Background and Objectives: The choice of specialty by medical students is pivotal for their careers and the health care system. The shortage of trained medical providers makes this choice particularly salient in Africa. Understanding the motivations and preferences of African medical students can inform interventions to improve the distribution and retention of doctors across specialties and regions. This study aims to explore the factors influencing specialty selection among medical students across Africa using a cross-sectional, mixed-methods approach.
Methods: A survey conducted from June to October 2023 included 1,044 students from 152 medical schools. Descriptive statistics summarized sample characteristics, and linear regression models identified predictors of primary care selection. Thematic analysis was performed on qualitative data.
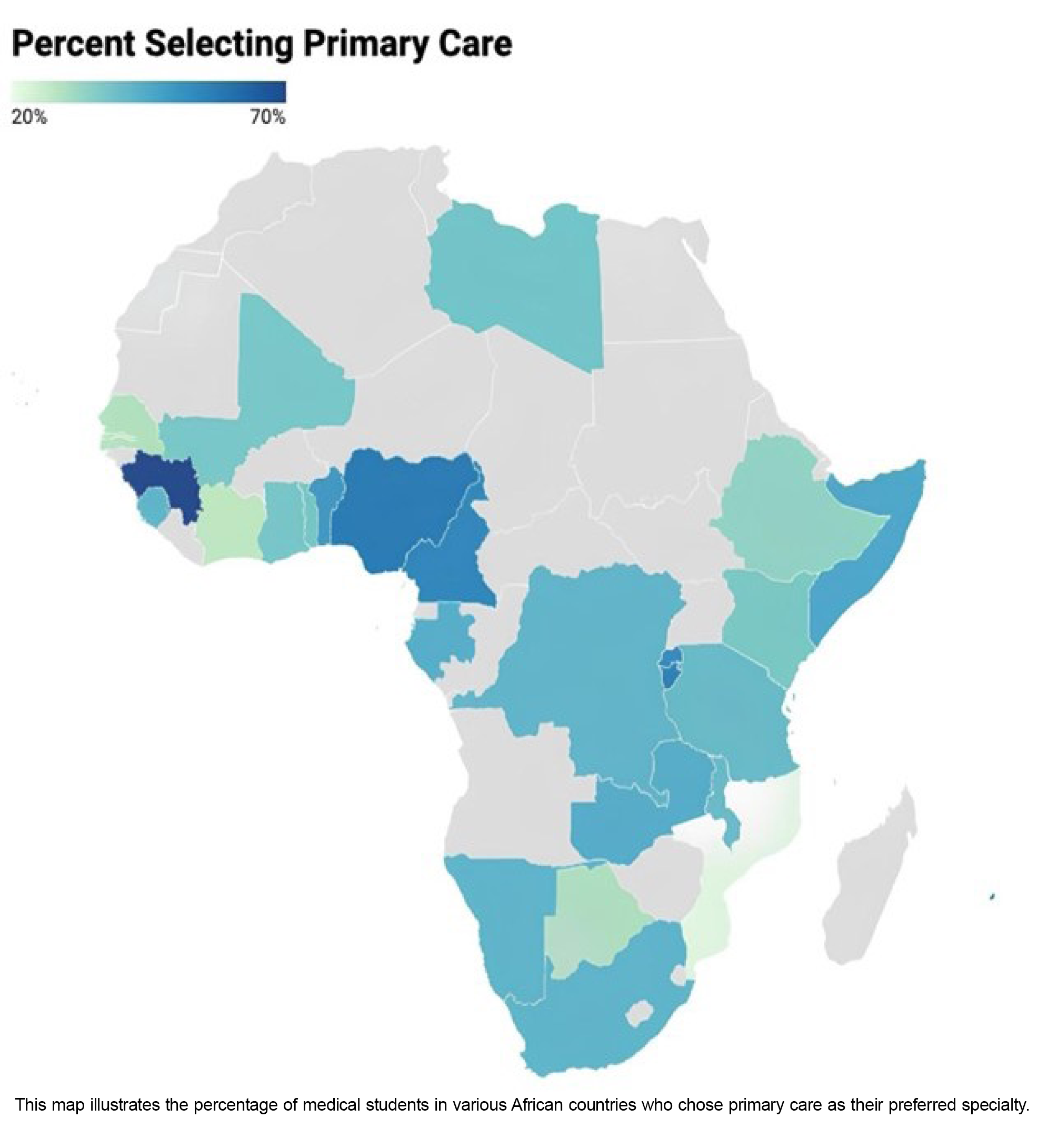
Results: Students interested in primary care were, on average, older and reported higher anxiety levels compared to their counterparts. Key factors influencing specialty choice across all students included personal interest, scope of practice, and intellectual stimulation, with prestige being least important for those choosing primary care. Additionally, the importance of mentorship was lower among primary care aspirants. Country-specific analysis revealed that students from Benin, Botswana, Ivory Coast, Senegal, and Sierra Leone were more likely to choose primary care.
