Background and Objectives: The 2023 Accreditation Council for Graduate Medical Education (ACGME) program requirements for family medicine residencies state that family physicians must have the competence to address racial and ethnic health disparities experienced by their patients. Racial justice curricula (RJC) or antiracism curricula can provide residencies with the tools faculty and residents need. This study explores the differences in perceived barriers between family medicine program directors (PDs) and residents.
Methods: Survey questions on RJCs were included in the 2020 Council of Academic Family Medicine Educational Research (CERA) survey of PDs and 2021 CERA survey of residents. Participants’ perceived top two barriers to implementing an RJC in their residency program were illustrated with Sankey diagrams. We used the χ2 test and logistic regression for analysis.
Results: Of the 578 participants included, 312 (54%) were PDs and 266 (46%) were residents. Compared to PDs, residents were more likely to identify as female, less likely White, and more likely from community-based, nonuniversity-affiliated residency programs. PDs ranked lack of faculty training as the most important barrier, while residents ranked lack of time as the top barrier. Residents also were significantly more likely to rank lack of faculty interest and resident interest as barriers.
Conclusions: Family medicine PDs and residents identified different barriers to implementing an RJC. Additional research is needed to investigate the impact of knowledge and culture on residency programs’ receptiveness to addressing racial and ethnic health disparities.
On July 1, 2023, the Accreditation Council for Graduate Medical Education (ACGME) introduced updated program requirements for family medicine residencies, emphasizing the importance of addressing racial and ethnic health disparities. 1 Among these updates, ACGME outlined that family physicians must possess “the competence necessary to address racial and ethnic health disparities experienced by their patients. Family physicians should understand that race is a social construct, that racism is a fundamental cause of health inequities, health disparities and disease.” While these updates mark a significant acknowledgment, the call to address systemic racism and its impact on health disparities is not new. 2-5 Over the years, multiple family medicine organizations have recognized racism’s detrimental impact on health and the health care system, issuing calls for action urging residency programs to intentionally design and implement curricular changes to address racism. 6-12
Historical perspectives support this call for action. In 2003, the Institute of Medicine highlighted that racial and ethnic health care disparities often were linked to physician bias, whether conscious or unconscious. 13 Implicit biases, reflecting subconscious attitudes, have since been demonstrated to contribute to inequities in outcomes for historically marginalized groups, including racial and ethnic minorities as well as gender and sexual minorities. 14-17 In response, training programs have increasingly sough to mitigate the negative effects of physician biases through racial justice curricula (RJC). Such curricula focuses on (a) understanding the cause and consequences of racism and its effects on health disparities and (b) creating a safe environment to allow individuals to develop the tools needed to address racism. 5, 18-20 For this study, antiracism curricula and RJC are used interchangeably; both share the goal of addressing systemic racism in medical education. Despite these national calls for change, the implementation of RJCs in family medicine residency programs has been inconsistent and slow.
Recent studies have highlighted this gap. A 2020 survey of family medicine residency program directors (PDs) found that while 88.7% of PDs (n=283) believed that understanding structural racism is important, only 30.7% reported having a formal RJC in their programs. 21 Similarly, in 2021, a survey of family medicine residents revealed that although 91.5% (n=266) of respondents believed that addressing racism is an educational priority, only 17.3% reported the existence of a longitudinal curriculum in their program. 22 These studies reflect a shared recognition of the importance of RJCs but also underscore barriers to their implementation. These barriers range from structural challenges such as limited time and resources to cultural ones such as varying levels of interest among residents and faculty. Both surveys identified lack of faculty training as a major barrier to implementing RJCs. Faculty, though often interested in developing skills to facilitate conversations about race and racism, frequently lack the same level of awareness as residents regarding topics such as the history of racism in medicine, structural competency, and health inequities. 11, 12, 23 This disconnect highlights a challenge for implementing RJCs.
The purpose of this study was to investigate and compare the barriers to implementing RJCs as perceived by PDs and residents. We hypothesized that PDs are more likely to rank structural barriers, such as insufficient faculty training and curricular resources, while residents are more likely to rank cultural barriers, such as perceived lack of faculty interest. We propose that these differences stem from variations in knowledge and training. 24 While PDs may lack specific knowledge on how to implement RJCs, residents, having received some antiracism training in medical school, may feel better equipped to engage with these concepts but perceive gaps in faculty interest. 22, 25
Survey
The survey questions were part of two larger omnibus surveys conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA). This study was an analysis of data obtained as part of the 2020 CERA PD survey and the 2021 CERA family medicine resident survey. The methodology of the CERA surveys has previously been described. 26
The 2020 CERA PD survey is distributed annually to all ACGME-accredited US family medicine residency PDs, as identified by the Association of Family Medicine Residency Directors. The final sampling pool included 624 PDs, and the response rate was 50% (312/624).
