Background and Objectives: Climate change is a major threat to the health of people worldwide. The health care system deals with the immediate health-related effects of climate change and, at the same time, is a major emitter of greenhouse gas. This study aimed to investigate (a) the awareness and perception of climate change among family medicine residency program directors, and (b) the state of climate change education in family medicine residency programs.
Methods: The Council of Academic Family Medicine Educational Research Alliance (CERA) conducted a cross-sectional survey of family medicine program directors in the United States in April 2023. We analyzed anonymous data using descriptive and bivariate statistics.
Results: We analyzed responses from 284 family medicine residency program directors (response rate 41.1%). Of these, 56.8% indicated not having any lectures/seminars dedicated to climate change and no plans to introduce such curricula, with considerably higher rates in East South Central United States (92.8%). A majority considered principles of climate change, carbon emissions emitted by the health care system, and discussion of climate change with patients of lesser importance for residency program education.
Conclusions: While climate change is an emerging topic affecting health and the provision of health care worldwide, our study suggests that many family medicine residency programs do not teach about it. Family medicine trainees may not always receive sufficient education about the risks posed to their patients by climate change, which could lead to them having limited knowledge and skills when discussing this topic with their patients in the future.
Climate change is a pressing global concern, representing one of the most significant challenges facing humanity in the 21st century. 1 The consequences of human-induced climate change already are having a substantial impact on the health and well-being of millions of people worldwide. 2 Primary care providers already are treating patients with health problems resulting from the changed climate, such as heat-related illness 3, 4 and mental health problems after experiencing extreme weather events. 5-7 Notably, the health care sector itself is a significant contributor to the issue, responsible for 8% to 10% of national greenhouse gas emissions in the United States. 8, 9 Greenhouse gas and toxic air pollutants from the US medical system were responsible for the loss of an estimated 388,000 disability-adjusted life years in 2018. 10 This reality places a profound moral and social responsibility on the entire health care sector. 11 Primary care providers can exert influence through their entrusted status in the communities they serve by providing education to patients on health concerns related to climate change. 12 Studies have highlighted that providers have enormous leverage through prescription and medication use to reduce the carbon footprint, for example, by reducing the prescription of particularly harmful metered-dosed inhalers and the use of inhaled anesthetics. 13- 16
Since the late 1980s, the call has been growing for physicians to assume a more proactive role in addressing climate change. 17, 18 Subsequently, several authors have highlighted the importance of including climate change in medical curricula. 19-24 Though they differ in magnitude and quality of teaching programs, many European medical schools have successfully implemented lecture series, seminars, or workshops on climate change. 25-27
In 2019, the American Medical Association (AMA) urged the inclusion of climate change in medical education, affirming its importance. 28 Though a promising step, a standardized curriculum on climate change in medical education is still pending. While some medical schools have included such curricula, widespread adoption remains uncertain. 29
A recent study showed that 29% of primary care providers doubted the existence of global warming, the human influence on climate change, or the effect of climate change on weather patterns. 30 Climate change is impacting health care through increased heat-related illnesses, wildfires, floods, deteriorating air quality leading to respiratory conditions, and a rise in infectious diseases due to the Earth’s higher temperature. 31-33