Conclusions: This study provides an overview of the motivations behind specialty choice among African medical students, highlighting the need for tailored interventions to address regional health care needs. Understanding these preferences can help in designing strategies to enhance the distribution and retention of medical professionals in various specialties, ultimately improving health care outcomes.
Medical students’ choice of specialty is a key decision that heavily affects their future career and, in aggregate, the health care system. The severe shortage of primary care physicians in Africa poses a significant challenge to achieving equitable health care outcomes across the continent. 1 Primary care serves as the cornerstone of effective health systems, yet its underrepresentation in medical specialties exacerbates health care disparities, particularly in underserved regions. Despite the need for trained medical providers in Africa, evidence is limited on the factors that influence medical students’ specialty choices.1 Understanding the motivations and preferences of African medical students is essential for shaping targeted interventions to improve the distribution and retention of doctors across different specialties and regions.
While substantial information is available on specialty choice in high-income countries, comprehensive and comparative data on the specialty preferences and motivations of medical students in lower-middle income countries (LMICs) are scarce.2, 3 Research in high-income countries has extensively explored factors influencing specialty choice, such as personal interest, lifestyle considerations, income potential, and the influence of role models and mentors. A recent scoping review explored willingness to pursue different specialties through the lens of gender but did not discuss differing motivations for primary care. 4 However, the findings are not easily generalizable to LMICs due to different socioeconomic and health care contexts.
Several studies have attempted to understand the specialty choices of medical students in LMICs. For example, Puertas et al conducted a systematic review highlighting the significant influence of socioeconomic factors, educational environment, and health care infrastructure on students’ career choices in high-, middle-, and low-income countries.3 Notably, specific factors such as understanding “rural needs” and “intellectual challenge” were more relevant in middle- and low-income countries, while high-income countries placed more emphasis on attitudes toward social problems, voluntary work, family influence, and residency length. In other African studies, specific challenges such as the migration of health care workers, the burden of infectious and noncommunicable diseases, and limited resources and faculty further complicate these decisions.5, 6 Assessments of specialty choice among Nigerian students found good knowledge of community medicine/primary care but a lack of interest in pursuing those specialties.7 Another study found most students were drawn to specialty training but relatively few were ultimately able to pursue their preferred initial choice. 8
Despite these insights, most existing studies are limited by small sample sizes, single-country or single-institution focus, or outdated information. An immense need exists to capture the current trends and motivations underlying the specialty choice of African medical students. This study aims to address this gap by exploring the elements that affect medical students’ specialty selection throughout Africa (including LMICs as well as upper-middle income countries) using a cross-sectional, mixed-methods approach.
We conducted a cross-sectional survey study from June to October 2023. The study was approved by the Institutional Review Board of St Paul’s Hospital Millennium Medical College in Ethiopia, which provided oversight for the research conducted across participating countries. All procedures were conducted in accordance with the ethical principles outlined in the Declaration of Helsinki.
