Family medicine residency programs can implement pathway programs to grow a diverse primary care workforce capable of caring for all patients and communities. A pathway program aims to support students from selected level(s) of the educational continuum toward becoming qualified applicants to health professions programs. This guide provides an evidence-informed approach to developing, implementing, and evaluating effective pathway programs that residency programs can use to build the diverse health care workforce that is critical for health equity. First, we provide practical guidance for program development that uses a logic model and builds partnerships with schools and crucial stakeholders. Then, we discuss how to incorporate a needs assessment to align program goals with student needs. Next, we describe how to leverage social cognitive theory to maximize impact on learners and their ultimate achievement. Finally, we overview systematic evaluation to support long-term program success. Effective program planning leverages the processes through which learning occurs, influencing learners’ self-efficacy and outcomes expectations through relatable role models and mastery experience. We provide concrete examples from the Family Medicine Bridging the Gap Pathway Program. Pathway program developers can accelerate students’ trajectory toward health profession graduate schools by choosing interventions that serve their greatest needs, thus preparing competitive applicants able to progress to the next educational level.
The Association of American Medical Colleges recently reported that 49.4% of all graduates of US medical schools (2022–2023) were non-Hispanic White; 23.5% were Asian; 6.7% were Black; 5.7% were of Hispanic, Latino, or of Spanish origin; 0.2% were American Indian or Alaska Native; and 0.05% were Native Hawaiian or other Pacific Islander. 1 Recruitment and retention of individuals underrepresented in medicine (URiM) is a key solution to improve health care use, lower health care expenditures, enhance patient satisfaction with care, and address physician shortages in rural and medically underserved areas; however, efforts to remedy the URiM physician shortage have thus far been unable to significantly improve representation rates of these groups. 1-6 Over the past 20 years, the percentage of URiM medical students remained underrepresented compared with the US population. 7, 8 Addressing ongoing shortages requires efforts along the educational pathway, including proactive community-level partnered efforts by health profession schools to support successful matriculation and retention of aspiring students in medical education. 9 A pathway program aims to support students from selected level(s) of the educational continuum toward becoming qualified applicants to health professions programs.10 K-12 pathway programs for URiMs are part of a multipronged approach to build sustained long-term improvement in URiM representation in medical schools, residencies, and the workforce; 11-13 however, to be effective, such programs must be not only well-intentioned, but also evidence-informed.