While a proposed framework for a residency curriculum on climate change exists, 29 this study assessed whether climate change topics already are taught in family medicine residency programs, which topics are perceived as important, and how program directors perceive climate change personally. In this paper, we provide results from a recurring survey among family medicine residency programs in the United States. 34
This cross-sectional online survey of family medicine program directors in the United States was conducted between April 18 and May 12, 2023. This study was part of a larger omnibus survey of the Council of Academic Family Medicine Educational Research Alliance (CERA). Results are reported following the consensus-based Checklist for Reporting of Survey Studies. 35
Questionnaire Development
The first survey segment covered demographics of program directors (gender, race/ethnicity, self-identification as underrepresented in medicine, years of professional experience) and organizational details of their programs (residency program type, affiliation, state, community size, and total resident count). To ensure privacy, program locations were categorized into nine regions (Table 1). This segment was predefined by the CERA Steering Committee. 34, 36
|
|
Survey respondents
N=284, n (%)
|
AFMRD program directors/US FM residency programsh
N=545, n (%)
|
P
|
|
Characteristics of residency program directors
|
|
Gendera
|
Female/woman
|
153 (54.6)
|
231 (49.5)
|
.259
|
|
Male/man
|
124 (44.3)
|
226 (48.4)
|
|
Choose not to disclose
|
3 (1.1)
|
10 (2.1)
|
|
Race/ethnicity
|
American Indian/Alaska Native/Indigenous
|
3 (1.1)
|
3 (0.6)
|
<.001
|
|
Asian
|
26 (9.2)
|
56 (10.6)
|
|
Black/African American
|
16 (5.7)
|
24 (4.5)
|
|
Hispanic/Latino/of Spanish origin
|
22 (7.8)
|
29 (5.5)
|
|
Middle Eastern/North African
|
3 (1.1)
|
11 (2.1)
|
|
White
|
214 (75.6)
|
329 (62.2)
|
|
Choose not to disclose
|
9 (3.2)
|
77 (14.6)
|
|
Underrepresented in medicinec
|
‑‑
|
52 (18.6)
|
72 (15.4)
|
.248
|
|
Experience as program directord
|
Years, mean (SD)
|
6.8 (5.9)
|
n/a
|
n/a
|
|
Characteristics of residency program
|
|
Typee
|
University-based
|
47 (16.6)
|
78 (10.4)
|
<.001
|
|
Community-based, university-affiliated
|
163 (57.6)
|
404 (54.1)
|
|
Community-based, nonaffiliated
|
65 (23.0)
|
251 (33.6)
|
|
Military
|
1 (0.4)
|
12 (1.6)
|
|
Other
|
7 (2.5)
|
2 (0.3)
|
|
Locationf
|
New England
|
8 (2.8)
|
20 (2.7)
|
.422
|
|
Middle Atlantic
|
40 (14.1)
|
113 (15.1)
|
|
South Atlantic
|
47 (16.5)
|
128 (17.1)
|
|
East South Central
|
13 (4.6)
|
40 (5.4)
|
|
East North Central
|
43 (15.1)
|
149 (19.9)
|
|
West South Central
|
35 (12.3)
|
75 (10)
|
|
West North Central
|
29 (10.2)
|
50 (6.7)
|
|
Mountain
|
27 (9.5)
|
58 (7.8)
|
|
Pacific
|
42 (14.8)
|
114 (15.3)
|
|
Size of community in which program is located
|
Less than 30,000
|
33 (11.6)
|
n/a
|
n/a
|
|
30,000 to 74,999
|
39 (13.7)
|
|
75,000 to 149,000
|
56 (19.7)
|
|
150,000 to 499,999
|
72 (25.4)
|
|
500,000 to 1 million
|
35 (12.3)
|
|
More than 1 million
|
49 (17.3)
|
|
Total residents enrolledg
|
Less than 19
|
112 (39.6)
|
n/a
|
n/a
|
|
19–31
|
127 (44.9)
|
|
More than 31
|
44 (15.5)
|
The second part of the survey comprised two questions on program directors’ perception of climate change. These questions, derived from the questionnaire of the Yale Program on Climate Change Communication, included a short definition of global warming. 37 Subsequently, program directors were queried about efforts to reduce CO² emissions in their programs/clinics and about the inclusion of dedicated lectures/seminars on climate change. Regardless of whether a program had a specific curriculum, directors were then prompted to rate the importance of certain topics (principles of climate change, heat-related illness, disaster preparedness, health care system’s impact on carbon emissions, discussion of climate change with patients). We used a discursive process to develop questions related to existing literature on climate change education in medicine. Questions were evaluated and revised externally through the CERA Steering Committee and checked for consistency, readability, and existing evidence of reliability and validity. Pretesting was done on family medicine educators who were not part of the target population.
The fielded survey is available online as Appendix A.
