Background and Objectives: This study sought to quantify the anecdotally reported experience of decredentialing in the profession of medicine, specifically as it applies to gender. Decredentialing is defined as the experience of being addressed by first name without permission or being mistaken as a nonphysician provider.
Methods: Eight questions regarding decredentialing microaggressions and resultant stress reactions were submitted as part of the 2023 Council of Academic Family Medicine Educational Research Alliance general membership survey.
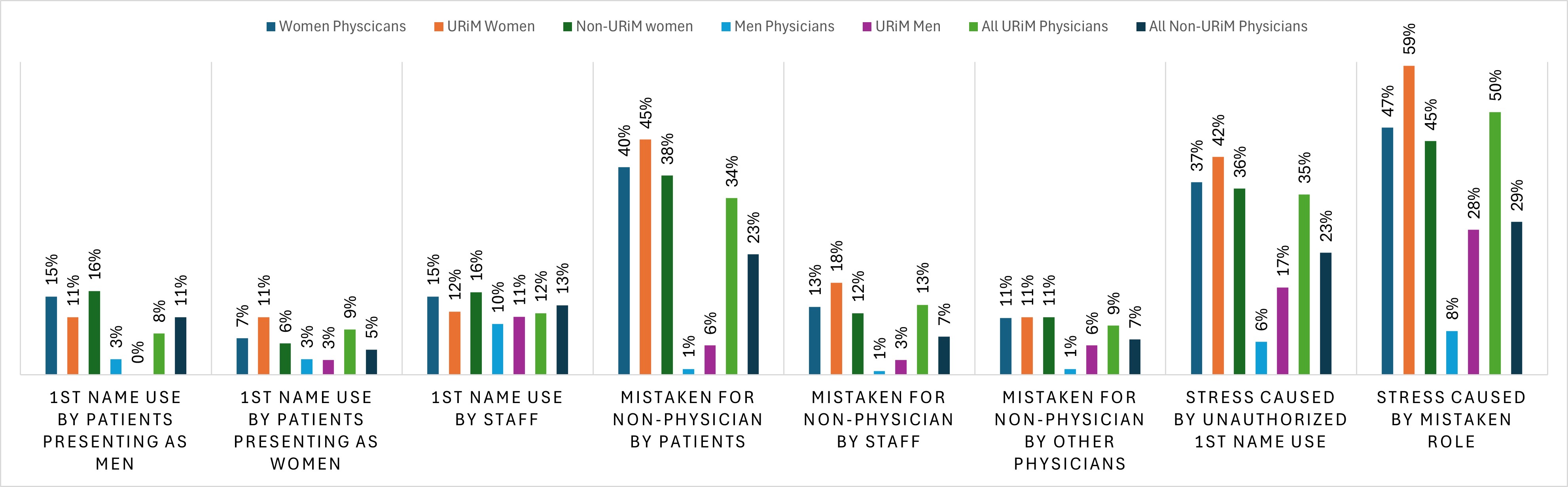
Results: Women physicians reported significantly higher rates of unauthorized first name use by patients (15% vs 3% for men patients; 7% vs 3% for women patients). Women physicians also reported significantly higher rates of decredentialing by being mistaken as a nonphysician by patients (39.8% frequent vs 1.1%), clinical staff (13.0% frequent vs 0.7%), and other physicians (10.9% frequent vs 1.1%). Women respondents reported more substantial stress responses after unauthorized first-name use (36.9% more stressful vs 6.3%) and mistaken roles (47.7% more stressful vs 8.4%). Subgroup analysis of self-identified underrepresented in medicine (URiM) populations showed significantly higher rates of microaggressions among URiM women physicians compared to men physicians and in total URiM respondents versus non-URiM respondents.
Conclusions: Women physicians experience the gender microaggression of decredentialing via unauthorized first-name use by patients and being mistaken for a nonphysician more frequently than men physicians. Women physicians also more frequently experience a stress response from these microaggressions. Decredentialing, long acknowledged anecdotally by women physicians, is a valid gender microaggression disproportionately affecting women physicians.