The study population included medical students enrolled in 152 medical schools across 36 African countries. Participants had to be proficient in either English or French and could not be on leave or have graduated from medical school. Participants were from the following countries: Benin, Botswana, Burkina Faso, Burundi, Cameroon, Central African Republic, Democratic Republic of Congo, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Ivory Coast, Kenya, Liberia, Libya, Malawi, Mali, Mauritius, Morocco, Mozambique, Namibia, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, Somalia, South Africa, South Sudan, Tanzania, Togo, Uganda, Zambia, and Zimbabwe.
We employed a convenience sampling approach, supplemented by snowball sampling techniques, both at the participant level. This survey was distributed via online platforms such as WhatsApp and Telegram, both of which are used commonly among this population and demographic. The survey was distributed specifically through the International Federation of Medical Students Association channels and referrals. However, we could not secure data collection from every country. Respondents were encouraged to share the survey link with their networks to increase sample diversity. In general, social media use throughout Africa varies, but WhatsApp is the most commonly used social messaging application.9 According to downloading data from a mobile technology company, more than 95% of the population in countries such as Kenya, South Africa, and Nigeria are using the app, and 44% of all mobile Internet use in the country of Zimbabwe is used on WhatsApp. 9
The online survey was administered using Google Forms and consisted of three sections: demographic information, academic and professional motivations, and factors influencing specialty choice. Using a 5-point Likert scale, students rated the importance of 11 different factors in choosing their specialty. We used descriptive statistics to summarize sample characteristics and factors influencing the choice of primary care specialties. Thematic analysis of the qualitative data followed the six steps proposed by Braun and Clarke. 10
