Background and Objectives: Effective feedback is recognized as essential to clinical training. Hattie and Timperley conducted a comprehensive review of feedback to develop their Model of Feedback to Enhance Learning (MFEL). The MFEL proposes that effective feedback can focus on any of four levels: task, process, self-regulation, and self. While Hattie and Timperley are frequently cited for their review, few studies in medical education have used the MFEL to explore feedback. We used the MFEL to examine the content of documented workplace-based feedback to explore how this model applies in a family medicine residency program.
Methods: We conducted this retrospective cross-sectional observational secondary data analysis (learning analytics) study in a Canadian university-based family medicine residency program. Our data source was de-identified field notes (a tool to document workplace-based feedback) for residents at two teaching sites. We coded the feedback using the levels from the MFEL. We used descriptive statistics to analyze the frequencies of each level and combinations of levels.
Results: Of the 2,250 field notes examined, 422 (18%) were excluded because they contained no feedback. The majority (1,105; 60%) included a single feedback level, while 705 (38%) contained two levels, and 17 (1%) included three levels. No field notes included all four levels. Of the field notes containing one feedback level, the most common levels were task (835; 76%) and process (248; 22%). The most common combination of levels was process and task (649; 92.1%).
Conclusions: Hattie and Timperley’s MFEL offers a way to explore feedback documented in medical education programs and may help programs identify opportunities for faculty development to improve feedback effectiveness.
Feedback is an essential element of clinical training, allowing preceptors to reinforce strengths and address gaps with their learners, and learners to monitor their competence. 1 One of the most cited publications about feedback effectiveness is “The Power of Feedback” by Hattie and Timperley. 2 In their paper, Hattie and Timperley conducted a review of feedback to develop a Model of Feedback to Enhance Learning (MFEL). According to the model, the purpose of feedback is to “reduce discrepancies between current understanding and performance and a goal” (p. 87). The model posits three key learner questions that must be answered for feedback to be effective: What is my learning goal? How am I doing in relation to that goal? and Where do I need to go next? 2 While this paper is often cited in the medical education literature, few researchers have applied the MFEL in the context of medical education to examine narrative feedback captured on assessment forms—a crucial gap in the literature given the increasing emphasis on narrative feedback as part of assessment. 3-5
Hattie and Timperley proposed that each of the key learner questions in the MFEL work at four core levels: task, process, self, and self-regulation (Table 1 ).2 Task-level feedback gives information about how well or correctly a task is performed, while process-level feedback discusses the learning process or approach that was or should have been used to accomplish a task. Self-level feedback refers to feedback describing personal characteristics of the learner that contribute to completing a task. Finally, self-regulation feedback addresses how the learner participates in their own learning by monitoring their progress and engaging in strategies to accomplish a task.
|
Feedback level
|
Description
|
Coding example from field notes
|
|
Task level
|
Focus is on how well the learner performs and/or understands the task.
|
“Pap test completed successfully . For next time, make sure the patient knows why the test is done and what to expect.”
|
|
Process level
|
Focus is on the process needed for understanding or performing the task.
|
“You demonstrated a systematic approach to locating the cervix. ”
|
|
Self level
|
Focus is on attributes or characteristics of the learner (him/them/herself).
|
“Excellent work today. You’re a capable, compassionate doctor, and I am proud to work with you.”
|
|
Self-regulation level
|
Focus is on the cognitive aspects of performing the task, such as self-monitoring or demonstrating regulation of action(s) or emotion(s).
|
“Despite very difficult subject, clearly had patient’s trust. Excellent reflective assessment of own experience and performance—insightful about what to change next time. ”
|
Hattie and Timperley’s model articulates the elements that make up the content of effective feedback, regardless of how the feedback is delivered. 2 This makes the MFEL useful for examining the effectiveness of narrative feedback, such as on workplace-based assessment forms. In this exploratory study, we use the MFEL to examine feedback within a family medicine residency program and answer the following:
-
How can Hattie and Timperley’s MFEL be applied to narrative feedback?
-
What feedback levels appear in narrative feedback comments in postgraduate family medicine workplace-based assessment forms?