Nearly 200 years after Elizabeth Blackwell graduated from Geneva medical school in 1849, women physicians continue to endure a spectrum of prejudices from overt sexism to gender microaggressions.1, 2 According to Association of American Medical Colleges data, women represent only 16% of medical school deans, 25% of full professors in medicine, and 18% of department chairs.3 Many large social, structural, and economic forces contribute to the gender pay/leadership gap in medicine, but unconscious bias has been described as contributing to ongoing inequities. 4, 5
Microaggressions are subtle verbal or nonverbal behaviors that often arise from unconscious biases, prejudices, or underlying hostility toward others based on race, ethnicity, gender, sexual orientation, religion, or other personal characteristics.1 They are often brief, may be intentional or unintentional, often are unacknowledged by the recipient, and occur in a large variety of settings. Microaggressions are a crucial phenomenon for medical learners to understand to provide appropriate clinical care. For example, gendered racial microaggressions experienced by patients of color during obstetric care have been associated with elevated postpartum blood pressure.6
Furthermore, learners also are directly affected by personal experiences of microaggressions in clinical and educational environments. Experiencing microaggressions of any kind has been shown to be associated with depressive symptoms in medical students, and medical students who identify as underrepresented in medicine (URiM) have reported higher rates of microaggressions, which have correlated with feelings of burnout and compromised learning.7- 9 Studies also have shown that women physicians experience gender microaggressions during both training and in the residency interview process.1, 10, 11 For example, women residents perceive that they receive less attention from nurses, get less assistance with tasks, and are evaluated more harshly than men residents. 11
One form of microaggression is decredentialing. For the purposes of our study, the term decredentialing is used to encompass the previously described phenomena of untitling women physicians(ie, not addressing them with their professional title) and misidentifying women physicians as nurses or other staff.12- 15 Decredentialing is often done without malice but can reflect unconscious bias and adversely affect the perceived authority and credibility of the target.13 Harvey and colleagues examined the use of physicians’ first name specifically within the electronic medical record written correspondences. They found that women physicians had more than twice the odds as their male counterparts to be addressed by their first name, even after adjusting for age, degree, and specialty.15 However, the incidence of physician experience with decredentialing in a broader clinical context in the field of family medicine has not been formally studied, nor has the stress impact of decredentialing been examined.
In this nationwide survey of practicing family physicians, we attempted to build on the existing literature regarding the gender microaggression of decredentialing as experienced by women versus men physicians. We also sought to understand whether being self-identified as URiM made decredentialing more likely and whether this experience more often resulted in a negative emotional response.
Eight questions focusing on decredentialing microaggressions and resultant stress reactions were submitted as part of the 2023 Council of Academic Family Medicine (CAFM) Educational Research Alliance (CERA) general membership survey of family medicine educators and practicing physicians. CAFM members were invited to propose survey questions for inclusion in the CERA survey. Approved projects were evaluated and questions reviewed for consistency with the overall subproject aim, readability, and existing evidence of reliability and validity. During pretesting, conducted with family medicine educators who were not included in the sampling frame, questions were evaluated for flow, timing, and readability. The study was approved by the American Academy of Family Physicians Institutional Review Board in November 2023.
Participants were selected based on membership type and credentials, with the goal of selecting only active medical clinicians belonging to one of the CAFM organizations and having an address in the United States. The pool was limited by excluding residency program directors, clerkship directors, and department chairs; these sample groups were excluded due to their participation in other, more specialized survey panels. Data were collected through SurveyMonkey (SurveyMonkey Inc).
The survey was distributed to 3,879 potential participants. Of these, 155 were returned with undeliverable email addresses, and 49 who had previously opted out of receiving surveys from SurveyMonkey also were excluded. The survey was delivered to a final sample of 3,675 members of the CAFM organizations. The survey contained qualifying questions for participation in the survey. Seventy-seven people failed to meet qualifications and were removed from the sample pool, leaving a sample size of 3,598. The survey was conducted between November 20, 2023, and December 22, 2023. Self-reported demographics of the sample pool are based on membership data from the Association of Departments of Family Medicine, the North American Primary Care Research Group, and the Society of Teachers of Family Medicine, including geographic region, degree earned, gender, age, race/ethnicity, and self-identification as URiM. 16
The main outcomes measured were the average frequency of self-reported incidents of decredentialing microaggressions and the amount of stress these incidents produce. Six questions focused on microaggression frequency:
-
How often are you addressed by your first name only (without your professional title or permission) by patients who are men?