For the 2021 CERA family medicine resident survey, a sample of 5,000 resident members of the American Academy of Family Physicians received an email invitation to participate in the survey. Respondents were entered into a drawing for one of five $100 gift cards as an incentive for survey completion. The overall response rate for the survey was 5.3% (266/5,000).
Due to the 5.3% response rate, the authors entered into a data-sharing agreement with the American Board of Family Medicine (ABFM) to compare the survey sample demographic characteristics with a national sample of family medicine residents (N=14,170 as of October 20, 2023). Using χ2 testing or the Fisher exact test, gender (female/male/unknown or other), ethnicity (Hispanic/Latino or not), race, and program region were found to be similar (Supplementary Table A). CERA respondents had a higher percentage of smaller programs (<19 residents, 44.7% vs 29.1%) and a smaller percentage of larger programs (>31 residents, 12.4% vs 23.1%).
Each survey study was approved by the American Academy of Family Physicians Institutional Review Board. University of Utah Institutional Review Board deemed this study as nonhuman subjects research.
Measures
We analyzed PD and resident respondent demographic characteristics (ie, gender, ethnicity, race) and responses to “What are the two most important barriers to implementing an RJC in your residency program?” Answers to the most important barriers were as follows: lack of faculty training in this topic area, lack of time in the overall curriculum, lack of interest in a formal RJC among faculty, lack of interest in a formal RJC among residents, lack of curriculum resources for the development of a formal RJC, and lack of financial resources for the development of a formal RJC. For the analysis, these barriers have been simplified in order of listing to faculty training, time, faculty interest, resident interest, curriculum resources, and financial resources. Participants’ first and second choice of important barriers were visualized with Sankey diagrams. Other measures included program type (university-based, community-based university-affiliated, community-based nonaffiliated, other), state region (New England, Middle Atlantic, South Atlantic, East South Central, East North Central, West South Central, West North Central, Mountain, Pacific), international medical graduates in the program, size of the residency, and community size (<30,000, 30,000–74,999, 75,000–149,999, 150,000–499,999, 500,000–1 million, >1 million).
Analyses
All statistical tests were conducted to assess the associations of demographic and barriers between PDs and residents. We used the χ2 test and logistic regression to conduct comparisons. The outcome for the logistic regression model was the respondents’ identification of their first or second most important barrier to implementing an RJC. The adjusted logistic regression analyses included predictors for program type, gender, ethnicity, race, state region, and community size. A comparison of 2021 ABFM demographics with the 2021 CERA demographics also was performed. Missing values were removed using listwise deletion. All final analyses were conducted in RStudio (R Foundation). All statistical tests were two-sided, with significance level set to .05.
The final analysis included 578 participants, comprising 54% PDs (n=312) and 46% residents (n=266; Table 1 ). The two groups differed significantly in terms of gender, race, and residency program type. Compared to PDs, residents were more likely to identify as female (41% vs 56%, P=.005), less likely to identify as White (79% vs 56%, P<.001), and more likely to come from community-based, nonuniversity-affiliated residency programs (21% vs 36%, P<.001).
