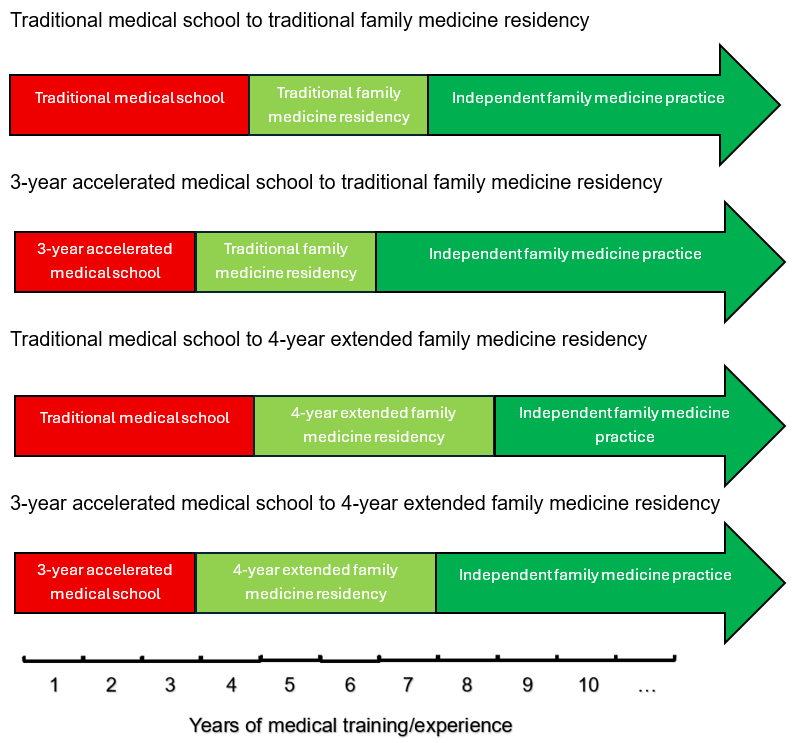
We read the article by Carney et al reporting on the Length of Training Pilot (LoTP) with great interest. 1 With the end of the LoTP, length-of-training work has transitioned to the Family Medicine Advancing Innovations in Residency Education (FM-AIRE) initiative, which promotes 4-year family medicine residency programs to enhance clinical preparedness and expanded scope of practice. 2, 3 Complementary, length-of-training innovations in undergraduate medical education (UME) are now graduating medical students through 3-year accelerated programs. Many of these shortened training pathways foster the choice of a primary care residency while also limiting medical school debt.4 Aligning these two models into a 3+4 training pathway (3 years of UME followed by 4 years of graduate medical education [GME]) could enhance both components of medical training.
A 3-year medical school program reduces tuition costs and provides quicker access to relevant clinical experiences.5 This streamlined approach benefits motivated learners by minimizing electives while reinforcing early professional identity. With 1 less year of tuition debt, students may be more likely to choose primary care.5 Additionally, several programs offer direct entry into primary care residencies within the same institutions. 6 This accelerated schedule, though, limits exposure to other specialties, reducing flexibility for career exploration and limiting opportunities to reinforce foundational knowledge.7 The compression of an already intense class load also increases the risk of burnout. 7
A 4-year family medicine residency program allows learners to keep the benefits of an accelerated UME experience while also addressing these shortcomings. Four-year extended training programs afford learners the flexibility to pursue additional rotations such as geriatrics, sports medicine, and procedural care.3 As Carney et al showed, graduates of 4-year residency programs were more clinically prepared and pursued a broader scope of practice. Four-year family medicine residency programs offer additional opportunities to hone core skills, foster leadership, and increase scholarly output. Longer residency training, however, delays entry into independent practice and its increased earning potential.
A structured 3+4 pathway mitigates the financial concerns of the 4-year family medicine GME program while maximizing its educational opportunities (Figure 1). A shortened UME duration reduces costs and accelerates clinical immersion, while the extended GME structure ensures comprehensive preparedness. The 3+4 pathway equates to the same 7 years that 4 years of UME and 3 years of GME would, but it adds the benefits just described. Financially, this pathway would reduce accumulated debt from medical school and add a year of resident salary.



There are no comments for this article.