Sample and Data Collection
The target population for this survey study was all program directors of all family medicine residency programs in the United States accredited by the Accreditation Council for Graduate Medical Education (ACGME). The sampling frame of N=745 program directors was somewhat lower than the overall number of family medicine residency programs (N=747) in the United States. 38 This difference was due to brand new programs not yet included.
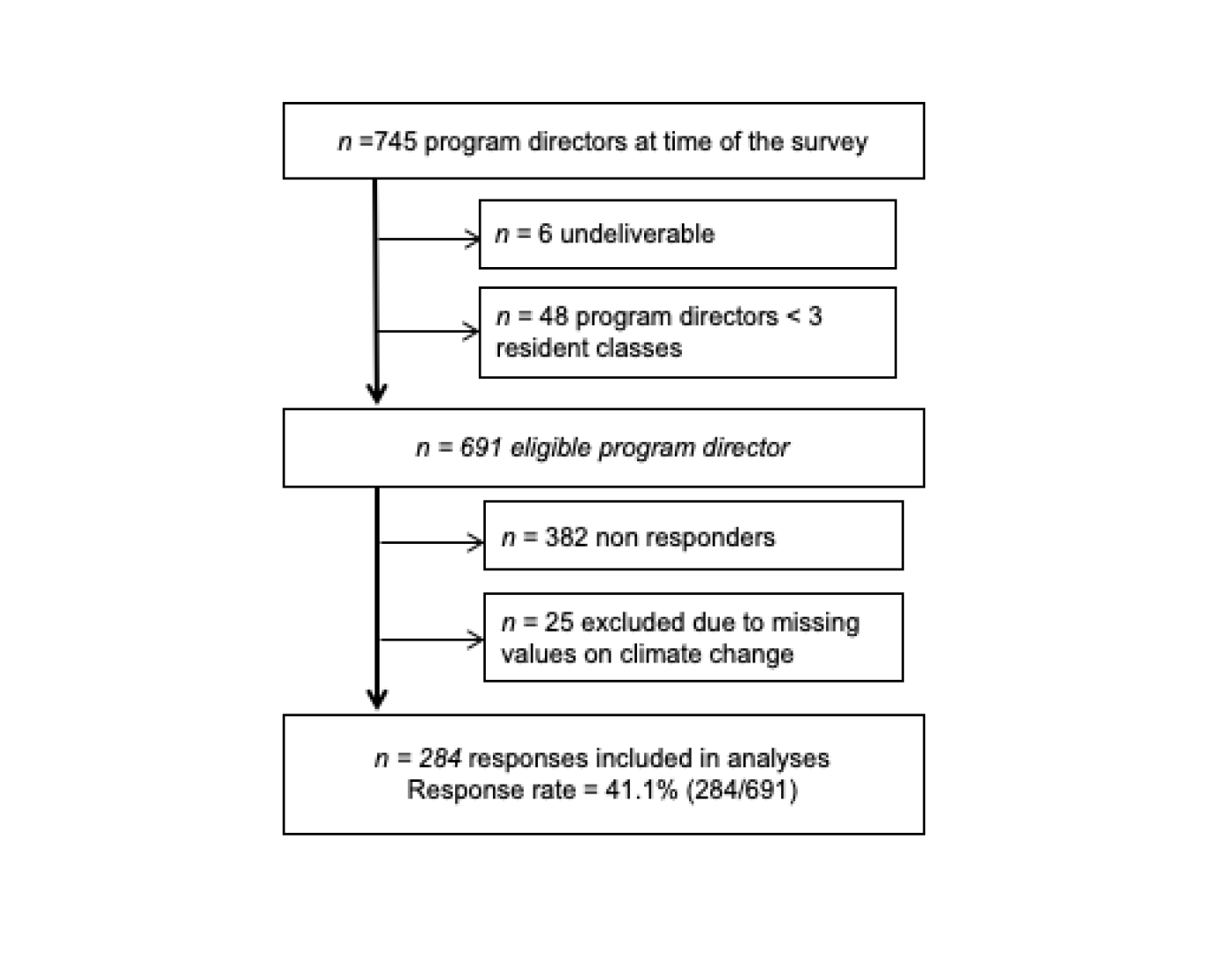
The survey invitation was sent to N=745 program directors on April 18, 2023, and three follow-up emails reminding them to participate were sent in the following weeks. The survey was terminated on May 12, 2023, and anonymized data were provided to us through CERA. The online program SurveyMonkey (Momentive Global Inc) was used to administer the survey. A priori, responses from newer residency programs (n=48) with less than three resident classes as well as undeliverable invitations (n=6) were excluded, leaving N=691 eligible program directors.