Primary care has been defined as “first-contact, continuous, comprehensive and coordinated care provided to populations,” and “the [primary care physician] should provide total care for the majority of patients’ complaints and be willing to care for patients in the appropriate setting.”11, 12 These were some of the definitions used in our study to delineate which students qualified as being interested in a primary care specialty. A student was categorized as interested in primary care if they responded with one of the following specialties in an open-ended question about which specialty they were planning to pursue: primary care, family medicine, internal medicine, emergency medicine, pediatrics, public health, sports medicine, psychiatry, nutrition, or preventative health care. Students who responded with a subspecialty of internal medicine (eg, cardiology, gastroenterology) were not included in the primary care group, nor were any students who reported other specialties of interest, such as general surgery, obstetrics and gynecology, or neurology (among others).
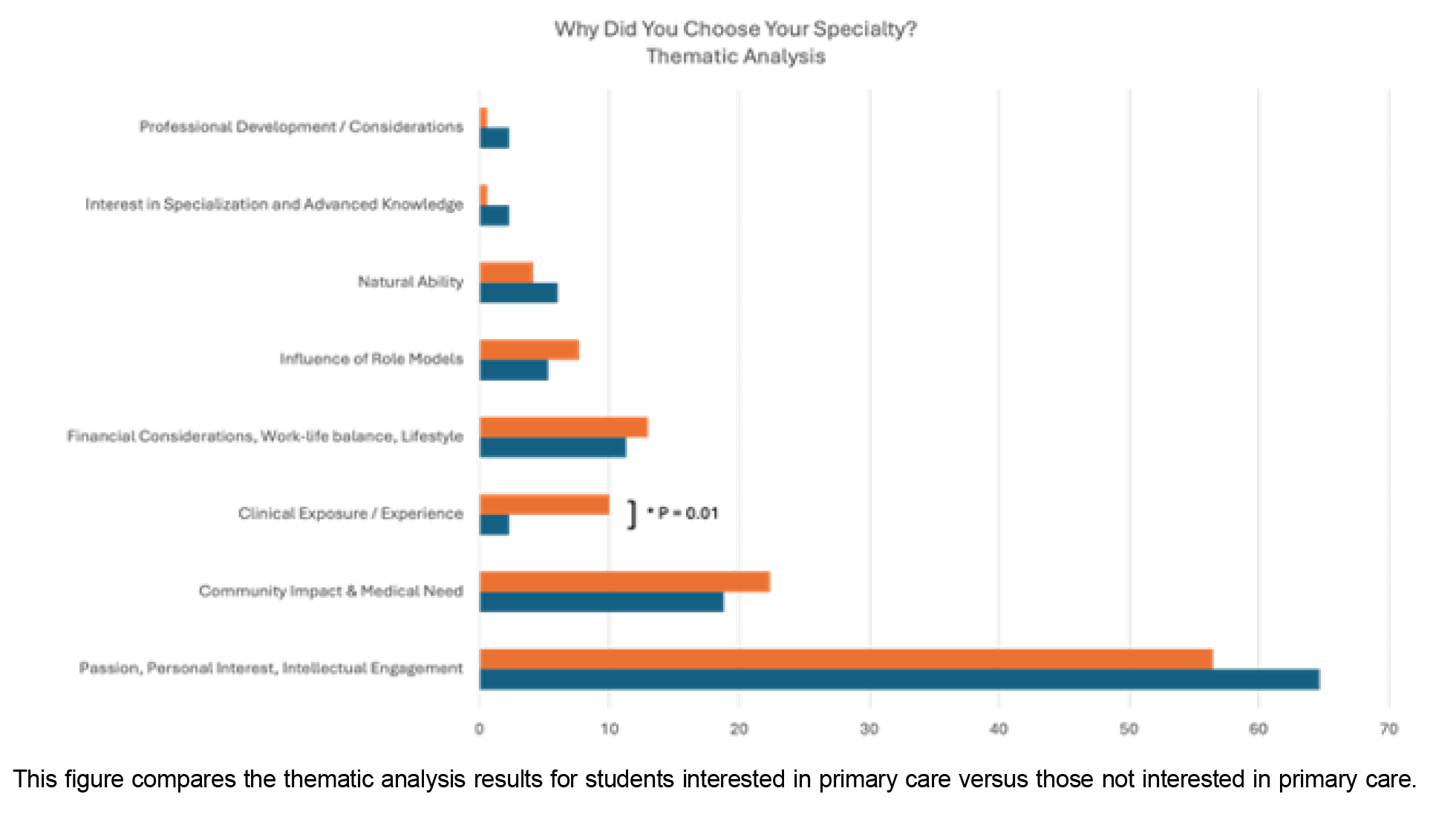
We employed various statistical methods to analyze the data. We used descriptive statistics to provide a summary of the sample characteristics and the factors influencing specialty choice. We used linear regression models to identify predictors of primary care selection, reported in terms of odds ratios, 95% confidence intervals, and P values. We performed additional linear regressions to compare outcomes across countries, with Togo serving as the reference country due to the highest number of responses (N=90). Countries were included in the analysis if their sample size exceeded 10 students. We used ꭓ2 tests, Mann-Whitney U and Wilcoxon rank-sum tests, and linear regression models to compare choices among groups of students interested and not interested in primary care (Figure 1). We set statistical significance at P<.05, and the reporting adhered to STROBE guidelines to ensure the accuracy and transparency of the findings.
Demographics and Descriptive Statistics
Our sample consisted of 1,044 medical students from 152 medical schools in Africa (Figure 2). The average age of the sample was 23.2, and 51.6% of participants were female. Students interested in primary care specialties were older on average than those not interested in primary care specialties (23.5 vs 22.9 years old; Table 1). We found no significant differences in gender, marital or relationship status, parental status, alcohol use, smoking, or drug use.