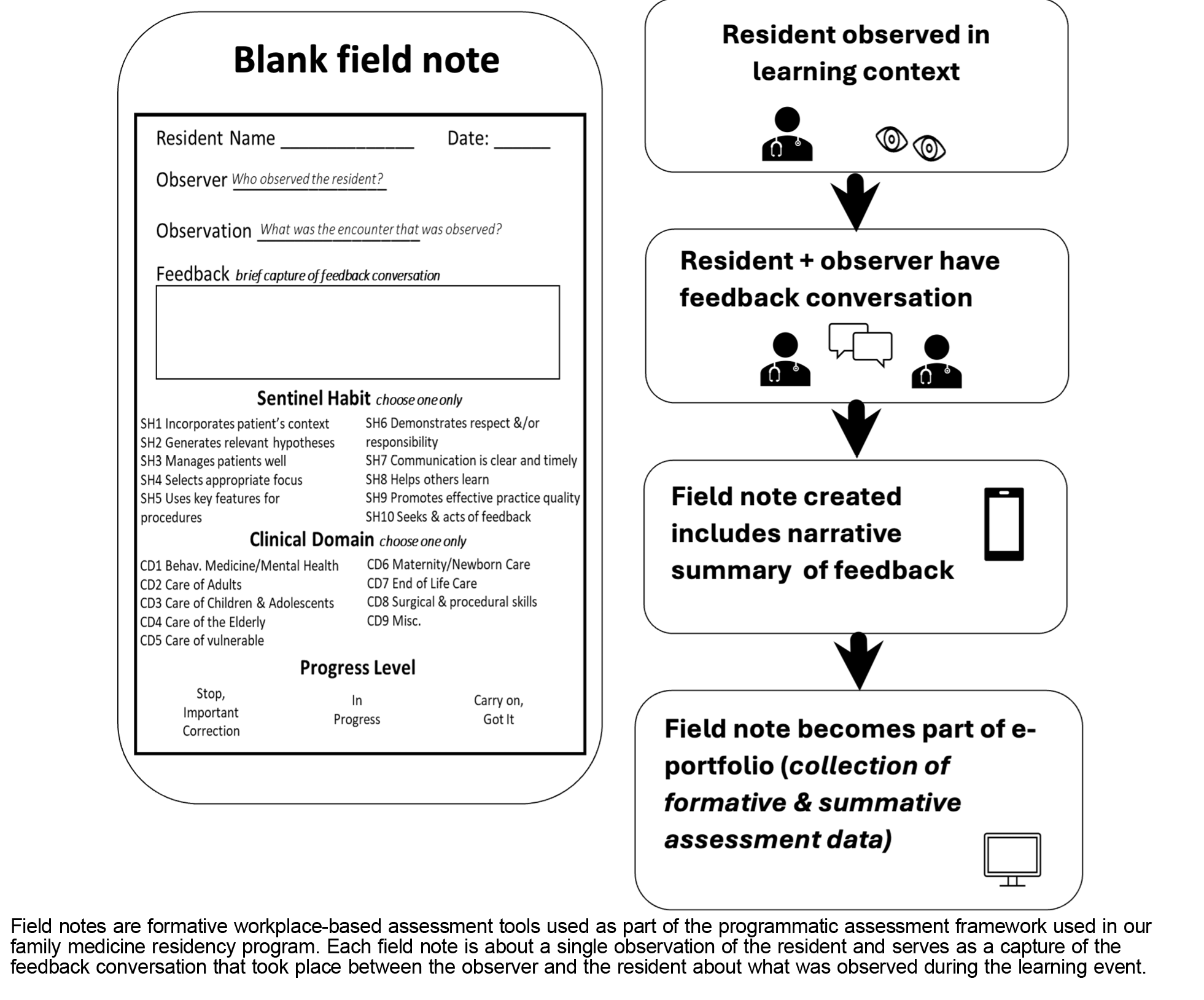
We conducted this study in a university-based family medicine residency program in Canada. The program uses field notes for formative workplace-based assessment. 6-8 Field notes are completed after direct observation of the resident by a teacher and contain information such as the clinical context, judgment of the level of competence demonstrated, and a narrative summary of the feedback conversation that took place between the resident and teacher (Figure 1). 8-10 Field notes are completed electronically and become part of the resident’s assessment eportfolio. 8
We included de-identified field notes entered between 2015 and 2018 for residents at two teaching sites. We coded the narrative feedback included in these field notes using the four levels of feedback from the MFEL (Table 1, far right column). To ensure consistency, we held multiple calibration sessions, during which each author coded 30 field notes. Coding discrepancies were discussed until consensus was reached. Cohen’s κ was used to assess interrater reliability between two raters for unordered categories. After four calibration sessions, Cohen’s κ reached 0.671, which represented substantial agreement between A.L. and K.C. The remainder of the field notes were coded by K.C. We analyzed the frequency of each of the feedback levels, as well as combinations of feedback levels, using descriptive statistics.