|
|
Total population, n (%)
|
Program director, n (%)
|
Resident, n (%)
|
P value*
|
|
Included in analysis
|
578 (100)
|
312 (54)
|
266 (46)
|
|
|
Program
|
<.001
|
|
University-based
|
97 (17)
|
49 (16)
|
48 (18)
|
|
|
Community-based, university-affiliated
|
293 (51)
|
174 (56)
|
119 (45)
|
|
|
Community-based, nonaffiliated
|
159 (28)
|
64 (21)
|
95 (36)
|
|
|
Military
|
0
|
0
|
4 (2)
|
|
|
Other
|
9 (2)
|
5 (2)
|
0
|
|
|
Unknown/N/A
|
20 (3)
|
20 (6)
|
0
|
|
|
State region
|
.566
|
|
New England (NH, MA, ME, VT, RI, or CT)
|
23 (4)
|
11 (4)
|
12 (5)
|
|
|
Middle Atlantic (NY, PA, or NJ)
|
93 (16)
|
51 (16)
|
42 (16)
|
|
|
South Atlantic (PR, FL, GA, SC, NC, VA, DC, WV, DE, or MD)
|
90 (16)
|
51 (16)
|
39 (15)
|
|
|
East South Central (KY, TN, MS, or AL)
|
34 (6)
|
17 (5)
|
17 (6)
|
|
|
East North Central (WI, MI, OH, IN, or IL)
|
100 (17)
|
55 (18)
|
45 (17)
|
|
|
West South Central (OK, AR, LA, or TX)
|
53 (9)
|
27 (9)
|
26 (10)
|
|
|
West North Central (ND, MN, SD, IA, NE, KS, or MO)
|
53 (9)
|
28 (9)
|
25 (9)
|
|
|
Mountain (MT, ID, WY, NV, UT, AZ, CO, or NM)
|
46 (8)
|
32 (10)
|
14 (5)
|
|
|
Pacific (WA, OR, CA, AK, or HI)
|
83 (14)
|
40 (13)
|
43 (16)
|
|
|
Unknown/NA
|
3 (1)
|
0
|
3 (1)
|
|
|
Size of the community
|
.527
|
|
Less than 30,000
|
61 (11)
|
33 (11)
|
28 (11)
|
|
|
30,000 to 74,999
|
102 (18)
|
53 (17)
|
49 (18)
|
|
|
75,000 to 149,999
|
123 (21)
|
56 (18)
|
67 (25)
|
|
|
150,000 to 499,999
|
128 (22)
|
70 (22)
|
58 (22)
|
|
|
500,000 to 1 million
|
68 (12)
|
38 (12)
|
30 (11)
|
|
|
More than 1 million
|
75 (13)
|
44 (14)
|
31 (12)
|
|
|
Unknown/N/A
|
21 (4)
|
18 (6)
|
3 (1)
|
|
|
Number of residents in program
|
.288
|
|
Less than 19
|
233 (40)
|
114 (37)
|
119 (45)
|
|
|
19–31
|
247 (43)
|
135 (43)
|
112 (42)
|
|
|
More than 31
|
78 (13)
|
45 (14)
|
33 (12)
|
|
|
Unknown/N/A
|
20 (3)
|
18 (6)
|
2 (1)
|
|
|
International medical graduates
|
.509
|
|
0%–24%
|
334 (58)
|
184 (59)
|
150 (56)
|
|
|
25%–49%
|
89 (15)
|
46 (15)
|
43 (16)
|
|
|
50%–74%
|
76 (13)
|
36 (12)
|
40 (15)
|
|
|
75%–100%
|
55 (10)
|
26 (8)
|
29 (11)
|
|
|
Unknown/N/A
|
24 (4)
|
18 (6)
|
4 (2)
|
|
|
|
Total population, n (%)
|
Program director, n (%)
|
Resident, n (%)
|
P value*
|
|
Gender
|
.005
|
|
Female
|
275 (48)
|
127 (41)
|
148 (56)
|
|
|
Male
|
275 (48)
|
161 (52)
|
114 (43)
|
|
|
Unknown/other
|
28 (5)
|
24 (8)
|
4 (2)
