Background and Objectives: The US physician workforce is at a critical juncture, with a projected shortage and misdistribution of primary care physicians. Culturally and linguistically diverse states, such as California, are challenged to search for innovative approaches in medical education to address the physician needs of diverse underserved communities. The University of California recognizes this imperative and supports Programs in Medical Education (PRIME), including PRIME Leadership and Advocacy (PRIME-LA) at University of California Los Angeles (UCLA). This study examines medical education outcomes for PRIME-LA graduates versus a comparator group.
Methods: We conducted a secondary data analysis of the graduation questionnaire responses from UCLA graduates between 2018 and 2023. Our study included 97 PRIME-LA graduates and 811 comparator graduates. Primary outcomes included intentions to practice in underserved areas and intentions to care for underserved populations. Secondary outcomes included participation in experiences related to health disparities, health education, providing mentorship, and specialty of interest.
Results: A higher proportion of PRIME-LA graduates reported an intention to practice in underserved areas than the comparator group (89% vs 32%, P<.001). Intentions to care for underserved populations were higher among PRIME-LA graduates than those in the comparator group (93% vs 44%, P<.001). Family medicine is the most common specialty among PRIME-LA graduates in contrast to graduates of the comparator group (26.4% vs 6.3%, P<.001).
Conclusions: Mission-based medical education programs play a critical role in addressing the physician workforce gap in underserved communities. The PRIME-LA program may equip students with additional skills and training to address California’s physician workforce needs.
The United States continues to experience a significant increase in racial and ethnic diversity, and California continues to have the largest and most diverse population of any state, with nearly 40 million residents. California’s population is 40% Latino, 35% White, 16% Asian American, 6.5% Black, 1.7% American Indian or Alaska Native, and 4% multiracial. 1 More than 10 million residents of California identify as immigrants, and about 7 million report speaking English less than very well. 1, 2 The population size and diversity of its residents warrants a robust and equally culturally and linguistically diverse physician workforce that is reflective of its residents. 3- 5
A report from the California Future Health Workforce Commission projected that by 2030, California will face a shortage of more than 4,100 primary care clinicians. 6 This shortage is felt among historically underresourced and marginalized communities. To adequately address this shortage, and ultimately achieve health equity, the state needs to implement new, and support existing, medical education programs to train a primary care workforce that aligns with the state’s population. 7- 9 Cultural and linguistic concordance between patients and physicians has been associated with improvements in quality of care, satisfaction with care, and greater access. 3, 5, 10-12
