Background and Objectives: The National Institutes of Health and related federal awards for research training (RT) and research career development (RCD) are designed to prepare applicants for research careers. We compared funding rates for RT and RCD for anesthesiology, dermatology, emergency medicine, family medicine, internal medicine, neurology, obstetrics-gynecology, pathology, pediatrics, and psychiatry.
Methods: We estimated the denominator using the number of residency graduates from different specialties from 2001 to 2010 from the Association of American Medical Colleges data. For the numerator, we used published data on federally funded awards by specialty from 2011 to 2020. We also examined the correlation between RCD funding and overall research funding.
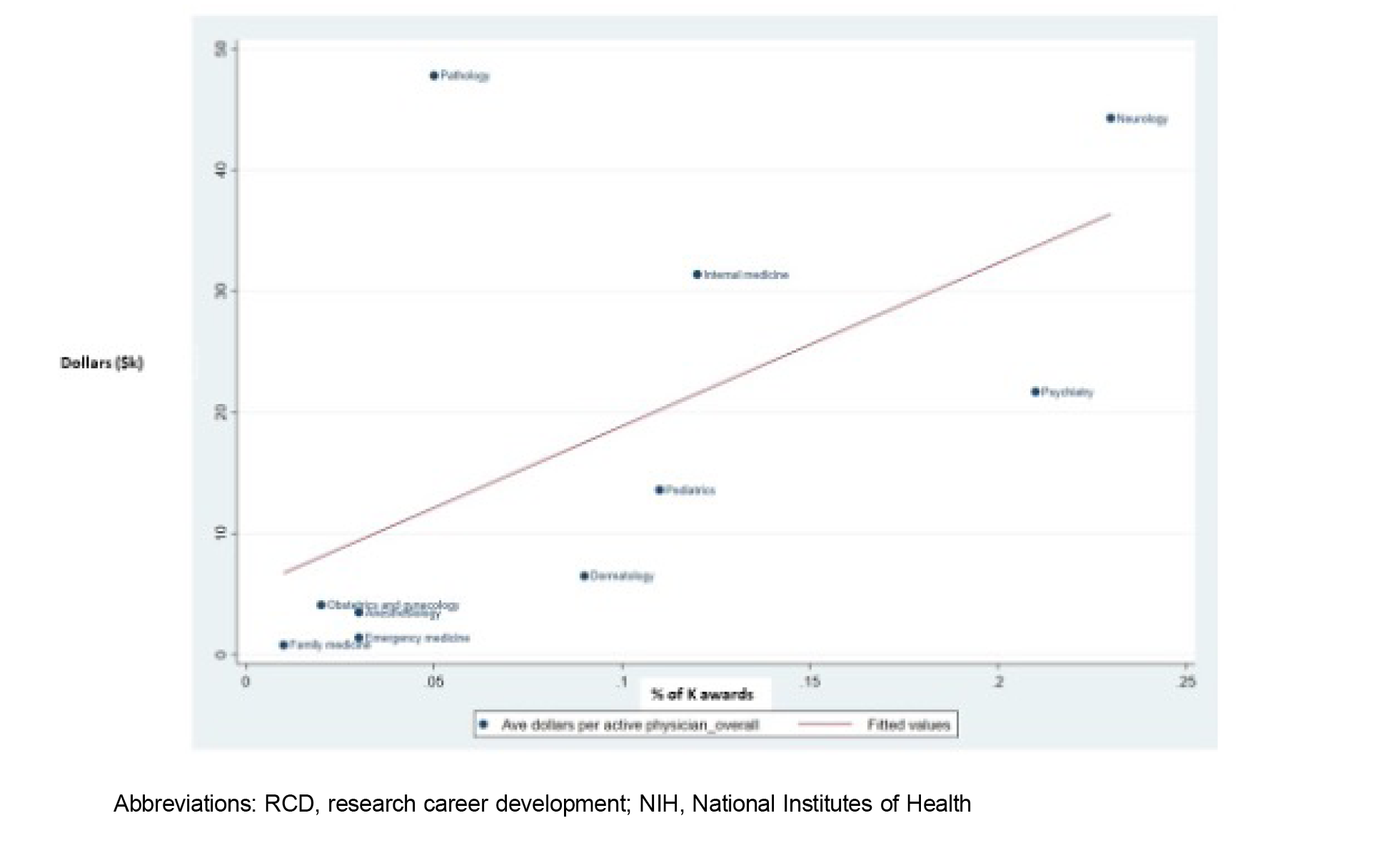
Results: Family medicine had the lowest rate per graduating resident for RT (0.01%) and RCD (0.77%) awards among 10 specialties and was lower than the mean/median for the other nine specialties, ranging from 2.15%/1.19% and 9.83%/8.74%. We found a strong correlation between rates of RCD awards and mean federal funding per active physician, which was statistically significant (ρ=0.77, P=.0098).