|
|
|
Ethnicity
|
.413
|
|
Non-Hispanic/Latino
|
510 (88)
|
271 (87)
|
239 (90)
|
|
|
Hispanic/Latino
|
46 (8)
|
21 (7)
|
25 (9)
|
|
|
Unknown
|
22 (4)
|
20 (6)
|
2 (1)
|
|
|
Race
|
<.001
|
|
American Indian or Alaska Native
|
5 (1)
|
5 (2)
|
0
|
|
|
Asian
|
86 (15)
|
24 (8)
|
62 (23)
|
|
|
Black or African American
|
36 (6)
|
14 (4)
|
22 (8)
|
|
|
Native Hawaiian or Pacific Islander
|
2 (<1)
|
1 (<1)
|
1 (<1)
|
|
|
White
|
395 (68)
|
245 (79)
|
150 (56)
|
|
|
Unknown/other**
|
54 (9)
|
23 (7)
|
31 (12)
|
|
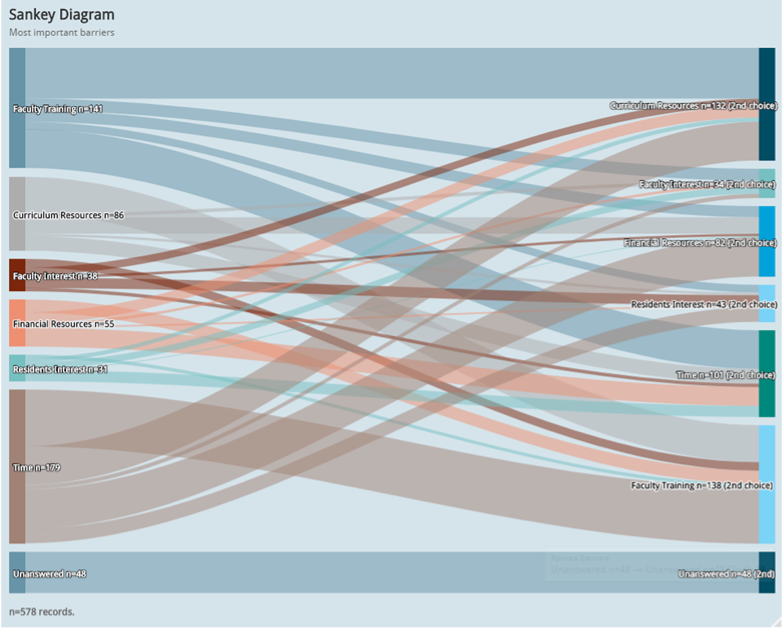
Figure 1 illustrates the pooled responses of PDs and residents on the top two barriers to implementing an RJC in their residency programs. Both groups ranked time (31%, n=179), faculty training (25%, n=141), and curriculum resources (15%, n=86) as the most important barriers, in that order. For the second most important barrier, faculty training (24%, n=138) was followed by curriculum resources (23%, n=132) and time (17%, n=101). In the Sankey diagram, the bands connecting the two top ranked barriers are widest, thus strongest, between time and faculty training, as well as between faculty training and curriculum resources.
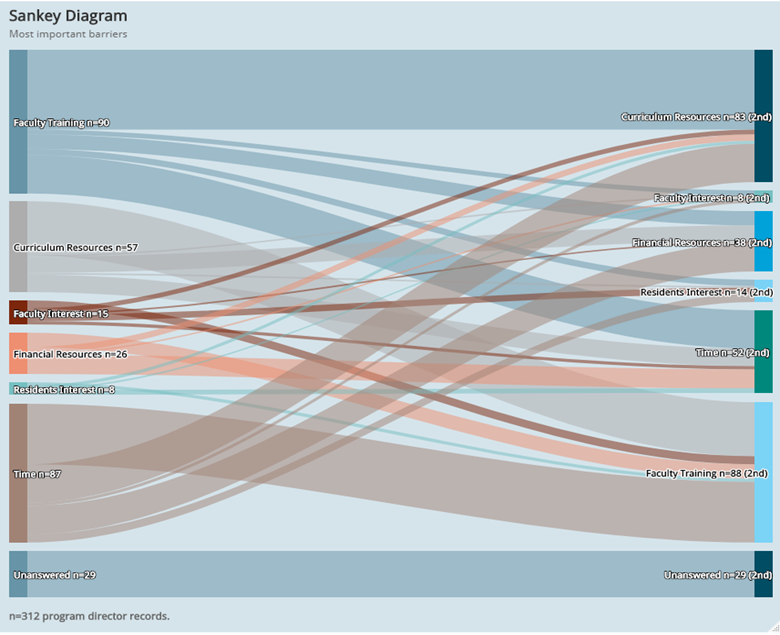
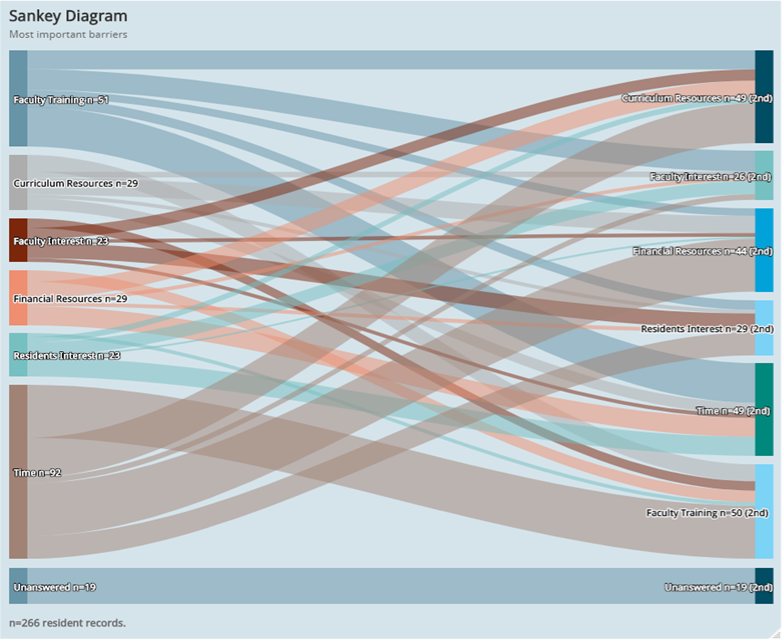
Figure 2 and Figure 3 provide detailed visual rankings for PDs and residents, respectively. Among PD’s, faculty training (29%, n=90) was the most important barrier, followed by time (28%, n=87) and curriculum resources (18%, n=57). For their second most important barrier, PDs ranked faculty training (28%, n=88), curriculum resources (27%, n=83), then time (17%, n=52). The strongest connections between the top two barriers were between faculty training and curriculum resources, as well as between time and faculty training. Residents, on the other hand, ranked time (35%, n=92) as the most important barrier, followed by faculty training (19%, n=51), and a tie between curriculum resources (11%, n=29) and financial resources (11%, n=29). For the second most important barrier, residents ranked faculty training (19%, n=50), followed by a tie between time (18%, n=49) and curriculum resources (18%, n=49), and then financial resources (17%, n=44). The strongest connections between the two top barriers were between time and faculty training, as well as between time and financial resources.
