019.
JAMA Netw Open. 2023;6(9):e2331807.
doi:10.1001/jamanetworkopen.2023.31807



There are no comments for this article.