Conclusions: Comparatively low rates for family medicine awards for RT and RCD plausibly contribute to poor federal funding for family medicine research, underscoring the need to bolster the research career pathway in family medicine.
Research is critical to informing the future of health care and primary care. 1 Historically, family medicine has had low rates of National Institutes of Health (NIH) and other federal research funding compared to other specialties. 2, 3 Yet, knowledge regarding the contribution of research training (RT) and research career development (RCD) to low federal research funding for family medicine is lacking. The NIH, the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Disease Control (CDC) provide competitive funding for RT awards (F32 and T32) and RCD awards (K01, K08, and K23) to create a pathway for independent NIH-funded researchers. 4
We examined two hypotheses: (1) Family medicine receives fewer RT and RCD awards per residency graduate than other specialties, and (2) the number of RCD awards is associated with total federally funded research per active physician within specialties.
No ideal way is available to compare research funding by specialty. Our first outcome variable was the number of RT and RCD awards in the ensuing 10 years per graduating resident in each of 10 specialties (anesthesiology, dermatology, emergency medicine, family medicine, internal medicine, neurology, obstetrics-gynecology, pathology, pediatrics, and psychiatry). We used a numerator from published data derived from the NIH RePORTER on the number of RT and RCD awards and academic departments (specialties) from 2011 to 2020—that is, awards to individuals and their department affiliation listed on their application. 5 Our denominator was the number of graduating residents in each specialty in the preceding 10 years based on the Association of American Medical Colleges data. 6, 7 We also did a sensitivity analysis, replacing residency graduates in the denominator with the number of faculty in each specialty from 2011 to 2020.
We also examined the correlation between the total research funding per specialty from 2011 to 2020 per practicing physician as reported by Schlafly et al 5 (Table 1, last column), with two outcomes as reported by Nguyen et al. 8 Our first outcome was total RCD awards, which included any RCD award (K01, K08, K23). Our second outcome was percentage of successful transition of RCD by specialty to independent research (R) funding. We performed a Spearman's correlation to assess the relationships and used a P value of <.10 to determine statistical significance. We verified the number of family medicine RCD awardees and spot-checked awards to other disciplines by individually searching the NIH RePORTER to confirm numbers. We matched awardee names with academic degrees (via an internet search). All data used were publicly accessible, exempting this study from review by our institutional review board.
|
Specialty
|
RT a (T32) %
|
RCD b (K01) %
|
RCD (K08) %
|
RCD (K23) %
|
Total RCD c (Any K) %
|
K to R d %
|
Total funding e ($K)
|
|
Anesthesiology
|
0.45
|
0.55
|
1.74
|
1.32
|
3.16
|
38.40
|
3.5
|
|
Dermatology
|
1.19
|
2.70
|
5.41
|
1.81
|
8.74
|
50.70
|
6.5
|
|
Emergency medicine
|
0.04
|
0.10
|
0.64
|
1.89
|
2.59
|
41.70
|
1.4
|
|
Family medicine
|
0.01
|
0.41
|
0.11
|
0.25
|
0.77
|
26.60
|
0.8
|
|
Internal medicine
|
2.52
|
3.18
|
5.51
|
6.06
|
12.23
|
41.40
|
31.4
|
|
Neurology
|
6.56
|
4.89
|
9.83
|
14.78
|
22.93
|
42.70
|
44.3
|
|
OB/GYN
|
0.47
|
0.49
|
0.56
|
1.05
|
1.63
|
33.30
|
4.1
|
|
Pathology
|
3.48
|
2.56
|
5.30
|
0.36
|
4.75
|
44.30
|
47.8
|
|
Pediatrics
|
1.09
|
1.17
|
5.67
|
5.21
|
10.96
|
32.50
|
13.6
|
|
Psychiatry
|
3.58
|
9.07
|
3.05
|
12.94
|
21.49
|
42.00
|
21.7
|
|
Mean/median
|
2.15/ 1.19
|
2.75/ 2.56
|
4.19/ 5.30
|
5.05/ 1.89
|
9.83/ 8.74
|
40.80/ 41.70
|
19.4/ 21.7
|
Between 2011 and 2020, family medicine ranked last for RT and RCD awards per graduating resident. Only two T32s were awarded to family medicine applicants during the entire decade, so this outlier category was excluded. The family medicine funding rate for RT was 0.01%, compared to a mean/median for other specialties of 2.15%/1.19%. Overall RCD funding for family medicine RCD awards was 0.77% compared to the mean of 9.83% and median of 8.74% for the other nine specialties. Substituting the number of current faculty for graduating residents as a denominator yielded similar findings.