Family medicine departments that house residency programs have an opportunity to support development of the workforce and are well positioned to create successful partnerships with local schools in the communities they serve. Family medicine residency programs are motivated to recruit a diverse workforce that reflects their community’s needs. 14 Furthermore, the Accreditation Council for Graduate Medical Education expects residents and residency programs to engage in and lead community innovations and workforce recruitment.15, 16 To help residency programs achieve these objectives, here we provide a practical guide, with concrete examples from the Family Medicine Bridging the Gap Pathway Program, for developing and implementing K-12 school pathway programs in family medicine residency programs. This guide includes program planning model fundamentals, including preplanning, building partnerships with K-12 schools, assessing student needs, and aligning these with pathway program goals. It also covers implementation fundamentals, such as applying a theoretical framework (eg, social cognitive theory) to facilitate improved outcomes, and evaluation fundamentals for demonstrating results and promoting continued growth and organizational support of pathway programming.
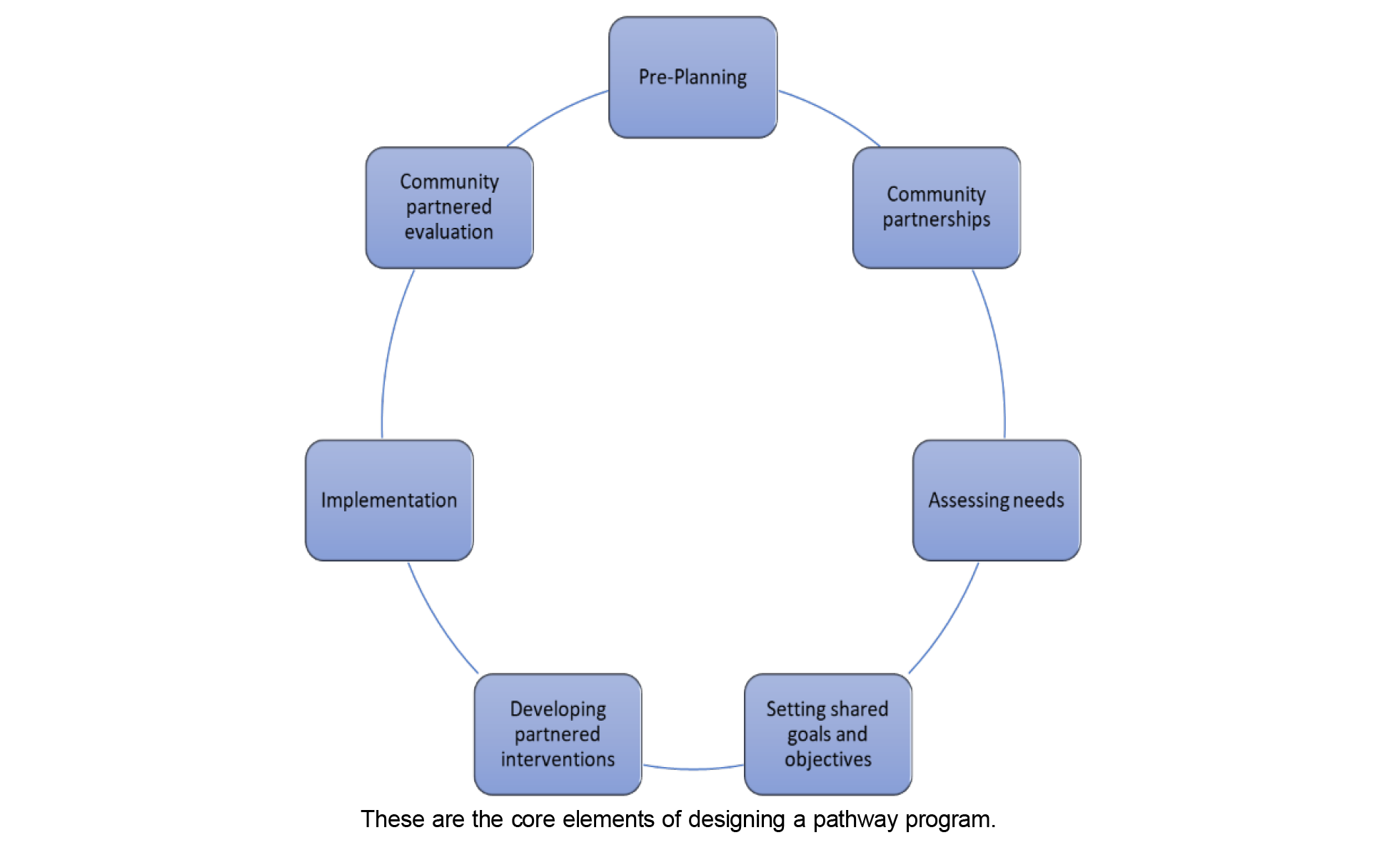
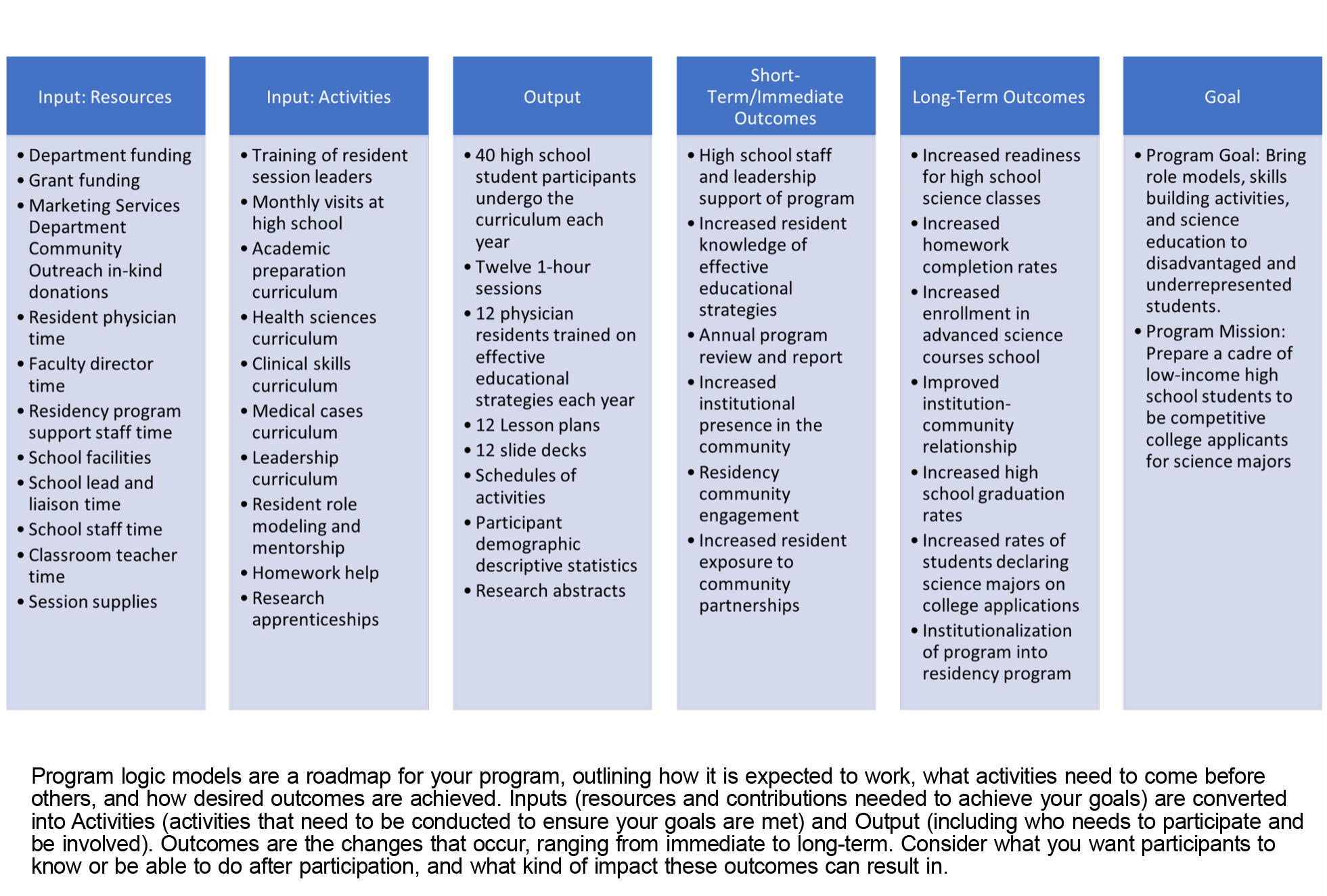
The core elements of designing a pathway program include preplanning, community partnership, needs assessment, goals and objectives setting, intervention development, implementation, and evaluation. Figure 1 is a program planning model to guide you through this process. As you proceed through the early phases of program design, develop a roadmap for your program (a logic model) that defines the sequence between planned work and intended results. As a graphic illustration of the relationships among a program’s resources, its activities, and its intended effects, 17 logic models are a useful tool in structuring the planning, implementation, and evaluation processes 18 and are associated with the development of successful programs. 19 Figure 2 is an example of a logic model for a pathway program.
DEVELOPMENT: PREPLANNING, PARTNERSHIP, NEEDS ASSESSMENT
Preplanning
The first step in preplanning is defining your program’s mission. Your mission statement answers the question, Why does this program exist and what does it hope to accomplish? Keep in mind that—while career awareness and motivation interventions are the easiest to conduct—research shows that URiM interest in science and health careers already matches or exceeds that of non-URiMs. 20 Instead, consider a program mission that centers on academic enrichment, academic support, safe spaces, research opportunities, and college preparation for students from disadvantaged backgrounds with inequitable access to such opportunities. Once a concise mission statement is defined, effective program goals can emerge as you assess needs and develop your basic program elements.
The next step is identifying a target K-12 school and laying the groundwork for a partnership. Defining a successful partnership requires an inventory of your institution’s available and needed resources, including the specific contributions that you hope your partner organization will bring. This inventory helps determine program scope and informs the intervention model and planned partnership. The inventory of resources that will enable the program becomes the first component of your logic model.