|
Variable
|
Total
sample
|
Primary
care
|
Other
specialty
|
|
Average
age
(in years)
|
23.2
|
23.5
|
22.9
|
|
|
n (%)
|
n (%)
|
n (%)
|
|
Phase of
training
|
|
Preclinical
|
337 (32.6)
|
88 (33.2)
|
177 (66.8)
|
|
Clinical
|
698 (67.4)
|
236 (43.9)
|
301 (56.1)
|
|
Gender
|
|
Male
|
499 (48.1)
|
162 (38.5)
|
259 (61.5)
|
|
Female
|
538 (51.9)
|
163 (42.3)
|
222 (57.7)
|
|
Language of
survey
|
|
English
|
785 (75.2)
|
242 (40.1)
|
362 (59.9)
|
|
French
|
259 (24.8)
|
82 (41.4)
|
116 (58.6)
|
|
GNI of
country
|
|
Lower income
|
360 (46.9)
|
41.10
|
58.90
|
|
Lower-middle income
|
277 (36.1)
|
38.60
|
61.40
|
|
Upper-middle income
|
130 (16.9)
|
42.30
|
57.70
|
Students interested in primary care specialties had a higher reported history of anxiety compared to those not interested in primary care specialties (χ2=8.2916, P<.01). In a linear model, age was the only predictive factor of choosing a primary care specialty, indicating that older students were more likely to choose primary care (β=0.015, SE=0.007, P<.05).
Choosing Primary Care
Students across all specialties and countries ranked the following factors with similar importance: prestige, income, ability to work part-time, exposure to the specialty, time for family, mentors, time for leisure activities and lifestyle, intellectual stimulation, personal interest in the specialty, predictable work hours, and scope of practice. However, the importance of a mentor was less important to those students choosing primary care specialties (P<.05).
The most important factors among students interested in primary care were personal interest in the field, scope of practice, and intellectual stimulation. Prestige was the least important factor for these students.
In a linear model testing predictors of primary care interest by country, students from five countries were more likely to show interest in careers in primary care: Benin (β=0.202, SE=0.102, P<.05), Botswana (β=0.416, SE=0.166, P<.05), Ivory Coast (β=0.282, SE=0.118, P<.05), Senegal (β=0.272, SE=0.130, P<.05), and Sierra Leone (β=0.249, SE=0.082, P<.01).
Thematic Analysis
The most endorsed theme surrounded passion, interest, and intellectual engagement with the specialty and specialty-related material (64.7% of respondents interested in primary care, 56.5% of those not interested in primary care; Table 2). The second most referenced theme for those wanting to go into primary care was the community impact and medical need of this specialty (18.8%).
|
Theme
|
% of responses
|
Representative
quotes
|
|
Passion, personal interest, intellectual engagement
|
64.7
|
“Am fascinated by the family and everything related to it.”
“I just know that internal medicine requires so much thinking and analyzing, which I’m good at.”
“Dream of childhood for pediatrics, so internal medicine has become a passion I feel comfortable in logic.”
|
|
Community impact and medical need
|
18.8
|
“Because these are areas in my country that have huge gaps and I feel it’s relevant to contribute to health care development in my country.”
“Because this specialty is my country’s current need.”
“To help the current suffering population without a proper medical management of simple diseases.”
“I am just interested in making an impact where it’s needed the most in my country.”
“Because I wish I can build a change in the society based on the issues that I usually observe in the surrounding area.”
|
|
Financial considerations, work-life balance, lifestyle
|
11.3
|
“Passion accompanied by monetary benefits.”
“Public health because I like money.”
|
|
Natural ability
|
6.0
|
“I’ve always felt like I was very good with kids, and people always tell me I’m very good with children.”
|
|
Influence of role models
|
5.3
|
“The fact that I was faced with great teachers and that it had interesting subject matter is a plus.”
“I was inspired by a teacher.”
“My role model is a pediatrician and I got inspired.”
|
|
Clinical exposure/experience
|
2.3
|
“I’ve always enjoyed every internal medicine class I’ve had, as they always felt like investigative medicine: finding the exact root cause(s) of why a patient decided to come to the hospital. I like that it employs my critical thinking and problem-solving skills.”