-
How often are you addressed by your first name only (without your professional title or permission) by patients who are women?
-
How often do clinical or hospital staff address you by your first name only (without your professional title or permission)?
-
How often have patients mistaken you for a nonphysician provider, such as a nurse?
-
How often have other physicians mistaken you for a nonphysician provider?
-
How often have clinical or hospital staff mistaken you for a nonphysician provider?
Two questions focused on a negative stress response resulting from decredentialing:
-
Is it stressful to be addressed by your first name without permission in a professional setting?
-
Is it stressful to be mistaken as a nonphysician in a clinical setting?
Frequency was measured with Likert-scale questions from 0=never to 4=always. Level of stress produced by these incidents also was measured with Likert-scale questions from 0=not at all to 3=extremely stressful.
Statistical Analysis
We computed descriptive analyses (frequencies and percentages) for demographics, practice setting, and responses to questions regarding decredentialing and the resultant stress reaction. We used χ2 comparisons to examine differences in response patterns to questions 1 through 8 based on the key demographic variables such as gender, self-identification as URiM, age, size of community, and practice setting. Data were aggregated into dichotomous categories. For microaggression frequency, we compared the category of “seldom” (comprised of the never, rarely, and sometimes combined) to “frequent” (comprised of often and always). For the resultant stress reaction analysis, we compared the dichotomous categories of “less stressful” (comprised of not at all stressful and minimally stressful) to “more stressful” (comprised of moderately stressful and extremely stressful). All data analyses were performed using SPSS version 26.0 (IBM) and Microsoft Excel.
Participants
The total number of responses to the overall survey was 972. Accounting for the 77 people who did not meet the qualifications for the survey, the number of responses was reduced to 895. Additionally, 62 people who answered only qualifying questions were removed from the responses, but not from the sample pool. The overall response rate for the survey was 23.15% (833/3,598), which is typical for online surveys.15 More than half of respondents (n=500, 61.3%) identified as women, and 312 respondents (38.2%) identified as men. Less than 1% of respondents identified as genderqueer or nonbinary. Respondents were allowed to self-identify as URiM, and 155 respondents (18.8%) replied “yes” to identifying as URiM while 671 respondents (81.2%) replied “no” to identifying as URiM. Relevant demographics are summarized in Table 1.
|
Demographic
|
Count (valid %*)
|
|
Gender
|
|
Women
|
500 (60.1)
|
|
Men
|
312 (37.5)
|
|
Other identity
|
20 (2.3)
|
|
URiM / not URiM
|
|
Total
|
155 (18.8) / 671 (81.2)
|
|
Women
|
107 (22) / 390 (78)
|
|
Men
|
45 (15) / 265 (85)
|
|
Other identity
|
3 (16) / 16 (84)
|
|
Age
|
|
<46
|
388 (55.3)
|
|
>47
|
313 (44.7)
|
|
Setting
|
|
Outpatient only
|
294 (59.3)
|
|
Inpatient or combination
|
202 (40.7)
|
Decredentialing in Women Versus Men Physicians
Women physicians reported significantly higher rates of decredentialing by first name use without permission by both men and women patients. For patients that presented as men, 15% of women physicians reported frequent first-name decredentialing vs 3% of men physicians (χ2=24.47, P<.001, RR=5.03, 95% CI=2.46–10.32). For patients that presented as women, 7% of women physicians reported frequent first-name decredentialing vs 3% of men physicians (χ2=4.5, P=.034, RR=2.35, 95% CI=1.10–5.05). The differences between men and women physicians in response to first-name use by clinical staff was not significant. For decredentialing by mistaken role (being identified as a nonphysician), women physicians also reported significantly higher rates of microaggressions with patients (women respondents 39.8% frequent vs men respondents 1.1%, χ2=130.63, P<.0001, RR=35.66, 95% CI=11.51–110.52), clinical staff (women respondents 13.0% frequent vs men respondents 0.7%, χ2=31.00, P<.001, RR=17.4, 95% CI=4.28–70.68), and other physicians (women respondents 10.9% frequent vs men respondents (1.1%, P<.001, RR=9.77, 95% CI=3.07; Figure 1).