Partnership
The proposals presented to your potential partner organization should be transparent about currently available resources, specify the program’s intended duration, and describe plans for sustainability. Each organization should address capacity and identify leaders responsible for managing and implementing program activities. These team leaders are also responsible for maintaining mission fidelity and the partnership relationship. Trust is essential to the partnership. Sponsoring institutions may demonstrate their true commitment to equity in the negotiation of partner roles and responsibilities to ensure that an unfair burden is not placed on the partner organization. 20 This level of accountability builds trust and shows the institution's true commitment to equity.
Partnership development also includes identifying and engaging any stakeholders whose support will be essential to the building, implementation, and long-term success of the program. Institutional stakeholders to consider include individuals and groups—from administrative staff to institutional leadership—housed within the sponsoring department, university, and health system. Engaging these stakeholders can center around common goals. Garnering institutional support requires demonstrating the added value of the investment in effort and resources, and clearly delineating how sponsoring a pathway program meets institutional goals and mandated standards. In the development of the Bridging the Gap Program, this dialogue was initiated with residency and department leadership jointly; and subsequently, administrative staff, school leadership and teachers; with eventual creative identification of health system sources of support, such as the marketing services department (Figure 2).
In the partnering school, stakeholders include administrators, teachers, parents, and the students themselves. Having buy-in from both administrative leadership and schoolteachers is essential for engagement, trust-building, and program success. Buy-in can be fostered by conveying program benefits clearly, demonstrating the institution’s commitment and credibility, and addressing potential areas of concern. These areas can include added workload. In addition, school personnel may be skeptical about long-term commitment because projects come and go, and funding is unstable. 20 Residency programs can establish trust by acknowledging the challenges schools and teachers face (eg, lack of resources, teaching loads, class sizes) in their pathway program design and in the asks and expectations of school personnel. Programs should also solicit feedback on the partnership and planned intervention components. Early on and over time, maintaining transparency when things are not going as planned and engaging these community stakeholders in such challenges will further build trust and promote creative solutions. In the Bridging the Gap Program, the faculty director of the program initially met frequently with school leadership and teachers, then less often but regularly to provide space for dialogue, transparency, and further innovation.