“I was satisfied with my internship in these services.”
|
|
Interest in specialization and advanced knowledge
|
2.3
|
“Because I want to be a specialist.”
“To deepen the knowledge of medicine to acquire expertise in a specific field.”
|
|
Professional development/considerations
|
2.3
|
“I want to be an academic.”
“The prestige that comes with it.”
“To be among the best.”
|
Of those wanting to pursue fields other than primary care, 10% of respondents noted that some form of clinical experience or exposure to that specialty in medical school influenced their decision, whereas only 2% of students interested in primary care endorsed clinical exposure as influential (P=.01).
The choice of specialty is influenced by many personal, educational, and contextual factors. Some commonly cited factors in Western medical students are interest, lifestyle, role models, social responsibility, financial incentives, and prestige.13-15 However, these factors may vary in importance and relevance across different settings and cultures.13 African medical students face unique challenges, such as faculty shortages, resource limitations, the burden of infectious and noncommunicable diseases, health care worker migration, and emerging public health needs. 5, 6, 16
The main objective of this study was to explore the factors influencing medical students’ career choices in primary care specialties. Students’ preferences for primary care were shaped by personal interest, intellectual stimulation, and perceived scope of practice. Prestige and income were less influential, consistent with findings that intrinsic rewards and societal impact drive interest in primary care.17 This finding suggests that medical schools and policymakers should focus on promoting the intrinsic rewards and societal impact of primary care to retain students in this field. Additionally, increasing the prestige and monetary pay of primary care specialties may serve to attract a broader pool of applicants to the field.
The thematic analysis provides further insights into the motivations and aspirations of medical students considering primary care. The overwhelming endorsement of passion, interest, and intellectual engagement with the specialty highlights the importance of aligning students’ personal values and interests with their career choices. Furthermore, the emphasis on community impact and medical need suggests that students are driven by a desire to make a meaningful contribution to society through their work.
Our findings have several implications for medical education and policy. First, medical schools should prioritize exposing students to primary care early in their training through clinical rotations, mentorship programs, and community engagement opportunities. This exposure will help students develop a better understanding of the scope of practice, challenges, and rewards of primary care. Second, medical schools and policymakers should develop targeted strategies to attract and retain students. These strategies may involve providing financial incentives, scholarships, or other forms of support to encourage students to pursue primary care careers.
The qualitative analysis revealed several interesting trends. One notable trend is the role that clinical exposure or experience plays in helping students choose a specialty. Clinical experience and exposure were endorsed by 10% of those not interested in primary care specialties, compared to only 2% of those interested in primary care. This finding is consistent with a review of family medicine understanding in Egypt, which found that increased curriculum exposure improved knowledge of family medicine but did not impact intentions to pursue the specialty.18 Distinguishing the lack of positive endorsement of clinical factors from endorsement of a negative effect of clinical factors is important. In our study, we can say only that students are not often endorsing positive clinical experiences as a primary reason to pursue their field, indicating that other factors are more important. This finding does not mean that clinical factors are unimportant or that they detract from students’ desire to go into the field. Every medical student is exposed to primary care by the very nature of it being a core part of medical education. In this way, clinical exposure alone is less likely to be a driving factor in someone’s choice of primary care as a specialty, especially in comparison to fields like neurosurgery or ophthalmology, where exposure is not guaranteed in medical school and strongly predicts a student’s interest in those specialties.19- 21 Therefore, focusing on increasing exposure to primary care specialties for students may not be pertinent, because this is likely already addressed through mandatory medical school rotations. Instead, focusing on other domains of the specialty, such as prestige, intellectual engagement, financial status, and community need, may be more effective in increasing medical student interest in primary care. 2
For example, many students across the sample, regardless of specialty choice, mentioned the desire to help their community by providing much-needed care in areas where care is scarce. Emphasizing community need by getting students involved in outreach programs, such as free hypertension screenings or pediatric physicals in primary schools, may be important for training programs trying to develop interest in primary care specialties. Similarly, a more effective approach may be to focus on identifying and admitting students with a preexisting passion for primary care and community engagement rather than attempting to generate interest among current medical students. If students who are passionate about primary care and public health could be identified and encouraged to apply to medical school, or if pathways could be created to remove barriers for these students to attend medical school, these efforts could have a significant impact. We have outlined specific recommendations for each stakeholder level in Table 3.