The University of California (UC) has been focused on addressing California’s physician workforce needs for nearly 2 decades. 13, 14 In 2007, the UC health sciences system concluded a comprehensive, multiyear planning effort, which included recommendations for medical education. 13 These recommendations called for an increase in medical student enrollment across the system to address the physician workforce shortage and to offer additional training opportunities for students committed to serving medically underserved communities throughout the state. 13, 14 The plan resulted in the expansion of Programs in Medical Education (PRIME).
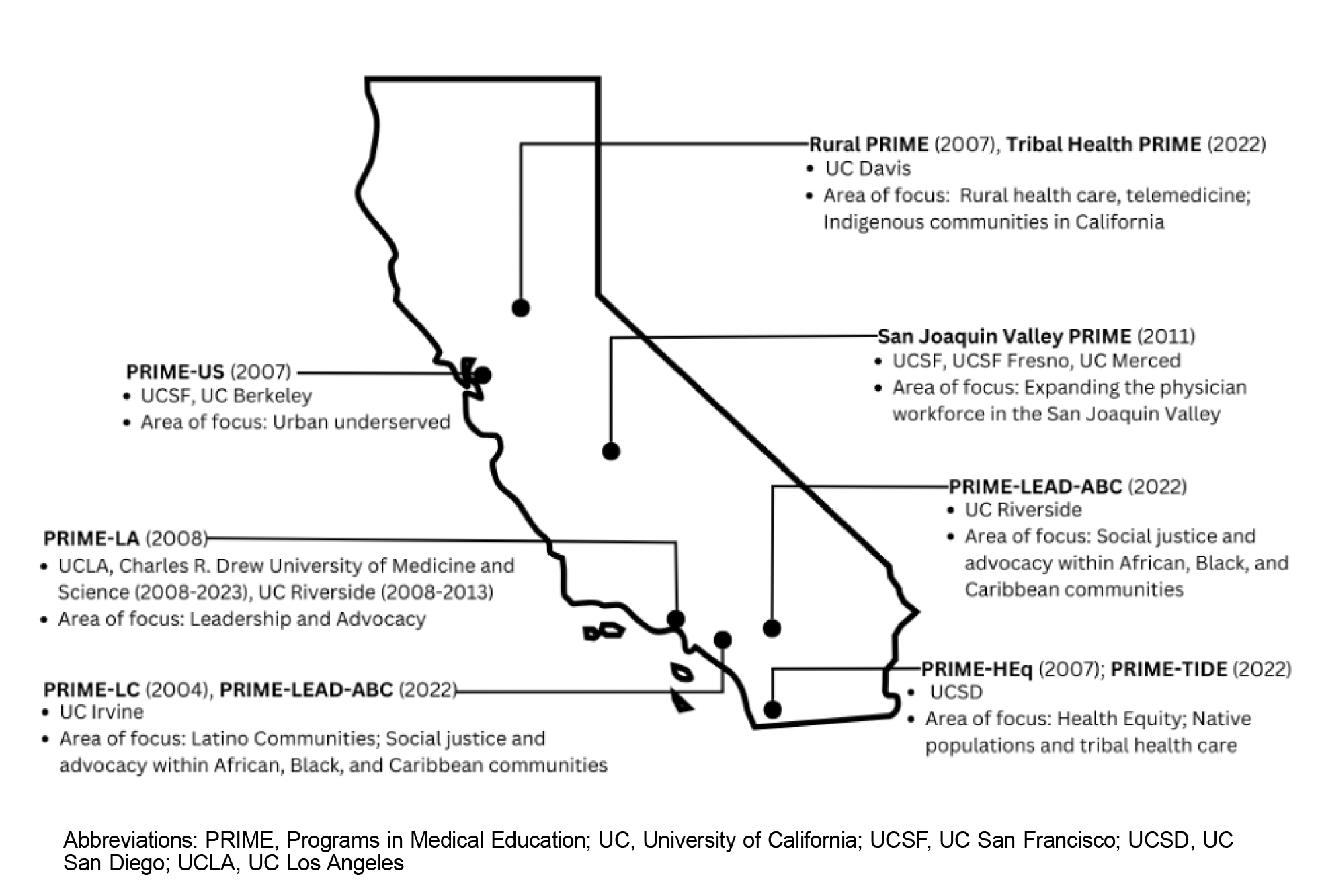
As shown in Figure 1, in 2004, UC Irvine developed the first program, PRIME-LC, which focused on Latino communities. 14, 15 Three years later, UC Davis launched Rural PRIME; UC San Francisco (UCSF) introduced PRIME-US, which focused on urban underserved communities; and UC San Diego (UCSD) established PRIME-HEq with a focus on health equity. 16-19 In 2008 UC Los Angeles (UCLA) started PRIME-LA with an emphasis on leadership and advocacy, and UCSF Fresno established San Joaquin Valley PRIME in 2011. More recently, UC Irvine and UC Riverside launched PRIME Leadership Education to Advance Diversity—African, Black, and Caribbean; and UC Davis and UCSD launched Tribal Health PRIME and PRIME Transforming Indigenous Doctor Education, respectively. All six UC medical schools have PRIME programs, each with a specific area of focus but an overlap in mission.
Across the UC system, PRIME programs have been successful in recruiting medical students from groups underrepresented in medicine (URM). 16-18 For example, a greater proportion of students from URM groups applied to UCSD’s PRIME program (PRIME-HEq) compared with students from non-URM backgrounds. 18 In an evaluation of the first 4 years of UCSF’s PRIME program (PRIME-US), 75% of students came from socioeconomically disadvantaged backgrounds, 44% identified as Latino, and 19% identified as African American. 16 While only 16 students entered PRIME-US during the period of evaluation, the majority of students matched into primary care specialties, including 38% in family medicine.
At the David Geffen School of Medicine at UCLA, PRIME-LA is one of two mission-based medical education programs. The second program is a partnership between UCLA and Charles R. Drew University of Medicine and Science (CDU); the UCLA-CDU program enrolled 24 students per year and included clinical rotations in South Los Angeles. The last cohort of the UCLA-CDU program was admitted in 2023, when CDU launched its new medical school.