We found a strong positive correlation between receipt of RCD awards and mean federally funded research per active physician, which was statistically significant (ρ=0.77, P=.0098). Pathology had the highest mean funding per practicing physician ($47.8K), and family medicine had the lowest ($0.80K). We observed a moderate monotonic relationship between RCD awards per specialty per graduate and successful transition to independent funding, (ρ=0.56, P<.10). We found no relationship between the number of active physicians and the total dollar amounts of funding awarded between 2011 and 2020 per specialty.
We identified 72 unique family medicine RCD awardees from 2011 to 2020 (7.2 awardees/yr). These included 23 MD/DOs (32%), 44 PhDs (62%), and 4 MD/PhDs (6%). Nine of 48 (19%) of K01 and K08 RCDs were funded by the AHRQ or CDC, with seven of the nine being awarded to nonclinical doctoral faculty.
Using the number of residents graduating a decade before RT and RCD awards were granted in 2011 to 2020 as a benchmark, we found that family medicine had the lowest number of these awards per resident among 10 specialties. Funding for RT for family medicine was roughly 1% of the mean of other specialties and roughly 10% of the mean for RCD. Using current faculty as the denominator yielded similar results, suggesting that the number of faculty by discipline did not explain these findings. Notably, a strong positive correlation existed between disciplines receiving RCD awards and mean funding per active physician. AHRQ and CDC represented important sources of RCD funding particularly for nonclinical doctoral faculty who are not eligible for K23s.
Published data has shown that family medicine faculty ranked the lowest in transitioning from RCD awards to independent funding. 8 Findings suggest that lower RT and RCD funding contribute to low research funding for family medicine. Our findings underscore the important role of nonclinical doctoral researchers who reflect a significant opportunity for federally funded research in family medicine departments. 9
Our study had limitations. First, factors contributing to the number of graduates (or faculty) in a specialty may differ from those affecting optimal RT or RCD awards. However, the number of physicians entering a field represents a gross measure of research need, and the magnitude of the disparity suggests comparative underfunding for family medicine. Moreover, to consider only seven awardees per year adequate is implausible by any standard.
Second, no publicly available data on RT and RCD award success rates exists, and that analysis also would require a denominator for the number of these awards submitted across specialties. However, that award success alone would account for differences of this magnitude in RT and RCD rates is unlikely. Instead, these differences probably are driven primarily by differences in the number of applications submitted. These differences in the research pathway for family medicine compared to other specialties may reflect weaker departmental research infrastructure, insufficient mentoring, competing faculty demands, and fewer funding mechanisms that support primary care research. 10-17 Third, some training awards that support family medicine research faculty go to departments rather than individuals, such as a department of pediatrics that may support family medicine trainees. Last, RT, RCD, and research grants from the Veterans Administration, Department of Defense, and the Patient-Centered Outcomes Research Institute are unavailable in the NIH RePORTER and are not included in these analyses.