Ethical approval for this study was granted by the University of Alberta Human Research Ethic Board (ID: Pro 00004050).
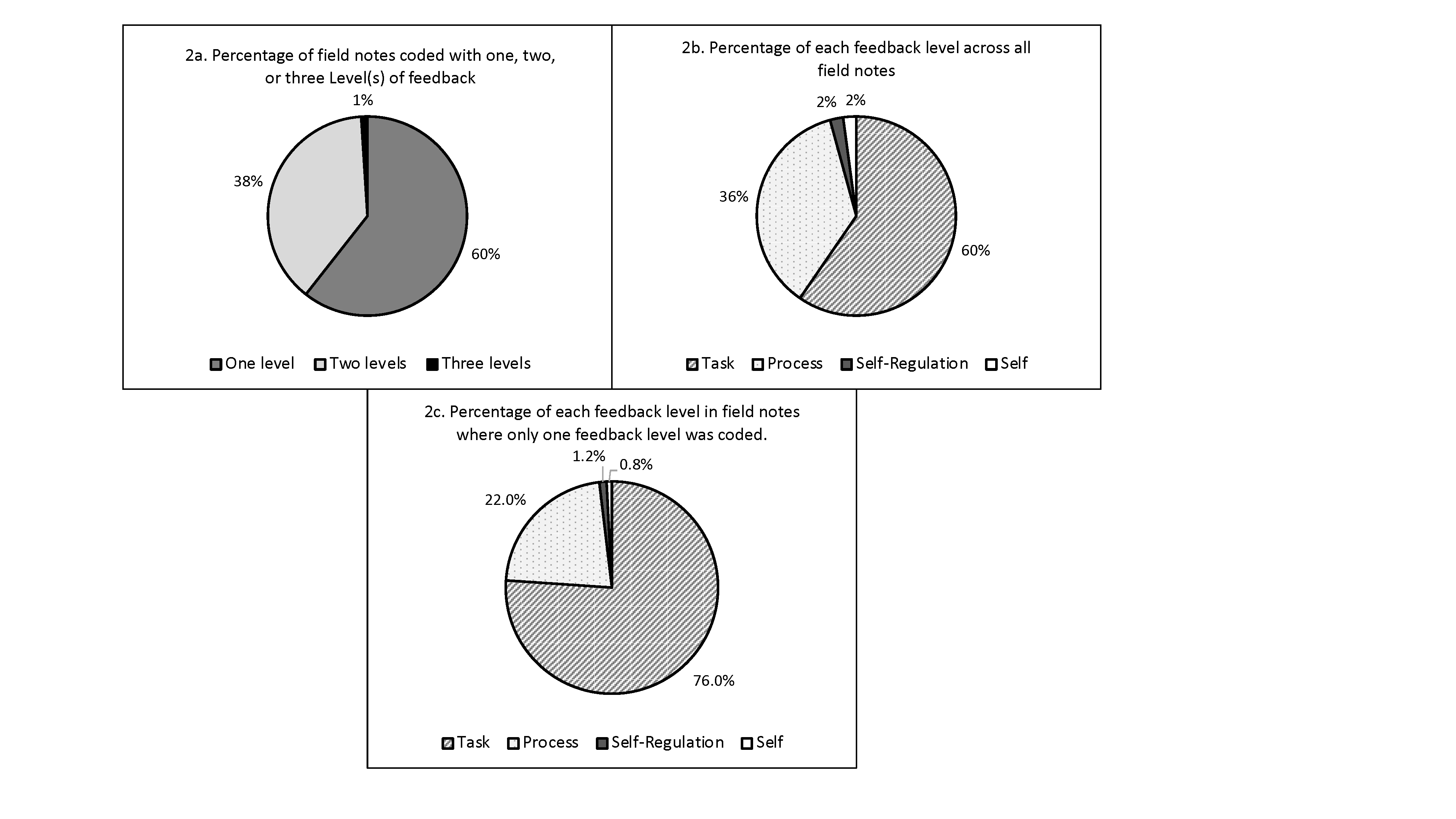
We examined 2,250 de-identified field notes. Of these, we excluded 422 (18%) field notes that did not include any narrative feedback. For the remainder of the field notes (N=1,828), the majority (1,105; 60%) included only one feedback level, 705 (38%) included two, and 17 (1%) included three (Figure 2a). None included all four feedback levels. In total, across all field notes, task was included the most frequently (1,533; 60%), followed by process (930; 36%), self-regulation (49; 2%) and self (49; 2%; Figure 2b). Of the field notes containing one feedback level, the most frequently included was task, which was present in 835 (76%). This was followed by process, which was included in 248 (22%) field notes, self-regulation in 13 (1.2%), and self, which was included in 9 (0.8%) of the field notes (Figure 2c).