Mission-based medical education programs have been successful in training those with intentions to practice in underserved communities. 7, 20, 21 Less is known about PRIME students’ intentions to practice in underserved areas or to care for underserved patients. The objective of this study was to examine intentions to practice in underserved communities for PRIME-LA graduates versus a comparator group. We hypothesized that participation in PRIME-LA is associated with increased intentions to practice in underserved areas or care for primarily underserved patient populations.
Program Description
PRIME-LA is a mission-based medical education program that trains future physician leaders and advocates who are engaged in health careers and in leadership in research and policy that address the needs of underserved and marginalized communities. Prospective students apply to UCLA through the Association of American Medical College’s centralized medical school application processing service, through which they can indicate interest in PRIME-LA. The mission of PRIME-LA is accomplished through a 5-year concurrent degree program leading to a Doctor of Medicine (MD) degree and a master’s in areas that complement the mission of the program. 13 Complementary areas might include a Master of Business Administration (MBA), Master of Public Health (MPH), Master of Public Policy (MPP), Master of Science (MS) in clinical research, Master of Legal Studies (MLS), or Master of Education (MEd). Most students obtain a master’s degree in public health, public policy, or business administration. The PRIME-LA program begins with a 3-week prematriculation curriculum, which consists of didactic learning focused on health equity for the underserved, community health, leadership and advocacy, mentorship, and advising. Students also participate in a year-long community-partnered cohort service project. Approximately 18 students are admitted annually; 291 students have matriculated to the PRIME-LA program, and 189 have graduated.
Participants
Our study sample included a total of 908 graduates of the David Geffen School of Medicine at UCLA between 2018 and 2023, who completed the graduation questionnaire administered annually by the Association of American Medical Colleges (AAMC).
Data Sources
We conducted a secondary analysis of data collected by AAMC for program evaluation purposes. Data was obtained from the AAMC graduation questionnaire, a national survey administered annually to all graduates of allopathic medical schools. The aggregate data was stratified by PRIME-LA participation (N=97). Our comparator group included all other graduates of the David Geffen School of Medicine at UCLA, including the MD/PhD, MD/DDS, and UCLA-CDU medical education programs. The study was institutional review board exempt.
Measures