Women physicians reported significantly higher stress responses after decredentialing by first name use without permission and by mistaken roles. For 36.9% of women physicians, unauthorized first-name use was reported as “more stressful” versus 6.3% of men physicians (χ2=80.97, P<.001, RR=5.84, 95% CI=3.63–9.40). Similarly, for 47.7% of women physicians, being labeled in a mistaken role was reported as “more stressful” versus 8.4% of men physicians (χ2=113.58, P<.001, RR=5.71, 95% CI=3.78–8.61; Table 2).
|
|
Women physicians
|
URiM women
|
Non-URiM women
|
Men physicians
|
URiM men
|
All URiM physicians
|
All non-URiM physicians
|
|
|
%
|
RR
|
95% CI
|
%
|
RR
|
95% CI
|
%
|
RR
|
95% CI
|
%
|
RR
|
95% CI
|
%
|
RR
|
95% CI
|
%
|
RR
|
95% CI
|
%
|
RR
|
95% CI
|
|
First name use by patients presenting as men
|
15**
|
5.03
|
2.46–10.32
|
11
|
0.68
|
0.36–1.28
|
16
|
1.46
|
0.77–2.75
|
3**
|
0.2
|
0.10–0.41
|
0
|
N/A
|
N/A
|
8
|
0.71
|
0.38–1.30
|
11
|
1.4
|
0.74–2.65
|
|
First name use by patients presenting as women
|
7*
|
2.35
|
1.10–5.05
|
11
|
1.83
|
0.89–3.75
|
6
|
0.55
|
0.29–1.03
|
3*
|
0.42
|
0.20–0.90
|
3
|
0.91
|
0.12–7.18
|
9
|
1.79
|
0.90–3.50
|
5
|
0.56
|
0.29–1.06
|
|
First name use by staff
|
15
|
1.55
|
1.01–2.38
|
12
|
0.76
|
0.42–1.39
|
16
|
1.31
|
0.70–2.46
|
10
|
0.64
|
.029–1.37
|
11
|
1.17
|
0.43–3.20
|
12
|
0.89
|
0.53–1.50
|
13
|
1.13
|
0.60–2.14
|
|
Mistaken for nonphysician by patients
|
40**
|
35.66
|
11.51–110.52
|
45
|
1.18
|
0.91–1.54
|
38
|
0.85
|
0.45–1.60
|
1**
|
0.03
|
0.01–0.06
|
6
|
12.83
|
1.19–137.9
|
34*
|
1.46
|
1.10–1.90
|
24*
|
0.68
|
0.36–1.29
|
|
Mistaken for nonphysician by staff
|
13**
|
17.4
|
4.28–70.68
|
18
|
1.49
|
0.88–2.53
|
12
|
0.67
|
0.36–1.26
|
1**
|
0.06
|
0.03–0.13
|
3
|
3.39
|
0.41–100
|
13*
|
1.84
|
1.10–3.10
|
7*
|
0.54
|
0.29–1.02
|
|
Mistaken for nonphysician by other physicians
|
11**
|
9.77
|
3.07–31.05
|
11
|
1
|
0.52–1.93
|
11
|
1
|
0.53–1.88
|
1**
|
0.1
|
0.05–0.21
|
6
|
12.78
|
1.19–137.4
|
9
|
1.4
|
0.75–2.60
|
7
|
0.72
|
0.38–1.36
|
|
Stress caused by unauthorized First name use
|
37**
|
5.84
|
3.63–9.40
|
42
|
1.17
|
0.88–1.55
|
36
|
0.86
|
0.46–1.62
|
6**
|
0.17
|
0.08–0.36
|
17*
|
3.5
|
1.38–8.88
|
35*
|
1.48
|
1.10–2.00
|
23*
|
0.67
|
0.35–1.27
|
|
Stress caused by mistaken role
|
47**
|
5.71
|
3.78–8.61
|
59*
|
1.32
|
1.07–1.62
|
45*
|
0.76
|
0.40–1.43
|
8**
|
0.18
|
0.08–0.39
|
28*
|
5.23
|
2.44–11.21
|
50**
|
1.72
|
1.40–2.10
|
29**
|
0.58
|
0.31–1.10
|
Decredentialing in URiM Women Versus Non-URiM Women Physicians
We found no statistically significant differences between URiM and non-URiM women in terms of unauthorized first name use or mistaken roles. However, URiM women physicians reported significantly higher stress responses after decredentialing by mistaken roles versus non-URiM women physicians. Of URiM women respondents, 59.3% reported decredentialing as “more stressful” vs 44.8% of non-URiM women respondents (χ2=5.52, P=.019, RR=1.32, 95% CI=1.07–1.62).