Table 3 represents the specific counts for each ranked barrier by total participants (both PDs and residents) and subgroups. Statistical analysis revealed significant differences between PDs’ and residents’ ranked barriers. For example, PDs were more likely to cite “lack of faculty training in this topic area” (30% vs19%; P<.001), while residents were more likely to cite “lack of interest in a formal RJC among faculty” (4% vs 9%; P<.001) and “lack of interest in a formal RJC among residents” (4% vs 10%; P<.001).
|
|
Population (N=578)
|
Program director (N=312)
|
Resident (N=266)
|
P value**
|
Adjusted P value***
|
|
|
First or second most important
|
Most important, n (vert %)
|
Second most important, n (vert %)
|
First or second most important
|
Most important, n (vert %)
|
Second most important, n (vert %)
|
First or second most important, n (%)
|
Most important, n (vert %)
|
Second most important, n (vert %)
|
|
|
|
Lack of . . .*
|
|
|
|
|
|
|
|
|
|
|
|
|
Time
|
280 (25)
|
179 (31)
|
101 (17)
|
139 (23)
|
87 (28)
|
52 (17)
|
141 (27)
|
92 (35)
|
49 (18)
|
.257
|
.169
|
|
Faculty training
|
279 (25)
|
141 (24)
|
138 (24)
|
178 (30)
|
90 (29)
|
88 (28)
|
101 (19)
|
51 (19)
|
50 (19)
|
<.001
|
<.001
|
|
Curriculum resources
|
218 (19)
|
86 (15)
|
132 (23)
|
140 (24)
|
57 (18)
|
83 (27)
|
78 (15)
|
29 (11)
|
49 (18)
|
<.001
|
<.001
|
|
Financial resources
|
137 (12)
|
55 (10)
|
82 (14)
|
64 (11)
|
26 (8)
|
38 (12)
|
73 (14)
|
29 (11)
|
44 (17)
|
.156
|
.160
|
|
Residents interest
|
74 (7)
|
31 (5)
|
43 (7)
|
22 (4)
|
8 (3)
|
14 (5)
|
52 (10)
|
23 (9)
|
29 (11)
|
<.001
|
<.001
|
|
Faculty interest
|
72 (6)
|
38 (7)
|
34 (6)
|
23 (4)
|
15 (5)
|
8 (3)
|
49 (9)
|
23 (9)
|
26 (10)
|
<.001
|
<.001
|
|
Unanswered
|
66 (6)
|
48 (8)
|
48 (8)
|
28 (5)
|
29 (9)
|
29 (9)
|
38 (7)
|
19 (7)
|
19 (7)
|
.108
|
.121
|
Both family medicine PDs and residents ranked structural barriers such as “lack of time in the overall curriculum,” “lack of faculty training in this topic area,” and “lack of curriculum resources for the development of a formal RJC” as the top challenges to implementing an RJC in their respective residency program. However, the prioritization of these barriers varied. Among PDs, lack of faculty training emerged as the most prevalent barrier, followed by lack of curricular resources and lack of time, respectively. In contrast, residents ranked lack of time as the most important barrier, followed by lack of faculty training and lack of curriculum resources. Notably, residents were significantly more likely to rank cultural barriers such as “lack of interest in a formal RJC among residents” and “lack of interest in a formal RJC among faculty,” although these did not rank among their top three barriers.