The primary outcome measures were (a) intentions to practice in an underserved area, and (b) intentions to care for underserved patients. The questions examined were “Do you plan to work primarily in an underserved area?” and “Regardless of location, do you plan to care primarily for an underserved population?” Response options for both questions included yes, no, or undecided. Given our interest in identifying graduates expressing intentions to work in underserved areas and/or care for underserved patient populations, we collapsed the no and undecided response categories.
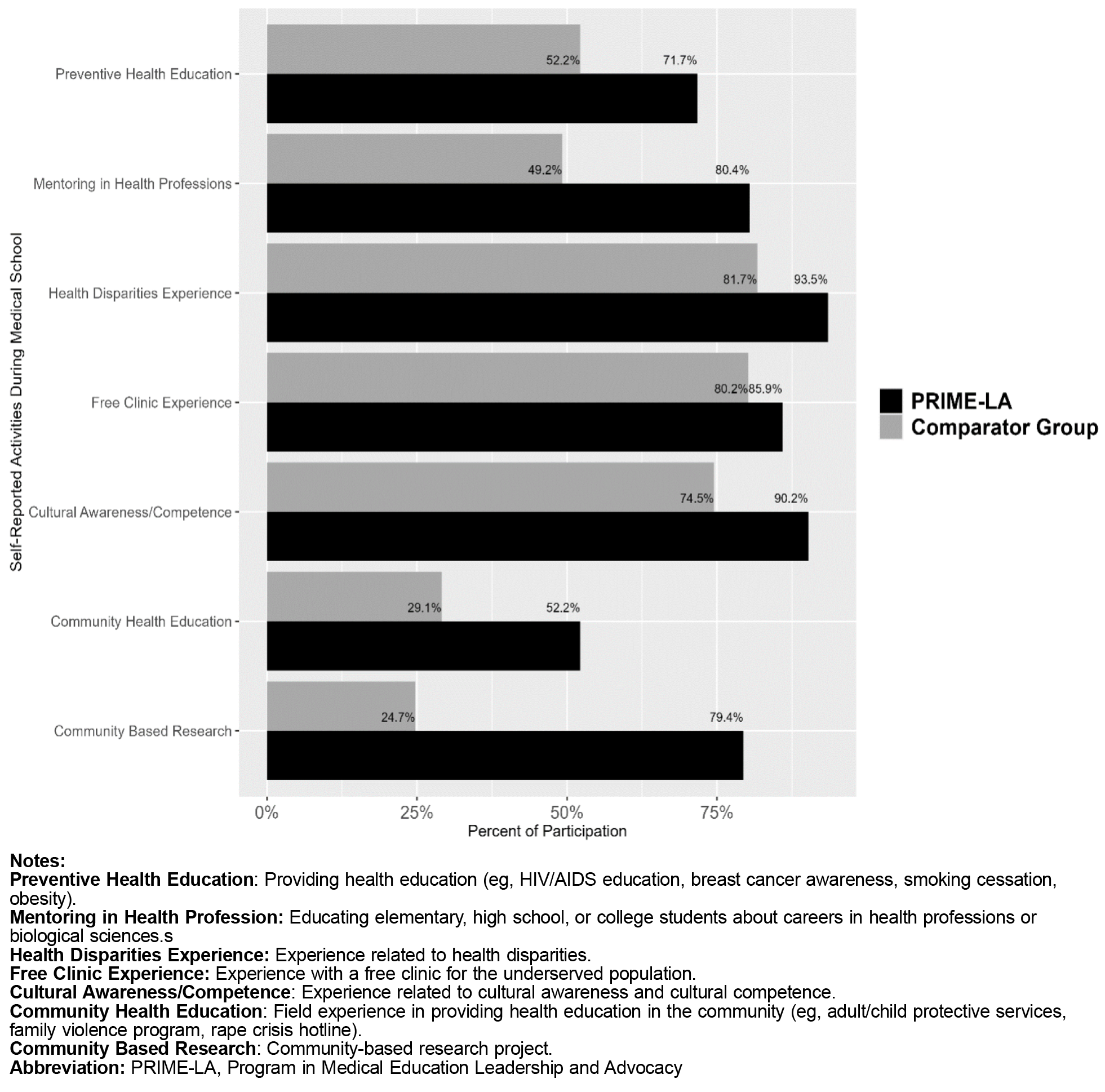
Secondary outcomes of interest included participation in selected activities during medical school (mentoring in health professions, public health education, health disparities experiences, community-based research, cultural awareness/competence experiences, and free clinic experiences) and intentions to specialize in family medicine. To measure participation in these activities, we used responses to the question “Indicate the activities you participated in during medical school on an elective (for credit) or volunteer (not required) basis.” This statement was followed by a list of 17 activities that graduates could select from. For our analysis, we defined “mentoring” as participation in “educating elementary, high school, or college students about careers in health professions or biological sciences.” Indicating participation in “providing health education (eg, HIV/AIDS education, breast cancer awareness, smoking cessation, obesity)” was defined as engaging in a public health–related activity. Involvement in a health disparities–related activity was defined as indicating participation in an “experience related to health disparities.” For our analysis, not selecting an activity was coded as a no response.
In our analysis, we defined URM status as graduates who self-identified their race/ethnicity as Black, Latino/a, Alaska Native, Native American, Native Hawaiian, or other Pacific Islander.
Statistical Analysis
All analyses for this study were conducted with Stata version 13.1 (StataCorp) statistical software. We computed frequencies across a 5-year period and performed ꭓ2 tests for all categorical variables. P values were calculated using ꭓ2 tests to compare two categorical variables. A P value of less than .05 determined statistically significant differences.
Characteristics of the UCLA graduates from 2018 through 2023 are shown in Table 1. A total of 908 graduates completed the demographics section of the graduation questionnaire. Of these, 97 were PRIME-LA graduates and 811 were in the comparator group. Sixty-three percent of PRIME-LA graduates and 51% of graduates from the comparator group identified as female (P=.041). Sixty-seven percent of PRIME-LA graduates identified as URM versus 29.2% of graduates in the comparator group (P<.001). A total of 91 PRIME-LA graduates and 778 graduates from the comparator group responded to the question regarding their intended area of practice. Fifty percent of PRIME-LA graduates reported intentions to specialize in a primary care specialty versus 38% of the comparator group (P=.040). Twenty-six percent of PRIME-LA graduates specifically expressed intentions to specialize in family medicine versus 6% of graduates in the comparator group (P<.001).