Comparisons between URiM women and URiM men physicians revealed that mistaken roles by patients and increased stress response to unauthorized first-name use and mistaken roles were the only stastitically significant results, disproportionately affecting women physicians. Of the comparisons between all URiM and all non-URiM respondents, mistaken roles by patients and staff, and subsequent stress response for both first-name use and mistaken roles were significantly higher in URiM participants.
The role of gender in the use of professional address has been highlighted by two recent studies of speaker introduction at conferences and grand rounds. Studies in both 2017 and 2019 showed that women speakers were less likely to be addressed by their professional title then men at grand rounds and at an international oncology conference.17, 18 Harvey et al more recently reported that women physicians were more likely than men physicians to be greeted by their first name in patient portal messages.15 However, that study did not account for whether physicians had given prior permission for first-name use or whether first-name use had been set as precedent in prior in-person visits. Furthermore, whether or not physicians also viewed these incidents in a negative light was unaddressed. Our study looked specifically at first-name use without physician consent and being mistaken for a nonphysician in a broader clinical context than previously reported. Additionally, we examined the stress response from decredentialing microaggressions.
Overall, our results showed that women physicians were significantly more likely to be referred to by first-name without permission by patients of both genders and were more frequently being mistaken for nonphysicians than men physicians by patients, staff, and physician colleagues. The greatest risk of decredentialing was seen with patients assigning nonphysician roles to women physicians (RR=35.66, 95% CI=11.51–110.52). Moreover, the bias of viewing women physicians as less than their professional title is unrestricted: It comes from patients, coworkers, and physician colleagues. Of note, both men and women patients decredential women physicians by mistaken roles, suggesting that this implicit bias exists regardless of patient gender.
Patients who identified as men were significantly more likely to use a woman physician’s first name without permission (RR=5.03, 95% CI=2.46–10.32) compared to women patients, though women patients were still sigificantly more likely to do so with women physicians than with men physicians (RR=2.35, 95% CI=1.10–5.05). Unauthorized first-name usage by staff, while higher for women physicians absolutely, did not reach statistical significance either between groups or by RR (RR=1.55, 95% CI=1.01–2.38). Both local work/office culture and/or explicit permission for first-name use may mitigate the occurrence of decredentialing from staff, although further studies are needed.
One explanation for first-name decredentialing is the assumption of traditional binary gender expression, which suggests that women are warmer, more approachable, and more accepting of a less formal address. Another hypothesis explaining the observed difference is that title usage is not as accurate a reflection of patients’ perception of role as other verbal cues, such as asking a physician for their medications or a bedpan. Finally, a possibility is that being mistaken for a nonphysician is more memorable than first-name usage, leading to increased reporting (recall bias).
Women physicians reported higher resultant stress from both mislabeling and unauthorized first-name use microaggressions. To our knowledge, this study is the largest survey of family doctors specifically that reports a greater stress impact on women physicians than on men physicians. These results support similar studies demonstrating an association between microaggressions among marginalized populations and poorer mental health outcomes. 19- 21
The phenomenon of decredentialing by mistaken roles exemplifies previously described implicit bias about women in several categories: assumptions of inferiority, assumptions of traditional gender roles, and expectations of appearance.22 The cause of mistaken roles cannot be directly determined in this study, but one could postulate that a woman in the role of a physician challenges traditional expectations of gender, even in the 21st century. A 2024 observational study published in JAMA showed that hospitalized patients cared for by women internists had fewer readmissions and lower mortality than patients cared for by men physicians.23 Despite this indirect evidence that women physicians provide equal (if not better) care than their men counterparts, our study reveals that women are repeatedly subjected to microaggressions from others that imply otherwise.