The difference in how PDs and residents ranked barriers likely reflected disparities in knowledge bases. PDs ranked faculty training as both the first and second most important barrier, signaling their awareness of a critical gap in medical education. This finding aligns with prior research suggesting that many faculty members lack adequate preparation to teach topics such as structural racism, health equity, and how to be antiracist. For instance, Fatahi et al reported that only 9 out of 29 undergraduate and graduate medical education program leaders felt that their faculty were adequate to educate learners on antiracism topics, and the majority acknowledged that faculty needed additional training, guidance, and/or support. 27 This barrier to faculty training can be addressed. One family medicine residency program demonstrated the feasibility of implementing a longitudinal training for faculty by embedding the series into existing meeting times. 28 Many of the topics covered do not require dedicated faculty to develop them. Major organizations, including the American Medical Association and the Association of American Medical Colleges, have developed training modules and curricular resources tailored to faculty with limited prior exposure to these topics. 25, 29-35 The Society of Teachers of Family Medicine also has developed a resource website and tool kit to guide conversations on race and racism, including a train-the-trainer workshop. 5, 31, 36 A potential research question to investigate is whether the demographics of PDs influence how they ranked barriers to implementing an RJC. In this pooled study, compared to the residents, PDs were more likely White and male. In the 2020 CERA PD survey, female PDs were more likely than male PDs to agree/strongly agree that formal RJCs should be included in residency training. 21. Yet gender and race were not explored as predictors to barriers. Additional analysis on how such demographics influence perceived barriers requires further study.
In contrast, residents prioritized lack of time in the overall curriculum as the most important barrier. While many published studies have focused on a one-time session or stand-alone workshop, the discussions repeatedly emphasized the need for ongoing trainings to ensure durable change. 19, 32, 34, 35, 37, 38 RJCs cover multiple complex topics that cannot be addressed in a single session, such as understanding structural racism and its impact on health and health care disparities, reflecting and addressing implicit biases, advocating for change, and more. Thus, RJCs need to be longitudinal and integrated throughout the residency curriculum. Successful implementation requires leadership engagement and support. For instance, a community-based residency program that successfully implemented a mandatory antiracism curriculum linked its effectiveness to strong leadership support and dedicated didactic time—highlighting the critical role of institutional prioritization. 11, 18, 25, 28, 29, 39, 40 Another successful longitudinal faculty training required a dedicated faculty work group, reiterating the importance of buy-in. 28 In a 2023 CERA survey of family medicine department chairs, 61.5% strongly agreed that advancing diversity, equity, inclusion, and antiracism (DEIA) was important, yet only 22.0% strongly agreed that they felt confident in advancing DEIA work. 41 Furthermore, appropriate financial and administrative support was still lacking, factors that need to be accounted for when exploring ways to increase time for an RJC.
A notable finding was that residents were significantly more likely than PDs to identify cultural barriers, such as “lack of interest in a formal RJC among residents” and “lack of interest in a formal RJC among faculty.” This difference may stem from residents’ attitudes and existing knowledge. A growing number of undergraduate medical education programs are incorporating aspects of RJC such as teaching concepts of equity, antiracism, and cultural competency versus humility, implicit bias, and microaggressions. 25, 27, 42, 43 Thus, a higher number of incoming residents understand these foundational concepts and are either ready to tackle the issues of racial justice in practice or do not prioritize the need to relearn these concepts. 25 A lack of interest from both residents and faculty also may arise from feelings of discomfort. Conversations about race often require essential but challenging reflections on the impact of structural and interpersonal racism in driving disparities between White communities and communities of color. Such discussions may evoke heightened sensitivity, particularly among individuals who identify as White, where feelings of guilt about past and present injustices can lead to reactions such as anger, frustration, or withdrawal—responses that hinder constructive dialogue. 11, 44, 45 Further research should evaluate whether such cultural barriers truly exist in residency programs and identify best practices to address them.
This study had several limitations. First, the differences in demographics and program types between PDs and residents reduce the generalizability of the findings. For instance, PDs were more likely to represent community-based, university-affiliated programs, while residents were more likely to represent community-based, nonaffiliated with university programs. These differences may have influenced the prioritization of barriers and limit the comparability of their responses. Second, the ranking methodology constrained participants to select their top two barriers from a predefined list, potentially oversimplifying their preferences or excluding other important considerations. Future studies might employ rating scales to capture more nuanced perspectives.