|
Medical student characteristics
|
PRIME-LA, N=97
%
|
Comparator group, N=811
%
|
P value
|
|
Gender
|
|
|
|
|
Male
|
37.1
|
48.6
|
.041
|
|
Female
|
62.9
|
51.4
|
|
|
Race/ethnicitya
|
|
|
|
|
American Indian or Alaska Native
|
3.7
|
0.1
|
<.001
|
|
Asian
|
19.4
|
40.4
|
<.001
|
|
Black
|
14.8
|
10.0
|
.135
|
|
Native Hawaiian or other Pacific Islander/other
|
0.9
|
6.5
|
.023
|
|
Latino/a
|
47.2
|
13.0
|
<.001
|
|
White
|
13.9
|
30.4
|
<.001
|
|
URMb
|
66.7
|
29.2
|
<.001
|
|
National Health Services Corps
|
12.5
|
2.7
|
.025
|
|
Specialty intentions at graduation
|
|
|
|
|
Family medicine
|
26.4
|
6.3
|
<.001
|
|
Pediatrics
|
8.8
|
7.3
|
.672
|
|
Internal medicine
|
14.3
|
24.2
|
.035
|
|
Obstetrics and gynecology
|
9.
|
5.3
|
.091
|
|
Psychiatry
|
9.
|
8.7
|
.697
|
|
Primary carec
|
49.5
|
37.8
|
.040
|
|
Nonprimary care specialtiesd
|
36.2
|
54.4
|
.001
|
Intentions to care for underserved populations are highlighted in Table 2. A total of 866 graduates responded to questions regarding their practice intentions. Ninety-one responses were from PRIME-LA graduates and 775 responses were from graduates of the comparator group. At the time of graduation, 89.0% of PRIME-LA graduates reported intentions to practice in underserved areas in contrast with 31.6% in the comparator group (P<.001). Similarly, 93.4% of PRIME-LA graduates expressed intentions to care for primarily underserved patients versus 43.5% of graduates from the comparator group (P<.001).
|
Intentions at graduation
|
PRIME-LA N=91 %
|
Comparator group, N=775 %
|
P value
|
|
Plan to work primarily in an underserved area
|
89.0
|
31.6
|
<.001
|
|
Regardless of location, plan to care primarily for an underserved population
|
93.4
|
43.5
|
<.001
|
Figure 2 summarizes selected elective or volunteer activities in which graduates reported participation. A total of 92 PRIME-LA graduates and 797 graduates from the comparator group responded. A greater proportion of PRIME-LA graduates indicated participating in mentoring activities during medical school (80.4% vs 4.2%, P<.001). In contrast with the comparator group, PRIME-LA graduates more frequently reported participation in health education (71.7% vs 52.2%, P<.001). About 86% of PRIME-LA graduates and 80% of graduates from the comparator group participated in an experience with a free clinic for underserved populations (P=.211). A larger proportion of PRIME-LA graduates reported participating in activities related to health disparities than graduates from the comparator group (93.5% vs 81.7%, P=.003) and in community-based research projects (79.4% vs 24.7%, P<.001).
In this study, we found that UCLA PRIME-LA program graduates, over a 5-year period, were more likely to report intentions to practice in underserved areas than the comparator group. Additionally, program graduates were more likely to report intentions to provide care to underserved patient populations regardless of location than the comparator group. Our results suggest that a mission-based medical education program may be an effective method to graduate diverse medical students who intend to address the health and health care needs of underserved communities.