These findings underscore the need for adequate funding to develop departmental infrastructure and faculty mentors and to offer opportunities to support RT and RCD for family medicine trainees and junior faculty. Developing a critical mass of family medicine researchers is essential to generating the science needed to implement high-quality primary care. 3 These findings underscore the need for the partnership between the Association of Departments of Family Medicine and NAPCRG, funded by the American Board of Family Medicine Foundation, to develop a strategic plan for growing funding of family medicine research in the next 6 to 7 years. 18
In conclusion, underfunded RT and RCD pathways in family medicine contribute to low federally funded research by family medicine faculty. Targeted funding is needed to bolster the family medicine research career pathway by improving research infrastructure, preparing for training awards, mentoring, and providing relevant federal funding opportunities to improve an unrealized potential for primary care research.
References
-
National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. National Academies Press; 2023.
-
Cameron BJ, Bazemore AW, Morley CP. Lost in translation: NIH funding for family medicine research remains limited.
J Am Board Fam Med. 2016;29(5):528-530.
doi:10.3122/jabfm.2016.05.160063
-
National Academies of Sciences, Engineering, and Medicine.
Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. National Academies Press; 2021. Accessed May 4, 2021.
https://doi.org/10.17226/25983
-
Yin HL, Gabrilove J, Jackson R, Sweeney C, Fair AM, Toto R. Sustaining the clinical and translational research workforce: training and empowering the next generation of investigators.
Acad Med. 2015;90(7):861-865.
doi:10.1097/ACM.0000000000000758
-
Schlafly A, Sebro R. Does NIH funding differ between medical specialties? a longitudinal analysis of NIH grant data by specialty and type of grant, 2011-2020.
BMJ Open. 2022;12(12):e058191.
doi:10.1136/bmjopen-2021-058191
-
Brotherton SE, Rockey PH, Etzel SI. US graduate medical education, 2003-2004.
JAMA. 2004;292(9):1,032-1,037.
doi:10.1001/jama.292.9.1032
-
-
Nguyen M, Panyadahundi A, Olagun-Samuel C, et al. Transition from mentored to independent NIH funding by gender and department.
JAMA. 2023;329(24):2,189-2,190.
doi:10.1001/jama.2023.7693
-
Berg EJ, Ashurst J. Patterns of recent National Institutes of Health funding in family medicine: analysis using the NIH Research Portfolio Online Reporting Tools Expenditures and Results system.
Cureus. 2019;11(10):e5847.
doi:10.7759/cureus.5847
-
Adler L, Gabay L, Yehoshua I. Primary care physicians’ attitudes toward research: a cross-sectional descriptive study.
Fam Pract. 2020;37(3):306-313.
doi:10.1093/fampra/cmz075
-
Kohlwes J, O’Brien B, Stanley M, et al. Does research training during residency promote scholarship and influence career choice? a cross-sectional analysis of a 10-year cohort of the UCSF-PRIME internal medicine residency program.
Teach Learn Med. 2016;28(3):314-319.
doi:10.1080/10401334.2016.1155460
-
Franks AM, Petrany SM. Building a culture of scholarship within a family medicine department: a successful eight-year journey of incremental interventions following a historical perspective of family medicine research.
Med Sci Educ. 2020;31(1):75-80.
doi:10.1007/s40670-020-01107-8
-
Weidner A, Peterson LE, Mainous AG III, Datta A, Ewigman B. The current state of research capacity in US family medicine departments.
Fam Med. 2019;51(2):112-119.
doi:10.22454/FamMed.2019.180310
-
Seehusen DA, Rogers TS, Al Achkar M, Chang T. Coaching, mentoring, and sponsoring as career development tools.
Fam Med. 2021;53(3):175-180.
doi:10.22454/FamMed.2021.341047
-
Mullen R, Weidner A, Liaw W, et al. Family medicine research capacity in the USA.
Fam Pract. 2021;38(2):186-188.
doi:10.1093/fampra/cmaa119
-
Seidenberg P, Shokar N, Vera J, Weidner A, Sutter J; BRC Steering Committee. A 5-year update on the building research capacity initiative.
Ann Fam Med. 2021;19(5):471-472.
doi:10.1370/afm.2746
-
-
Asif I, Weidner A, Elwood S. Toward a unified and collaborative future: creating a strategic plan for family medicine research.
Ann Fam Med. 2023;21(3):289-291.
doi:10.1370/afm.2987



There are no comments for this article.