Needs Assessment
After establishing the mission and partnerships for your pathway program, conduct a needs assessment to help you identify, analyze, and prioritize the needs of your specific group of learners. 21 The prioritized needs then inform the program goals and objectives. Setting program goals after the needs assessment sets up a pathway program for success because no program can optimally achieve its goals unless it accounts for learners’ needs and learning environment. This needs assessment also will help garner buy-in from stakeholders, including and especially students. Allowing students to tell you what they need and how you can help them aligns with principles of applying an equity lens and facilitates learners’ agency and social power toward their own social and academic goals. 22 This step is essential to centering the needs and experiences of marginalized communities and thus to developing a program truly committed to mitigating disparities. As recently summarized by the National Academies, societal barriers that specifically or disproportionately impact students from a URiM background include school-level racial-economic segregation and achievement; uneven distribution of opportunities to learn in STEM (science, technology, engineering, and mathematics) education; learner experiences in education varying by race, ethnicity, socioeconomic class, and gender with consequences for learning, identity, and sense of belonging in STEM; and psychological phenomena like stereotype threat that can affect academic performance. 23
IMPLEMENTATION: THEORETICAL FRAMEWORK, DEFINING BASIC ELEMENTS, EDUCATIONAL AND INTERVENTION STRATEGIES
Theoretical Framework
Pathway program development, like clinical medicine, should prioritize evidence-informed approaches to avoid a design based on a planner’s well-intentioned yet incorrect instincts about what would work, familiar but ineffective approaches, or the ease of implementation. In this context, effective program planning uses behavior change theory to (a) understand potential drivers of the targeted problem (eg, context-specific barriers students face), (b) identify where to target your intervention, (c) develop the right methods to address your targeted problem, and, most importantly, (d) increase the efficacy of your program.
A particularly well-suited and validated behavior change theory to apply in education and pathway program development is social cognitive theory (SCT) 24 and, an extension of this, social cognitive career theory. 25 SCT enables us to understand factors that influence student behavior; the processes through which learning occurs; and how this learning paves the way for goal setting, academic choices, and career choices. 25 Thus, those developing programs can apply SCT to select and develop program components that address these key factors. As SCT posits, individuals tend to form goals related to activities that are associated with higher self-efficacy and more positive outcome expectations.
Self-efficacy beliefs describe one’s beliefs about their personal ability to perform behaviors that bring desired outcomes. Unless learners believe that their actions can produce the outcomes they desire, they have little incentive to act or to persevere in the face of difficulties. For instance, a person is more likely to apply to college if they believe they will be accepted. Thus, influencing learners’ self-efficacy and outcomes expectations impacts the goals they set and the courses of action they pursue. We can increase self-efficacy through social modeling (providing relatable role models), mastery experience (providing new learning experiences that lead to success in attainable and increasingly challenging performances of desired behaviors), verbal persuasion (providing encouragement to boost confidence to induce efforts toward behavior change), and improvement of physical and emotional states (reducing stress and building positive emotions before attempting new behaviors).
Regarding social modeling, role models are imitated especially when observers perceive the models to be similar to themselves. Further, “coping models,” individuals who have confronted and successfully struggled with the same challenges and barriers, are especially valuable in increasing self-efficacy and should be a key component of programming. Importantly, cross-cultural coping models should be appropriately trained and incorporated to avoid disproportionate taxation on residents and faculty who are URiM. 26
Self-efficacy and outcome expectations are facilitated or impeded by socio-structural factors. Socio-structural factors that programs can address range broadly and should reflect the findings of your needs assessment. Examples of facilitators include providing resources (eg, financial aid resources), tools (eg, academic), or environmental changes (eg, access to research opportunities) that make new behaviors easier to perform. Moreover, as far as career choices go, interests will be translated to a career choice only if barriers are perceived as possible to overcome. Because financial barriers often are cited by students of underrepresented backgrounds, consider how you might address this barrier through your program. For example, you might provide assistance with applying for scholarships. In the Bridging the Gap Program needs assessment, students identified financial barriers to college education; thus, a “Financing Higher Education” session was created and enhanced with student input.