Our study found that graduates of this mission-based program were more likely to choose family medicine as a specialty and primary care. This finding has medical education and workforce policy implications because family physicians are increasingly providing care in diverse languages, which is integral to addressing pressing national health issues. Furthermore, family physicians from diverse backgrounds are more likely to care for underserved populations and to work in solo practices. 22-26 Although limited in sample size, studies of UCSF’s PRIME-US and Rural-PRIME at UC Davis also found that family medicine was the most common specialty for graduates. 16, 17 We posit that family medicine was the most common specialty among PRIME-LA graduates because the program’s curricula (ie, concurrent master’s degree and community-based experiences) and mission focus on training physician leaders and advocates who are sensitive to community and social issues that impact clinical care among diverse disadvantaged communities. The program attracts mission-aligned applicants. 18
Our findings that program graduates intend to practice and care for underserved patients are consistent with similar studies that evaluated other mission-based medical education programs. 20, 21 Studies of the UCLA-CDU program have shown that graduates had greater adjusted odds of reporting intention to work in underserved communities at graduation, greater odds of maintaining these intentions between matriculation and graduation, and higher adjusted odds of practicing in underserved areas compared with those in the traditional UCLA curriculum. 18, 19 A study of alumni of the Urban Underserved Program (UUP) at Jefferson Medical College found that the vast majority of respondents were practicing in urban areas and underserved or physician shortage areas, and more than half were practicing primary care. 27
The high level of affirmative intentions to practice in underserved areas is important to highlight given that our UCLA comparator group included students from the UCLA-CDU Medical Education Program, which has been shown to be associated with increased intentions to practice in underserved areas at the time of graduation. 18 We also found our program participants, during medical school, were more likely to participate in activities (eg, mentoring, public health, community-based learning, and health disparities) that are aligned with the improvement of underserved communities. Our measure of participation in activities was captured at the end of medical school; these results are similar to a previous study that examined activities during medical school. 14 Our results expand the peer-reviewed literature on the UC system PRIME programs by focusing on practice intentions outcomes at graduation. Previous literature focused on curricula, the diverse applicant pool, or a description of the mission. 13-19
Our study had some limitations. The analysis was cross-sectional, and whether intentions correlate with actual practice location or providing care for underserved patients and communities is unclear. We cannot infer causal effects of the program on intentions. Selection bias could explain the observed results. For example, PRIME-LA students may already have been more inclined to practice in underserved areas or care for underserved populations at the time of matriculation. We did not measure objective practice location, nor did we verify student participation in the selected medical school activities. Self-reports are subject to recall bias and socially desirable answers. The findings cannot be generalized to other mission-based programs.
Our results have medical education policy implications. Medical schools that aim to improve the number of medical school graduates who have intentions to practice in underserved areas should consider establishing or expanding mission-based medical education programs. Mission-based programs that use holistic admissions rubrics provide an effective mechanism for meeting the physician workforce needs of individual states or the United States. In 2022, California invested to expand the PRIME programs for key communities that remained significantly underresourced. Future research will focus on actual and objective practice outcomes in underserved geographical areas or caring for underserved populations as opposed to self-reported intentions at graduation.
We conclude that UCLA PRIME-LA program graduates, over a 5-year period, were more likely to report intentions to practice in underserved areas than the comparator group. Program graduates also were more likely to report intentions to provide care to underserved patient populations, regardless of location, than the comparator group. Our results support the effectiveness of mission-based medical education programs designed to graduate physicians who intend to practice and/or provide clinical care for underserved communities.
Presentations
This research was presented at the Society of Teachers of Family Medicine Annual Spring Conference in Los Angeles, California, on May 6, 2024.
References
-
-
-
Moreno G, Morales LS.
Hablamos juntos (Together we speak): interpreters, provider communication, and satisfaction with care.
J Gen Intern Med. 2010;25(12):1,282-1,288.
doi:10.1007/s11606-010-1467-x
-
Moreno G, Tarn DM, Morales LS. Impact of interpreters on the receipt of new prescription medication information among Spanish-speaking Latinos.
Med Care. 2009;47(12):1,201-1,208.
doi:10.1097/MLR.0b013e3181adcc1b
-
Detz A, Mangione CM, Nunez de Jaimes F, et al. Language concordance, interpersonal care, and diabetes self-care in rural Latino patients.
J Gen Intern Med. 2014;29(12):1,650-1,656.
doi:10.1007/s11606-014-3006-7
-
California Future Health Workforce Commission. Meeting the Demand for Health: Final Report of the California Future Health Workforce Commission. The Commision; February 2019.
-
Goodfellow A, Ulloa JG, Dowling PT, et al. Predictors of primary care physician practice location in underserved urban or rural areas in the United States: a systematic literature review.
Acad Med. 2016;91(9):1,313-1,321.
doi:10.1097/ACM.0000000000001203
-
Talamantes E, Hernandez AM, Gonzalez R, et al. Interest in family medicine among US medical students and its association with a community college academic pathway. Fam Med. 2017;49(10):759-764.
-
Talamantes E, Mangione CM, Gonzalez K, Jimenez A, Gonzalez F, Moreno G. Community college pathways: improving the U.S. physician workforce pipeline.
Acad Med. 2014;89(12):1,649-1,656.
doi:10.1097/ACM.0000000000000438
-
Talamantes E, Norris KC, Mangione CM, et al. Linguistic isolation and access to the active kidney transplant waiting list in the United States.