Finally, these findings must be interpreted within the broader sociopolitical context. The CERA studies were conducted in 2020 and 2021, a critical period marked by a surge in research and advocacy shedding light on the health care disparities stemming from systemic racism. 46, 47 During that time, medical students and residents vocally urged institutions to enact reforms aimed at addressing structural racism. 3, 4, 7 Since then, several states have enacted legislative changes prohibiting initiatives aimed at fostering equity, diversity, and inclusion. Despite these challenges, the updated ACGME requirements to address racial and ethnic health disparities present an opportunity for programs to prioritize RJCs. Future research should evaluate how family medicine residency programs navigate these evolving dynamics and assess the long-term impact of RJCs on resident learning, faculty development, and patient care.
This study underscores the need for targeted strategies to overcome structural and cultural barriers to implementing RJCs in family medicine residency programs. By investing in faculty development, securing dedicated curriculum time, and fostering a culture of engagement, programs can address the identified challenges and advance their commitment to health equity. Continued research and advocacy will be essential to ensure that RJCs become an integral part of graduate medical education, even amid shifting political and institutional landscapes.
References
-
-
Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions.
Lancet. 2017;389(10,077):1,453-1,463.
doi:10.1016/S0140-6736(17)30569-X
-
-
-
Edgoose J, Brown Speights J, White-Davis T, et al. Teaching about racism in medical education: a mixed-method analysis of a train-the-trainer faculty development workshop.
Fam Med. 2021;53(1):23-31.
doi:10.22454/FamMed.2021.408300
-
-
Sexton SM, Richardson CR, Schrager SB, et al. Systemic racism and health disparities: a statement from editors of family medicine journals.
Fam Med. 2021;53(1):5-6.
doi:10.22454/FamMed.2020.805215
-
Roett M, Archer DKL, Kudrimoti A, Elwood S. Moving the needle on racial justice in medical education: updates after the 2021 ADFM Conference session.
Ann Fam Med. 2022;20(6):580-582.
doi:10.1370/afm.2912
-
-
Beets J. From STFM: STFM solidifies antiracism initiative.
Ann Fam Med. 2021;19(6):566-567.
doi:10.1370/afm.2405
-
Smith L, Kashubeck-West S, Payton G, Adams E. White professors teaching about racism: challenges and rewards ψ.
Couns Psychol. 2017;45(5):651-668.
doi:10.1177/0011000017717705
-
Harper SR, Davis HF III. Eight actions to reduce racism in college classrooms. Academe. 2016;102(6):30-34.
-
Smedley BD, Stith AY, Nelson AR, eds; Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care.
Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; 2003. Accessed December 9, 2024.
http://www.ncbi.nlm.nih.gov/books/NBK220358
-
Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review.
Am J Public Health. 2015;105(12):e60-e76.
doi:10.2105/AJPH.2015.302903
-
Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care.
Am J Public Health. 2012;102(5):979-987.
doi:10.2105/AJPH.2011.300558
-
Hagiwara N, Slatcher RB, Eggly S, Penner LA. Physician racial bias and word use during racially discordant medical interactions.
Health Commun. 2017;32(4):401-408.
doi:10.1080/10410236.2016.1138389
-
Blair IV, Steiner JF, Havranek EP. Unconscious (implicit) bias and health disparities: where do we go from here?
Perm J. 2011;15(2):71-78.
doi:10.7812/TPP/11.979
-
Guh J, Harris CR, Martinez P, Chen FM, Gianutsos LP. Antiracism in residency: a multimethod intervention to increase racial diversity in a community-based residency program.
Fam Med. 2019;51(1):37-40.
doi:10.22454/FamMed.2019.987621
-
White-Davis T, Edgoose J, Brown Speights JS, et al. Addressing racism in medical education: an interactive training module.
Fam Med. 2018;50(5):364-368.
doi:10.22454/FamMed.2018.875510
-
Schlaff AL, Amutah-Onukagha NN, Mabiala D, Kamruddin J, Ona FF. Can US medical schools teach about structural racism?
Milbank Q. 2023;101(3):975-998.
doi:10.1111/1468-0009.12650
-
Wusu MH, Baldwin M, Semenya AM, Moreno G, Wilson SA. Racial justice curricula in family medicine residency programs: a CERA survey of program directors.
Fam Med. 2022;54(2):114-122.
doi:10.22454/FamMed.2022.189296
-
Ho T, Laskow B, Zaballa A, Moreno G. Family medicine resident perceptions on racial justice training in residency: a CERA study.