Defining Basic Elements: Setting Goals and Objectives
A well-defined mission statement will enable you to develop effective program goals. Use SMARTIE (specific, measurable, achievable, relevant/realistic, time-bound, inclusive, equitable) as a tool to plan and write goals and objectives for your program and for your sessions. 27
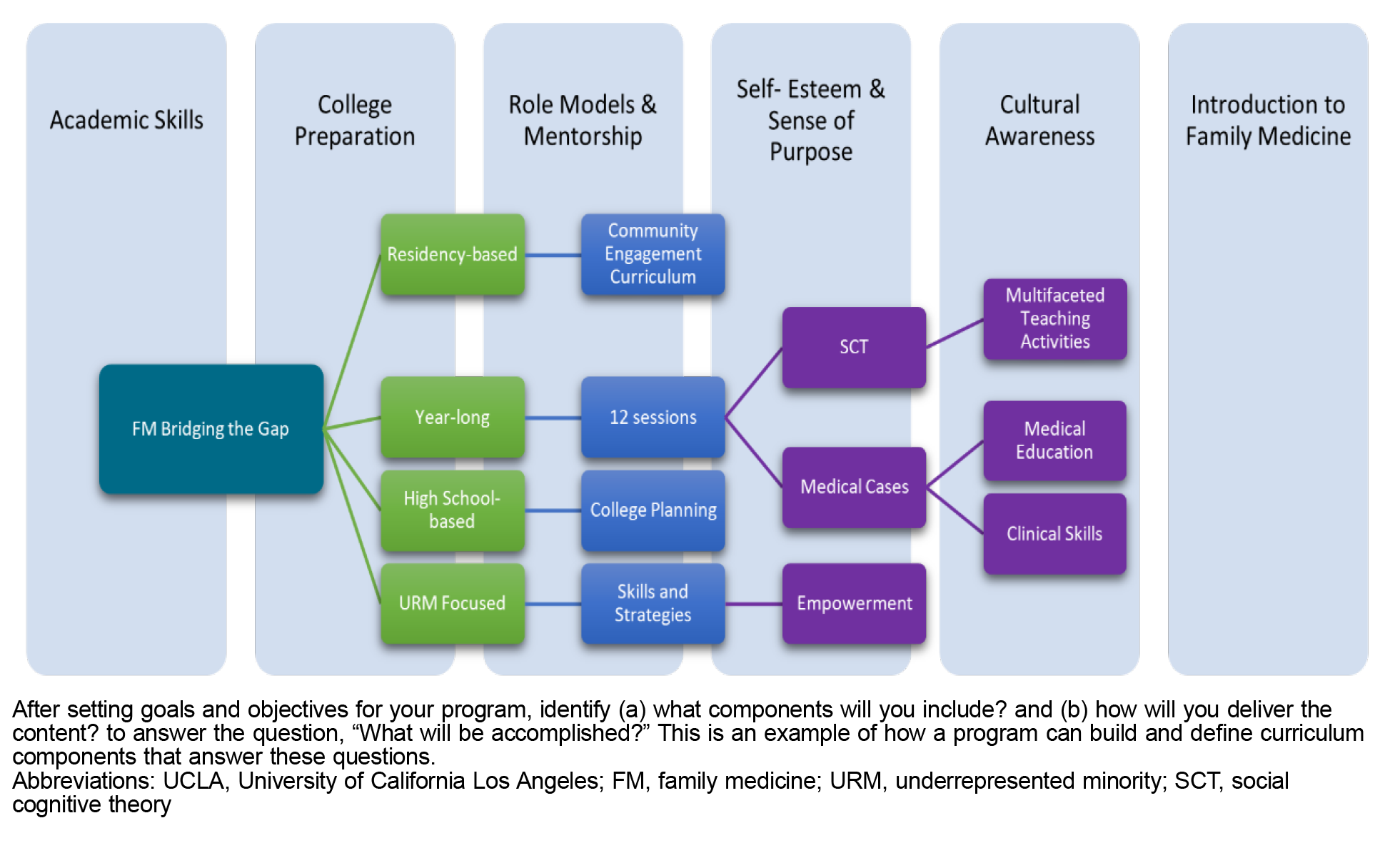
After setting goals and objectives for your program, brainstorm (a) content (what components will you include?) and (b) method (how will you deliver the content?) to answer the question, “What will be accomplished?” Based on the Bridging the Gap Program, Figure 3 illustrates building and defining curriculum components that answer these questions. 28, 29 Once these elements of your program design are defined, you can focus on individual lesson plans. To develop session curriculum, you will similarly progress through a process of writing session goals, then session objectives, followed by defining your content and learning methods. 30 This simplified approach exemplifies the curriculum development process. In practice, the curriculum development process may not proceed in this linear fashion, as it is an interactive, partnered, and continual process. In successful curriculum development, the curriculum evolves, based on evaluation results, increasing resources, changes in targeted learners, and changes in the material requiring mastery. Your theoretical framework should be embedded throughout your curricular components as well as your methods.
Educational and Intervention Strategies
Though less often a focus of pathway program interventions, as a result of inequitable access to high-quality teachers and opportunities, academic and college preparation serve the greatest needs of underrepresented youth from underresourced educational settings. 20, 23, 10 Strategies to build student academic preparation include science instructional enrichment, research apprenticeship, and academic enhancing skills such as test-taking strategies. Nonacademic enrichment strategies include financial college preparation instruction, parental involvement and education, reward incentives, creation of psychological safe spaces of belonging, 23, 31 and coaching and mentoring.