We attempted to determine the role, if any, that URiM status had on decredentialing microaggression. Examining several subgroup comparisions (URiM women with non-URiM women, URiM women with URiM men, and all URiM vs all non-URiM respondents), we observed these trends: URiM status was not a significant risk factor for decredentialing when comparing URiM women to non-URiM women; when comparing URiM women to URiM men, gender for several microaggressions persisted to disproportionately affect women more than men physicians. This finding implies that gender is a more robust risk factor for decredentialing when compared to URiM status among women physicians. However, when comparing all URiM to non-URiM respondents, we found that mistaken roles by patients and staff did occur significant more frequently in URiM participants. Taken as a whole, our data suggest that while gender is the strongest predictor of decredentialing, URiM is also a significant risk factor. The role of URiM and race in the context of professional decredentialing should be the focus of further research.
Strengths
Through our survey questions, we sought to specifically define the potential differences between decredentialing behavior patterns in patient-physician dyads where gender was matched versus mismatched. To our knowledge, our study is one of the first to objectively demonstrate a gender disparity with misidentification as a nonphysician between men and women family physicians. Our study also involved a survey of predominantely postresidency physicians, unlike other studies that included primarily trainees. 12, 13
We also showed a relationship between decredentialing and a more frequent resultant stress reaction in women physicians, making a strong argument for this type of decredentialing being classified as a validated gender microaggression. While other studies have examined the first-name use disparity between men and women physicians, we explicitly examined usage without permission and the emotional response from these behaviors.
Limitations
The response rate for our survey was 23%; the CERA committee cited a lower response rate to its general membership survey postpandemic that mirrored national trends. Therefore, whether the respondents represented a generalizable sample of practicing family physicians is unclear. Furthermore, this was a study exclusively of family physicians within CAFM; therefore, whether these results can be applied to physicians in other specialties is unknown. Additionally, statistical analyses comparing URiM men to some other subpopulations was impossible due to expected cell values falling below required frequency thresholds, making χ2 results unreliable.
Resident physicians were excluded from this survey because they are surveyed separately by CERA; this limited our ability to query younger physicians. Additionally, in the year of this CERA survey cycle, unfortunately no resident-focused survey was distributed. Only four respondents identified as genderqueer/gender-nonconforming or nonbinary, making this sample too small to analyze statistically.
Given the cross-sectional design of our study, these data are subject to possible recall bias, and we were unable to longitudinally analyze the effects of decredentialing microaggressions. However, our study design and use of questionnaires is consistent with other studies published on racial and gender microaggression.1, 22 Future experimental designs would further establish a causal relationship between decredentialing and stress or negative emotions.
Our study showed that decredentialing is a gender microaggression experienced more often by women and results in a stress response. Addressing gender microaggressions—including decredentialing, both in residency curriculum and when observed clinically—is important to promote an inclusive environment that will result in retention of women physicians in the field of medicine. This study demonstrated that what is often anecdotally described by women physicians—being referred to by first name without explicit permission or being mistaken for a nonphysician provider—is a quantifiable gender disparity. Self-identified status as a URiM physician was not a significant risk factor for decredentialing when comparing women physicians in this study. However, when examined as a whole, URiM physicians did experience a greater risk of mistaken roles by patients and staff compared to non-URiM physicians. This finding indicates that URiM status is also an independent risk factor for decredentialing microaggressions.
Decredentialing is both a reflection bias (conscious or unconscious) and a microaggression that perpetuates gender inequity in the profession of family medicine. Based on the findings of our study, decredentialing should be recognized and addressed by family medicine educators. Further research is needed to elucidate other contributory risk factors for decredentialing and ways that organizations and our profession can move toward eliminating this oft-discussed but relatively understudied gender-disparity for women physicians.
Acknowledgments
The authors thank the 2023 Council of Academic Family Medicine Educational Research Alliance.
References
-
Sudol NT, Guaderrama NM, Honsberger P, Weiss J, Li Q, Whitcomb EL. Prevalence and nature of sexist and racial/ethnic microaggressions against surgeons and anesthesiologists.