CERA also provided data on demographic characteristics of members of the Association of Family Medicine Residency Directors (AFMRD), which were used to compare with the sample of respondents.
Statistical Analyses
Anonymized data were provided to us in an Excel file. We used SPSS version 28 (IBM) to analyze data and plot figures. We used descriptive statistics (absolute and relative numbers, mean, standard deviation [SD]) to characterize the sociodemographic characteristics of respondents. To compare survey respondents’ key demographics with those of AFMRD members, we used χ2 and Fisher-Freeman-Halton tests.
We displayed the relative frequency of responses to each question in the climate-change section of the survey using stacked bar graphs. We used χ2 and Fisher-Freeman-Halton tests to assess survey responses with sociodemographic and program characteristics for independence. Previous research has linked sociodemographic factors with perception of climate change. 39 For Likert-scaled survey responses, we used Mann-Whitney U or Kruskal-Wallis tests. We assessed correlations between two Likert-scaled items with Spearman’s ρ. Significance was set at P values <.05.
This study received approval from the American Academy of Family Physicians Institutional Review Board on April 3, 2023 (#19-366, Amendment #20).
Sample
After applying exclusion criteria, we assessed 284 responses to our survey (response rate 41.1%; Figure 1).
Most respondents identified themselves as females (n=153, 54.6%) and White (n=214, 75.6%). They had an average of 6.8 years (SD 5.9 years) of experience in the program director role. Compared with program directors that were members of AFMRD (n=545), respondents did not differ regarding gender and self-perceived underrepresentation in medicine. However, White program directors were overrepresented in our sample (75.2% vs 62.2% among AFMRD members; Table 1). Similarly, community-based residency programs nonaffiliated with a university were underrepresented (P<.001).
Climate Change Beliefs, Risk Perception, and Curricula
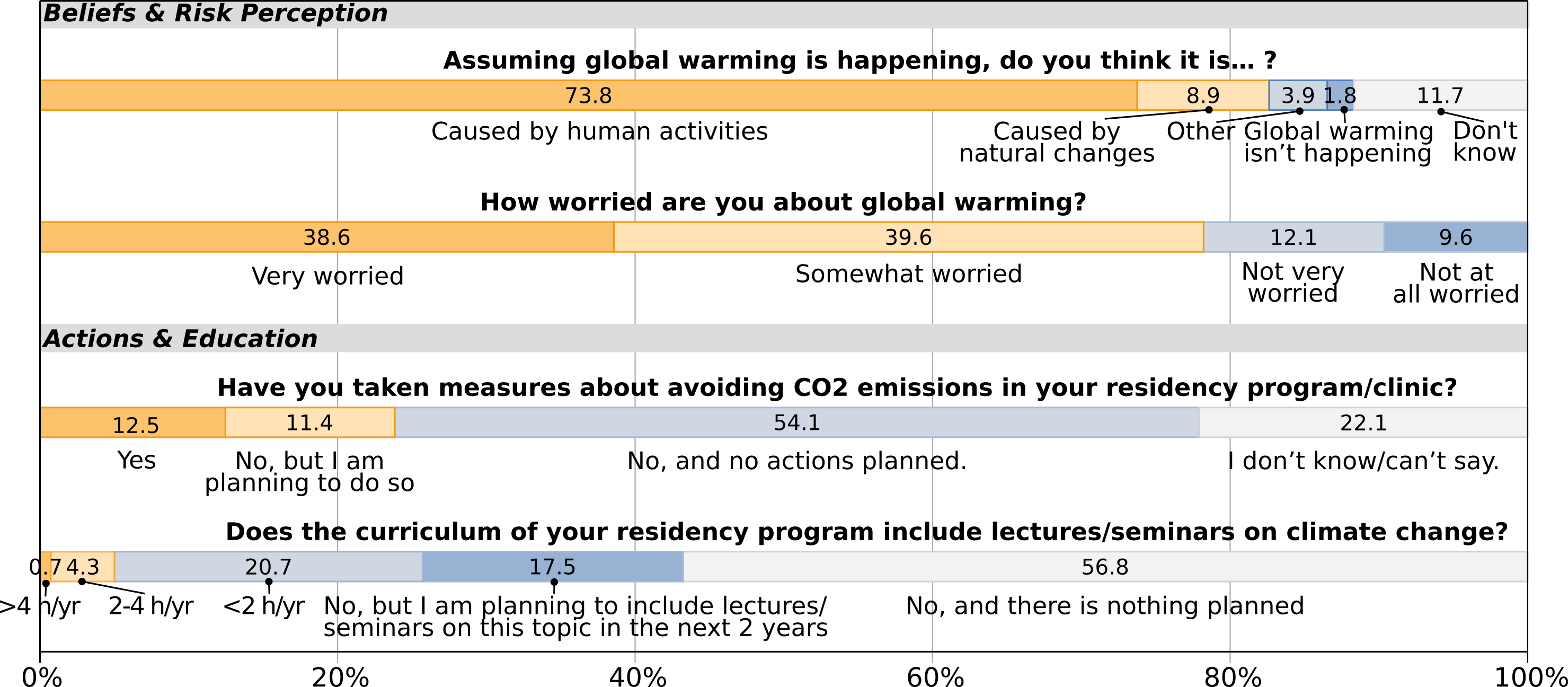