Other strategies to consider include (a) early interventions to maximize potential impact well before students are expected to be considering college preparation, (b) long-term programs where students apply concepts for mastery experience, and (c) career discovery activities that expose students to a broad array of options previously unknown to them. Offering programs earlier on the educational pathway and focusing on economically disadvantaged, racially minoritized, and marginalized communities (eg, English language learners) can further capture a wider net of students who may later consider a health care career. In addition, pathway program developers must ensure a mindset of high expectations for students from disadvantaged backgrounds to help counter any unconscious biases and racialized narratives they carry regarding student achievement. 32
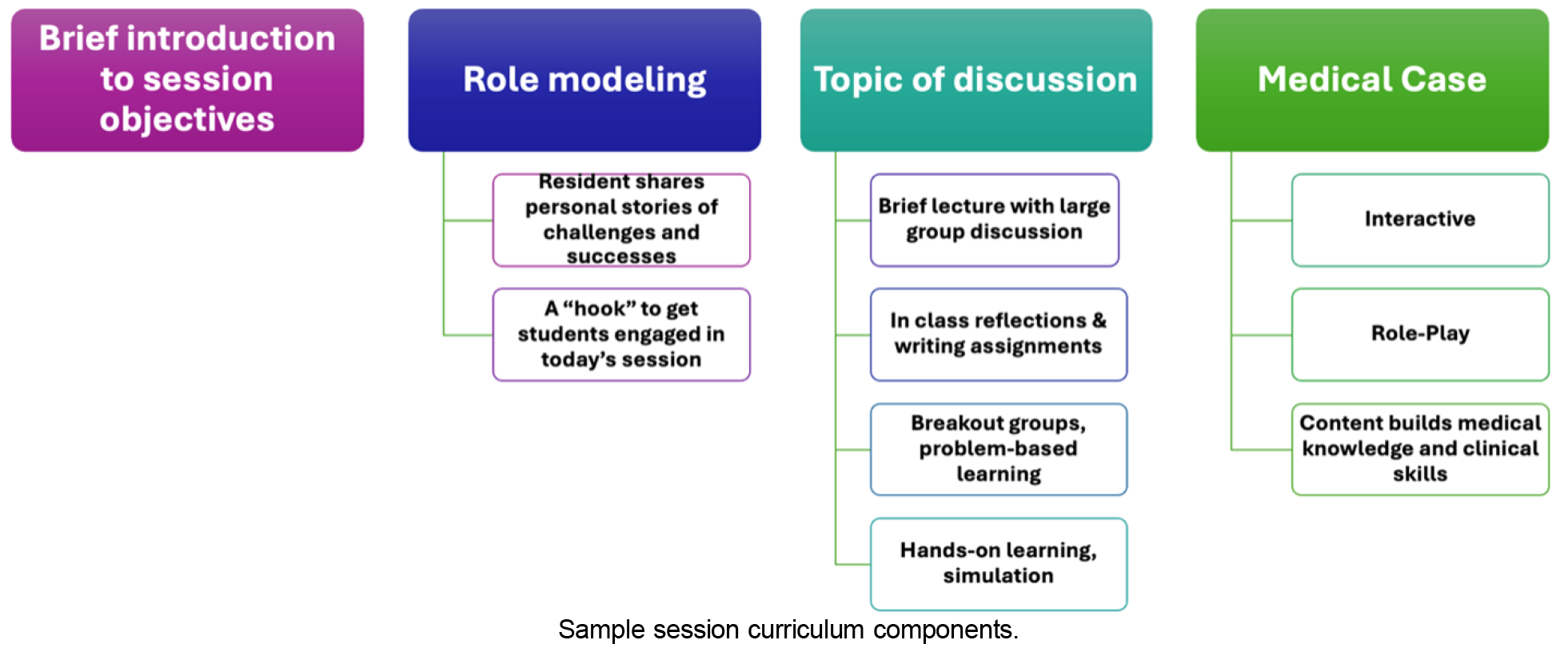
Once broad program strategies are identified, curriculum content and educational methods are chosen. We recommend active learning methods and peer-led team learning, which have been demonstrated to successfully increase engagement. 33 Other excellent strategies include cases, problem-solving exercises, simulations, role-play, and reflection exercises. Aim to include two to three different educational strategies in each session’s lesson plan. Sample session curriculum components are presented in Figure 4.
EVALUATION: TYPES AND FOCUS
Evaluation design will be informed by the program goals, logic model, questions to be answered, available resources, resources and capacity of the partner school, and funding requirements. 18 Draw on your logic model to develop measurable and targeted evaluation questions that are high-quality and actionable, identify your data sources, and select appropriate analyses. 18 Your evaluation should be an integral part of program planning, not something to consider after implementation is complete. 17
With regard to evaluation design, pilot programs are often small in scope and evaluated using descriptive or correlational designs. We strongly encourage partnering with researchers trained in evaluation to aid development of evaluation approaches that increase accountability and validation of effective programs. 34 If promising evidence is found, programs may then be scaled up. 18
Types of Evaluation Design
Table 1 escribes three evaluation designs in their approach to evaluating program effectiveness. Descriptive designs document program implementation by answering who, what, where, when, and to what extent, helping identify barriers and outcomes. Correlational designs examine relationships between variables without establishing causality, helping understand associations and participant changes. Comparison group designs assess program impact by comparing outcomes between treatment and a comparator group, with quasi-experimental approaches using statistical adjustments and randomized controlled trials providing the strongest evidence of causality.
|
Design type
|
Purpose
|
Questions
addressed
|
Example evaluation questions
|
Examples
from
Bridging the Gap
|
|
Descriptive
|
Document how a program works, provide feedback on implementation, identify barriers to program success, or help determine the best outcomes for assessing program effectiveness.
|
Who?
What?
Where?
When?
To what extent?
|
What are the demographic characteristics of students and volunteers?