Clin J Am Soc Nephrol. 2017;12(3):483-492.
doi:10.2215/CJN.07150716
-
Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A systematic review of the impact of patient-physician non-English language concordance on quality of care and outcomes.
J Gen Intern Med. 2019;34(8):1,591-1,606.
doi:10.1007/s11606-019-04847-5
-
Hsueh L, Hirsh AT, Maupomé G, Stewart JC. Patient-provider language concordance and health outcomes: a systematic review, evidence map, and research agenda.
Med Care Res Rev. 2021;78(1):3-23.
doi:10.1177/1077558719860708
-
Nation CL, Gerstenberger A, Bullard D. Preparing for change: the plan, the promise, and the parachute.
Acad Med. 2007;82(12):1,139-1,144.
doi:10.1097/ACM.0b013e318159cd6e
-
Manetta A, Stephens F, Rea J, Vega C. Addressing health care needs of the Latino community: one medical school’s approach.
Acad Med. 2007;82(12):1,145-1,151.
doi:10.1097/ACM.0b013e318159cccf
-
-
Sokal-Gutierrez K, Ivey SL, Garcia RM, Azzam A. Evaluation of the Program in Medical Education for the Urban Underserved (PRIME-US) at the UC Berkeley–UCSF Joint Medical Program (JMP): the first 4 years.
Teach Learn Med. 2015;27(2):189-196.
doi:10.1080/10401334.2015.1011650
-
Eidson-Ton WS, Rainwater J, Hilty D, et al. Training medical students for rural, underserved areas: a rural medical education program in California.
J Health Care Poor Underserved. 2016;27(4):1,674-1,688.
doi:10.1353/hpu.2016.0155
-
Bailey JA, Willies-Jacobo LJ. Are disadvantaged and underrepresented minority applicants more likely to apply to the program in medical education-health equity?
Acad Med. 2012;87(11):1,535-1,539.
doi:10.1097/ACM.0b013e31826d6220
-
Powell T, Garcia KA, Lopez A, Bailey J, Willies-Jacobo L. University of California San Diego’s Program in Medical Education-Health Equity (PRIME-HEq): training future physicians to care for underserved communities.
J Health Care Poor Underserved. 2016;27(3):937-946.
doi:10.1353/hpu.2016.0109
-
Ko M, Edelstein RA, Heslin KC, et al. Impact of the University of California, Los Angeles/Charles R. Drew University Medical Education Program on medical students’ intentions to practice in underserved areas.
Acad Med. 2005;80(9):803-808.
doi:10.1097/00001888-200509000-00004
-
Ko M, Heslin KC, Edelstein RA, Grumbach K. The role of medical education in reducing health care disparities: the first ten years of the UCLA/Drew Medical Education Program.
J Gen Intern Med. 2007;22(5):625-631.
doi:10.1007/s11606-007-0154-z
-
Tong ST, Jetty A, Liaw WR, Bazemore AW, Jabbarpour Y. Racial/ethnic minority identifying family physicians are more likely to work in solo practices.
J Am Board Fam Med. 2023;36(2):380-381.
doi:10.3122/jabfm.2022.220332R1
-
Eden AR, Bazemore A, Morgan ZJ, Jabbarpour Y. Family physicians increasingly deliver care in diverse languages.
J Am Board Fam Med. 2022;35(1):5-6.
doi:10.3122/jabfm.2022.01.210190
-
Abraham R, Wilkinson E, Jabbarpour Y, Bazemore A. Family physicians play key role in bridging the gap in access to opioid use disorder treatment. Am Fam Physician. 2020;102(1):10-10.
-
Jetty A, Hyppolite J, Eden AR, Taylor MK, Jabbarpour Y. Underrepresented minority family physicians more likely to care for volunerable populations.
J Am Board Fam Med. 2022;35(2):223-224.
doi:10.3122/jabfm.2022.02.210280
-
Flores-Rodarte J, Topmiller M, Jabbarpour Y. Distribution of Spanish-speaking family physicians, 2013-2019. Am Fam Physician. 2022;105(6):654-655.
-
Roy V, Hurley K, Plumb E, Castellan C, McManus P. Urban underserved program: an analysis of factors affecting practice outcomes. Fam Med. 2015;47(5):373-377.



There are no comments for this article.