|
Recommendation
domain
|
Specific
examples
|
|
Clinical
|
Implement outreach programs such as free hypertension screenings in underserved areas. Provide medical students with early and ongoing exposure to primary care clinics and community health settings.
|
|
Academic
|
Integrate primary care-focused courses and electives into the medical school curriculum. Promote mentorship programs where students can connect with primary care physicians who are role models.
|
|
National
|
Develop national policies to improve the working conditions and financial incentives for primary care practitioners. Support initiatives that highlight the importance of primary care in addressing national health crises.
|
|
International
|
Foster international collaborations to provide resources, training, and exchange programs for primary care competencies. Leverage global health partnerships to create scholarships and grants for students committed to primary care.
|
We do not mean to downplay the importance of positive clinical experiences and are cognizant of the high levels of burnout in primary care settings. Addressing burnout is crucial for creating better clinical environments that inspire students. In our study, many students who desired a career in primary care noted an intellectual engagement with and passion for primary care that may have started prior to medical school. Programs that mirror initiatives in the United States, such as special tracks or scholarships for students applying with a focus on primary care, may help cultivate interest. Identifying and supporting these students early could prove more impactful than increasing clinical exposure during medical school.
This study had several important limitations. First, the diversity across African countries means that medical education systems, health care infrastructure, and cultural factors vary significantly. These differences can influence medical students’ specialty choices in ways that are not fully captured in our study. Second, the sample sizes from each country were relatively small, limiting our ability to compare effectively between sites; the results may not be representative within any given country, particularly in nations with more heterogeneous populations or varied regional characteristics. Third, we were unable to compare survey demographics with regional demographics of medical students and were unable to assess the representativeness of our sample. To that end, we received survey responses from medical students in 36 countries throughout Africa but included only 27 countries in any intra-country analyses due to sample sizes that limited the generalizability of the additional nine countries (those with less than 10 responses). However, because our survey was distributed in two languages, French and English, it allowed for wider-spread sampling than a survey in a single language. Additionally, combining multiple specialties under the umbrella of “primary care” may have affected the interpretation of students’ preferences
Lastly, we found that students interested in primary care were more likely to endorse a history of anxiety. This finding requires further exploration. A potential misalignment between the question’s intent and students’ interpretation may have influenced responses. For example, students may have interpreted the question as asking about general anxiety rather than a clinically diagnosed condition. Therefore, while intriguing, this finding should be approached with caution and explored further in future research. These limitations suggest that while our findings provide valuable insights, further research with larger, more representative samples and more rigorous sampling methods is needed to better understand the factors influencing medical specialty choices across different African contexts.
Overall, our study contributes to the understanding of the factors influencing medical students' career choices in Africa and provides a valuable snapshot for stakeholders involved in medical education and health care policy. By addressing the needs and aspirations of medical students, we can ensure a sustainable and effective primary care workforce that meets the health care needs of communities across the region.
References
-
Ahmat, A, Okoroafor SC, Kazanga I, et al. The health workforce status in the WHO African Region: findings of a cross-sectional study.
BMJ Glob Health. 2022;7(Suppl 1).
doi:10.1136/bmjgh-2021-008317
-
-
Puertas EB, Arósquipa C, Gutiérrez D. Factors that influence a career choice in primary care among medical students from high-, middle-, and low-income countries: a systematic review. Rev Panam Salud Publica. 2013;34(5):351-358.