PRiMER. 2022;6:44.
doi:10.22454/PRiMER.2022.517073
-
Gertz AM, Smith M, Thomas D, Ti A, Vamos C, Bohn J. A qualitative study to explore experiences of anti-racism teaching in medical residency programs across the United States and subsequent creation of the SPOC (Support - Pipeline - Outcomes - Community) Model to guide future curricula design.
BMC Med Educ. 2024;24(1):382.
doi:10.1186/s12909-024-05305-5
-
Foster KE, Johnson CN, Carvajal DN, et al. Dear White people.
Ann Fam Med. 2021;19(1):66-69.
doi:10.1370/afm.2634
-
Sotto-Santiago S, Poll-Hunter N, Trice T, et al. A framework for developing antiracist medical educators and practitioner-scholars.
Acad Med. 2022;97(1):41-47.
doi:10.1097/ACM.0000000000004385
-
Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research.
Ann Fam Med. 2018;16(3):257-260.
doi:10.1370/afm.2228
-
Fatahi G, Racic M, Roche-Miranda MI, et al. The current state of antiracism curricula in undergraduate and graduate medical education: a qualitative study of US academic health centers.
Ann Fam Med. 2023;21(suppl 2):S14-S21.
doi:10.1370/afm.2919
-
Lehn C, Huang H, Hansen-Guzman A, et al. Longitudinal antiracism training for family medicine residency faculty.
PRiMER. 2023;7:40.
doi:10.22454/PRiMER.2023.351932
-
Falusi O, Chun-Seeley L, de la Torre D, et al. Teaching the teachers: development and evaluation of a racial health equity curriculum for faculty.
MedEdPORTAL. 2023;19:11305.
doi:10.15766/mep_2374-8265.11305
-
-
-
-
Calardo SJ, Kou M, Port C, et al. Realizing inclusion and systemic equity in medicine: upstanding in the medical workplace (RISE UP)—an antibias curriculum.
MedEdPORTAL. 2022;18:11233.
doi:10.15766/mep_2374-8265.11233
-
-
Hill Weller L, Tang J, Chen R, Boscardin C, Ehie O. Tools for addressing microaggressions: an interactive workshop for perioperative trainees.
MedEdPORTAL. 2023;19:11360.
doi:10.15766/mep_2374-8265.11360
-
-
Dennis SN, Gold RS, Wen FK. Learner reactions to activities exploring racism as a social determinant of health.
Fam Med. 2019;51(1):41-47.
doi:10.22454/FamMed.2019.704337
-
Sotto-Santiago S, Mac J, Duncan F, Smith J. “I didn’t know what to say”: responding to racism, discrimination, and microaggressions with the OWTFD approach.
MedEdPORTAL. 2020;16:10971.
doi:10.15766/mep_2374-8265.10971
-
-
Mateo CM, McCormick D, Connors C, Basu G. From theory to action: evaluation of a longitudinal project-based antiracism course for post-graduate physicians.
J Med Educ Curric Dev. 2024;11:23821205241303643.
doi:10.1177/23821205241303643
-
Sonoda K, Malhotra K, Oni K, Pratt G, Weidner AKH. Strategies and barriers for diversity, equity, inclusion, and antiracism work in family medicine departments: a CERA study.
Fam Med. 2024;56(10):672-677.
doi:10.22454/FamMed.2024.836778
-
Tarleton C, Tong W, McNeill E, Owda A, Barron B, Cunningham H. Preparing medical students for anti-racism at the bedside: teaching skills to mitigate racism and bias in clinical encounters.
MedEdPORTAL. 2023;19:11333.
doi:10.15766/mep_2374-8265.11333
-
Ackerman-Barger K, Jacobs NN, Orozco R, London M. Addressing microaggressions in academic health: a workshop for inclusive excellence.
MedEdPORTAL. 17:11103.
doi:10.15766/mep_2374-8265.11103
-
DiAngelo DR. White Fragility: Why Understanding Racism Can Be So Hard for White People (Adapted for Young Adults). Beacon Press; 2022.
-
Peek ME, Vela MB, Chin MH. Practical lessons for teaching about race and racism: successfully leading free, frank, and fearless discussions.
Acad Med. 2020;95(12S):S139-S144.
doi:10.1097/ACM.0000000000003710
-
Ortega AN, Roby DH. Ending structural racism in the US health care system to eliminate health care inequities.
JAMA. 2021;326(7):613-615.
doi:10.1001/jama.2021.11160
-



There are no comments for this article.