We also examined the frequency counts for different combinations in field notes that contained more than one level. The most commonly seen feedback level combination was task and process (649; 92.1%), followed by task and self (19; 2.7%), task and self-regulation (16; 2.3%), process and self (12; 1.7%), and process and self-regulation (8; 1.1%). The most infrequent combination was self and self-regulation (1; 0.1%).
DISCUSSION AND CONCLUSIONS
When using Hattie and Timperley’s MFEL to examine narrative feedback captured in our program’s field notes, we found that the majority included only one feedback level. Hattie and Timperley suggested that effective feedback often contains multiple levels, but time constraints may limit the levels of feedback in the clinical setting. In field notes that contained a single feedback level, either task or process level was most commonly coded, indicating that our program’s preceptors place emphasis on these two levels. Feedback at the task level is effective when knowledge is present and correction for faulty interpretations is needed. It can, however, be less effective than process level feedback because it lacks information about the underlying processes that lead to successful task completion.
For field notes that included two feedback levels, the most commonly coded combination was task and process. Hattie and Timperley noted that these two levels can have an interactive effect on one another by increasing task confidence for improving processes. Self and self-regulation were least likely to be in the field notes. Feedback at the self level is considered less effective because it is not focused on improving performance; thus, finding it infrequently included was reassuring. Feedback at the self-regulation level, however, is important to the learning process. The infrequent feedback at this level warrants further understanding, particularly in a profession where continuous personal development is expected.
Moreover, we found that some field notes included no feedback, and instead documented the context of the feedback conversation, such as the patient encounter. This finding identifies a potential area for improving the use of field notes.
Our data was collected from one family medicine residency program, which may limit its transferability. Additionally, we were able to code only feedback that was recorded in the field notes, and we recognize that some components of the feedback conversations may not have been recorded or included in our analysis.
The results of this exploratory study offer opportunities for further research using Hattie and Timperley’s four levels of feedback, such as examining change in feedback focus as a resident progresses through the program or based on the preceptor’s relationship to the resident (longitudinal vs episodic).
The findings of this study provide preliminary support for the use of the MFEL, especially the four levels of feedback, in medical education. Our analysis of narrative feedback on assessment forms using the feedback levels resulted in a more nuanced understanding of preceptors’ focus when documenting feedback with residents. Examining feedback using the MFEL could help programs identify opportunities to target faculty development to improve the effectiveness of feedback.
Presentations
This work was previously presented as an oral presentation at the Ottawa 2024 Conference on the Assessment of Competence in Medicine and the Healthcare Professions, February 25, 2024.
References
-
Cantillon P, Sargeant J. Giving feedback in clinical settings.
BMJ. 2008;337:a1961.
doi:10.1136/bmj.a1961
-
-
Hodges B. Assessment in the post-psychometric era: learning to love the subjective and collective.
Med Teach. 2013;35(7):564-568.
doi:10.3109/0142159X.2013.789134
-
Ross S, Hauer KE, Wycliffe-Jones K, et al. Key considerations in planning and designing programmatic assessment in competency-based medical education.
Med Teach. 2021;43(7):758-764.
doi:10.1080/0142159X.2021.1925099
-
-
Donoff MG. The science of in-training evaluation: facilitating learning with qualitative research. Can Fam Physician. 1990;36:2,002-2,006.
-
-
Ross S, Poth CN, Donoff M, et al. Competency-based achievement system: using formative feedback to teach and assess family medicine residents’ skills. Can Fam Physician. 2011;57(9):e323-e330.
-
Lee JR, Ross S. A comparison of resident-completed and preceptor-completed formative workplace-based assessments in a competency-based medical education program.
Fam Med. 2022;54(8):599-605.
doi:10.22454/FamMed.2022.854689
-
Ross S, Lawrence K, Bethune C, et al. Development, implementation, and meta-evaluation of a national approach to programmatic assessment in family medicine residency training.
Acad Med. 2023;98(2):188-198.
doi:10.1097/ACM.0000000000004750



There are no comments for this article.