-
Levaillant M, Levaillant L, Lerolle N, Vallet B, Hamel-Broza J-F. Factors influencing medical students’ choice of specialization: a gender based systematic review.
eClinicalMedicine. 2020;28:100589.
doi:10.1016/j.eclinm.2020.100589
-
Silvestri DM, Blevins M, Wallston KA, et al. Nonacademic attributes predict medical and nursing student intentions to emigrate or to work rurally: an eight-country survey in Asia and Africa.
Am J Trop Med Hyg. 2017;96(6):1,512-1,520.
doi:10.4269/ajtmh.16-0756
-
Krishnaswami S, Nwomeh BC, Ameh EA. The pediatric surgery workforce in low- and middle-income countries: problems and priorities.
Semin Pediatr Surg. 2016;25(1):32-42.
doi:10.1053/j.sempedsurg.2015.09.007
-
Ugwunna NC, Okeke AJ, Okeke CP, et al. Perception and attitude of medical students in UNEC towards community medicine as a career choice.
Eur J Public Health. 2020;30(Suppl 5):ckaa166.650.
doi:10.1093/eurpub/ckaa166.650
-
Ossai EN, Uwakwe KA, Anyanwagu UC, Ibiok NC, Azuogu BN, Ekeke N. Specialty preferences among final year medical students in medical schools of southeast Nigeria: need for career guidance.
BMC Med Educ. 2016;16(1):259.
doi:10.1186/s12909-016-0781-3
-
-
-
Cantor J.
Primary Care: Concept, Evaluation, and Policy. Starfield B, New York, NY, Oxford University Press, Inc, 1992, paperback, 254 pp, $18.95.
J Phys Ther Educ. 1993;7(2):80-81.
doi:10.1097/00001416-199307000-00024
-
Jimenez G, Matchar D, Koh GCH, et al. Revisiting the four core functions (4Cs) of primary care: operational definitions and complexities.
Prim Health Care Res Dev. 2021;22:e68.
doi:10.1017/S1463423621000669
-
Alamri AA, Alshehri KA, Alharbi AA, et al. Factors influencing the choice of otolaryngology (ORL) head and neck surgery as a future specialty for Saudi medical students.
J Family Med Prim Care. 2019;8(6):1,941-1,946.
doi:10.4103/jfmpc.jfmpc_414_19
-
Alhussain, AA. Effect of Anticipated Lifestyle and Income on Medical Students’ Decision to Pursue a Primary Care Career in Saudi Arabia. Dissertation. University of South Carolina; 2021.
-
Bland CJ, Meurer LN, Maldonado G. Determinants of primary care specialty choice: a non-statistical meta-analysis of the literature.
Acad Med. 1995;70(7):620-641.
doi:10.1097/00001888-199507000-00013
-
Draper C, Louw G. What is medicine and what is a doctor? medical students’ perceptions and expectations of their academic and professional career.
Med Teach. 2007;29(5):e100-e107.
doi:10.1080/01421590701481359
-
-
AlKot MM, Gouda MA, KhalafAllah MT, Zahran MS, Kallaf MM, Zayed AM. Family medicine in Egypt from medical students’ perspective: a nationwide survey.
Teach Learn Med. 2015;27(3):264-273.
doi:10.1080/10401334.2015.1044654
-
Yoon JD, Ham SA, Reddy ST, Curlin FA. Role models’ influence on specialty choice for residency training: a national longitudinal study.
J Grad Med Educ. 2018;10(2):149-154.
doi:10.4300/JGME-D-17-00063.1
-
Li J. Plastic surgery or primary care? altruistic preferences and expected specialty choice of U.S. medical students.
J Health Econ. 2018;62:45-59.
doi:10.1016/j.jhealeco.2018.09.005
-
Maiorova T, Stevens F, Scherpbier A, van der Zee J. The impact of clerkships on students’ specialty preferences: what do undergraduates learn for their profession?
Med Educ. 2008;42(6):554-562.
doi:10.1111/j.1365-2923.2008.03008.x



There are no comments for this article.