How many sessions did students receive?
|
Annual reporting of curricular content, participant demographics, and participant feedback.
|
|
Correlational
|
Identify a relationship between two variables and determine whether that relationship is statistically meaningful. Does not demonstrate causality but may uncover other relationships of interest.
|
How program participation relates to outcomes of interest.
Understand associations among various subgroups and changes in participants’ knowledge, skills, and behaviors.
Determine how differences in implementation are associated with intended outputs.
|
Did the residents who participated in program training demonstrate an increased knowledge of effective educational strategies?
|
Evaluation of changes in student and resident participant knowledge and skills.
|
|
Comparison group
|
Determine whether a program is likely to have caused its expected outcomes by comparing the outcomes of a treatment group, which receives the intervention, to the outcomes of a comparison group, which does not receive the intervention.
|
Quasi-experimental designs use matching or other statistical adjustments to create treatment and comparison groups that are as similar as possible to one another.
Randomized controlled trials assign individuals to the treatment or comparison group to help ensure that any changes observed in the treatment group are most likely due to the intervention and not to some other cause, thus offering the highest-quality evidence of effectiveness of a program.
|
Did participation in the program affect student enrollment in advanced science courses in high school? Did participation in the program increase college matriculation rates?
|
Set up a comparison group from another classroom serving a similar population of students and operating under a “business as usual” condition in which no interventions were offered.
|
Evaluation Focus
Process evaluation. Process evaluation questions help describe a program and the quality of its implementation by focusing on resources, activities, and outputs. Example process evaluation questions include, “Is the program being implemented as intended?” and “What needs to be improved in the program, and how?” 18
Outcome evaluation. Outcome evaluation questions are focused on the results of a program over the short-, mid-, and long-term. However, using descriptive and correlational designs to answer outcome evaluation questions cannot provide evidence of efficacy. 18 Example outcome evaluation questions include, “What are the effects of the program on knowledge of financial aid options for paying for college?” and “Were the intended outcomes on high school graduation rates achieved?”
Learning evaluation. Applying a well-established model of learning evaluation such as the Kirkpatrick evaluation model helps demonstrate curricular impact and facilitates dissemination and publication. The Kirkpatrick model frames assessment at four levels: 35
-
Level 1: Learner reaction
-
Level 2: Acquisition of the intended knowledge, skills, attitudes
-
Level 3: Behavior change
-
Level 4: Ultimate organizational-level, system-level, and other high-level results
Level 4 is critical, but all levels have a role in indicating impact (or lack thereof) and in identifying which aspects of the program should continue and which should be modified or discontinued. When preparing for dissemination and publication, reporting models such as the DoCTRINE guidelines can aid scholarly curriculum development reporting. 36 Documenting program impact is crucial for attracting resources and long-term institutionalization; sponsoring organizations should dedicate funds for rigorous evaluation. 20
Pathway programs can help increase medical school and residency diversity toward a goal of sustained improvement in URiM representation. 11-13 Family medicine departments are ideally positioned to partner with schools37 to develop pathway programs tailored to growing a diverse primary care workforce. However, to be effective, programs must be evidence-informed; while career awareness and motivation interventions are easiest to conduct, research shows that URiM student interest in health careers already matches or exceeds that of other students. 20 Further, URiM students are disproportionately more likely to have inequitable preK-12 and out-of-school learning opportunities. 23 Therefore, family medicine programs must address other barriers to recruit and retain diverse students in the pathway. To maximize impact and accelerate students’ ultimate trajectory toward health profession graduate schools, pathway programs should focus on preparing competitive applicants able to progress to the next educational level, 34 which can be achieved by focusing on academic enrichment, academic support, research opportunities, and college preparation. This pathway program development guide can help residency programs create successful partnerships with local schools, align student needs with program goals, apply an evidence-informed framework to curriculum development, and plan a well-designed evaluation that can help demonstrate impact to sustain and expand such programs. By implementing these programs in residencies, academic family medicine can grow a diverse primary care workforce that can care for the diverse needs of communities. 9, 14
Presentations
Preliminary components of this manuscript have been presented at the Society of Teachers of Family Medicine Annual Spring Conference, 2021 (Virtual) and the American Academy of Family Physicians Program Directors Workshop and Residency Program Solutions Residency Education Symposium, 2020 (Virtual).
Acknowledgments
We are grateful to the UCLA family medicine residents and past graduates, staff, and faculty who have been involved in the implementation and ongoing delivery of the UCLA FM Bridging the Gap Program. We are grateful to student participants, teachers, and high school leadership, from whom we learned and who were integral to the enrichment of the program. We are also grateful to the University of Wisconsin–Madison Department of Family Medicine Scientific Editor, Rachel Lundwall, for her review and helpful insights that improved the quality of our manuscript.
References
-
Association of American Medical Colleges. Table B-64: total U.S. MD-granting medical school graduates by race/ethnicity (alone) and gender, 2018- 2019 through 2022-2023. July 25, 2023. Accessed July 7, 2024.
https://www.aamc.org/media/6121/download
-
Martínez LE, Anaya YB-M, Santizo Greenwood S, Diaz SFM, Wohlmuth CT, Hayes-Bautista DE. The Latino resident physician shortage: a challenge and opportunity for equity, diversity, and inclusion.