JAMA Surg. 2021;156(5):e210265.
doi:10.1001/jamasurg.2021.0265
-
-
- Fry R, Aragao C. Gender pay gap in U.S. has narrowed slightly over 2 decades. Pew Research Center; March 4, 2025. Accessed April 15, 2024. https://www.pewresearch.org/short-reads/2023/03/01/gender-pay-gap-facts
-
-
Janevic T, Howell FM, Burdick M, et al. Racism and postpartum blood pressure in a multiethnic prospective cohort.
Hypertension. 2025;82(2):206-215.
doi:10.1161/HYPERTENSIONAHA.124.23772
-
Walls ML, Gonzalez J, Gladney T, Onello E. Unconscious biases: racial microaggressions in American Indian health care.
J Am Board Fam Med. 2015;28(2):231-239.
doi:10.3122/jabfm.2015.02.140194
-
Anderson N, Lett E, Asabor EN, et al. The association of microaggressions with depressive symptoms and institutional satisfaction among a national cohort of medical students.
J Gen Intern Med. 2022;37(2):298-307.
doi:10.1007/s11606-021-06786-6
-
Chisholm LP, Jackson KR, Davidson HA, Churchwell AL, Fleming AE, Drolet BC. Evaluation of racial microaggressions experienced during medical school training and the effect on medical student education and burnout: a validation study.
J Natl Med Assoc. 2021;113(3):310-314.
doi:10.1016/j.jnma.2020.11.009
-
Hoi KK, Kana LA, Sandhu G, et al. Gender microaggressions during virtual residency interviews and impact on ranking of programs during the residency match.
J Grad Med Educ. 2022;14(4):398-402.
doi:10.4300/JGME-D-21-00927.1
-
Molina MF, Landry AI, Chary AN, Burnett-Bowie SM. Addressing the elephant in the room: microaggressions in medicine.
Ann Emerg Med. 2020;76(4):387-391.
doi:10.1016/j.annemergmed.2020.04.009
-
Chang J, Arbo J, Jones MP, Silverberg J, Corbo J. Mitigating the gender gap: How “doctor” badges affect physician identify.
Am J Emerg Med. 2021;46: 141-145:
doi:10.1016/j.ajem.2021.04.037
-
Berwick S, Calev H, Matthews A, et al. Mistaken identity: frequency and effects of gender-based professional misidentification of resident physicians.
Acad Med. 2021;96(6):869-875.
doi:10.1097/ACM.0000000000004060
-
-
Harvey JA, Butterfield RJ, Ochoa SA, Yang YW. Patient use of physicians’ first (given) name in direct patient electronic messaging.
JAMA Netw Open. 2022;5(10):e2234880.
doi:10.1001/jamanetworkopen.2022.34880
-
-
Files JA, Mayer AP, Ko MG, et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias.
J Womens Health (Larchmt). 2017;26(5):413-419.
doi:10.1089/jwh.2016.6044
-
Duma N, Durani U, Woods CB, et al. Evaluating unconscious bias: speaker introductions at an international oncology conference.
J Clin Oncol. 2019;37(36):3,538-3,545.
doi:10.1200/JCO.19.01608
-
Lui PP, Quezada L. Associations between microaggression and adjustment outcomes: a meta-analytic and narrative review.
Psychol Bull. 2019;145(1):45-78.
doi:10.1037/bul0000172
-
Wright T, Lewis G, Greene T, et al. The association between microaggressions and mental health among UK trans people: a cross-sectional study.
Soc Psychiatry Psychiatr Epidemiol. 2025;60:1,211-1,225.
doi:10.1007/s00127-024-02775-2
-
Nadal KL, Wong Y, Sriken J, Griffin K, Fujii-Doe W. Racial microaggressions and Asian Americans: an exploratory study on within-group differences and mental health.
Asian Am J Psychol. 2015;6(2):136-144.
doi:10.1037/a0038058
-
Derthick A. The Sexist MESS: Development and Initial Validation of the Sexist Microaggressions Experiences and Stress Scale and the Relationship of Sexist Microaggressions to Women’s Mental Health. Dissertation. University of Alaska; 2015.
-
Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians.
JAMA Intern Med. 2017;177(2):206-213.
doi:10.1001/jamainternmed.2016.7875



There are no comments for this article.