Acad Med. 2022;97(11):1,673-1,682.
doi:10.1097/ACM.0000000000004793
-
Gonzalez CM, De Leon E. A call to promote interventions for increased diversity in health professions programs-beyond trends.
JAMA Netw Open. 2023;6(12):e2347852.
doi:10.1001/jamanetworkopen.2023.47852
-
Jetty A, Jabbarpour Y, Pollack J, Huerto R, Woo S, Petterson S. Patient-physician racial concordance associated with improved healthcare use and lower healthcare expenditures in minority populations.
J Racial Ethn Health Disparities. 2022;9(1):68-81.
doi:10.1007/s40615-020-00930-4
-
Goodfellow A, Ulloa JG, Dowling PT, et al. Predictors of primary care physician practice location in underserved urban or rural areas in the United States: a systematic literature review.
Acad Med. 2016;91(9):1,313-1,321.
doi:10.1097/ACM.0000000000001203
-
Xierali IM, Nivet MA. The racial and ethnic composition and distribution of primary care physicians.
J Health Care Poor Underserved. 2018;29(1):556-570.
doi:10.1353/hpu.2018.0036
-
Majerczyk D, Behnen EM, Weldon DJ, et al. Racial, ethnic, and sex diversity trends in health professions programs from applicants to graduates.
JAMA Netw Open. 2023;6(12):e2347817.
doi:10.1001/jamanetworkopen.2023.47817
-
-
-
-
Muppala VR, Janwadkar RS, Rootes A, Prakash N. Creating a pipeline for minority physicians: medical-student-led programming.
Cureus. 2021;13(4):e14384.
doi:10.7759/cureus.14384
-
-
Valla JM, Williams WM. Increasing achievement and higher-education representation of under-represented groups in science, technology, engineering, and mathematics fields: a review of current K-12 intervention programs.
J Women Minor Sci Eng. 2012;18(1):21-53.
doi:10.1615/JWomenMinorScienEng.2012002908
-
-
-
-
-
-
-
Patterson DG, Carline JD. Promoting minority access to health careers through health profession-public school partnerships: a review of the literature.
Acad Med. 2006;81(6 suppl):S5-S10.
doi:10.1097/01.ACM.0000225247.84379.9c
-
-
-
National Academies of Sciences, Engineering, and Medicine. Equity in K-12 STEM Education: Framing Decisions for the Future. National Academies Press; 2025.
-
-
-
Campbell KM, Rodríguez JE. Addressing the minority tax: perspectives from two diversity leaders on building minority faculty success in academic medicine.
Acad Med. 2019;94(12):1,854-1,857.
doi:10.1097/ACM.0000000000002839
-
-
Anaya YB, Sur D. Development and implementation of pipeline programs to shape aspirations and build confidence in underserved youth. Presented at: American Academy of Family Physicians Program Directors Workshop and Residency Program Solutions Residency Education Symposium, Virtual On Demand Workshop; 2020; Kansas, City, MO.
-
Anaya YB, Abdi R. Shaping aspirations and building confidence in underserved youth through high school & residency partnership pipeline programs. Presented at: Society of Teachers of Family Medicine Annual Spring Conference; 2021; Virtual.
-
Thomas P, Kern D, Hughes M, Chen B.
Curriculum Development for Medical Education. A Six-Step Approach. 3rd ed. Johns Hopkins University Press; 2016.
doi:10.1353/book.44600
-
Foster KE, Robles J, Anim T, et al. What do underrepresented in medicine junior family medicine faculty value from a faculty development experience?
Fam Med. 2022;54(9):729-733.
doi:10.22454/FamMed.2022.895447
-
Breese AC, Nickerson AB, Lemke M, et al. Examining implicit biases of pre-service educators within a professional development context.
Contemp Sch Psychol. 2023;27(4):1-16.
doi:10.1007/s40688-023-00456-6
-
National Academies of Sciences, Engineering, and Medicine. Promising practices for addressing the underrepresentation of women in science, engineering, and medicine: opening doors. Proceedings of a symposium-in brief. National Academies Press; 2020.
-
-
Kirkpatrick DL, Kirkpatrick JD. Evaluating Training Programs: The Four Levels. 3rd ed. Berrett-Koehler Publishers; 2006.
-
Blanco M, Prunuske J, DiCorcia M, Learman LA, Mutcheson B, Huang GC. The DoCTRINE guidelines: defined criteria to report INnovations in education.
Acad Med. 2022;97(5):689-695.
doi:10.1097/ACM.0000000000004634
-
Moreno G, Rodríguez MA, Lopez GA, Bholat MA, Dowling PT. Eight years of building community partnerships and trust: the UCLA family medicine community-based participatory research experience.
Acad Med. 2009;84(10):1,426-1,433.
doi:10.1097/ACM.0b013e3181b6c16a



There are no comments for this article.