Most respondents expressed that global warming is caused by human activities (n=208, 73.8%; Figure 2). Responding program directors who did not attribute global warming to human activities (n=74, 26.2%) were more often of male gender (n=38, 30.9% vs n=31, 20.4% female; P=.002) and more frequent in East South Central (n=9, 69.2%) and West South Central states (n=15, 42.9%; P<.001) and in smaller communities with less than 30,000 inhabitants (n=15, 46.9% vs n=8, 14.3% in communities >1 million residents; P=.001). These responding program directors also had been in this position longer (mean 8.1 yrs [SD 6.4]) than those who expressed that global warming is caused by humans (mean 6.4 yrs [SD 5.6]; P=.019). Other characteristics, such as type or size of residency program or race/ethnicity of the program director, were not associated with a certain response.
Of all responding program directors, 78.2% (n=219) were either “very worried” or “somewhat worried” about global warming, with considerable differences between regions (Figure 3A). Responding program directors who did not acknowledge the human impact on global warming were much more likely to feel “not at all worried” or “not very worried” (n=51, 69.9% vs n=22, 30.1% “somewhat worried” or “very worried”; P<.001). Characteristics of gender, race/ethnicity, and years of experience as program directors, as well as size or type of residency program, were not associated with the feeling of being worried about global warming.
Only a minority (n=67, 23.9%) of responding program directors had already taken measures to avoid carbon emissions in their residency programs/clinics or were planning to apply measures. Having or planning to take measures was not associated with program directors’ sociodemographics or the type and location of the residency program. The majority of respondents (n=152, 54.1%) did not plan to take any actions. This proportion was even higher (n=51, 69.9%; P<.001) among responding program directors who did not consider mankind as a driver of global warming. Association with directors’ gender, race/ethnicity, or years of experience was not apparent.
Most programs in our survey (n=159, 56.8%) currently did not have any lectures/seminars dedicated to climate change, and the program directors did not plan to introduce such curricula. However, 17.5% (n=49) of responding program directors indicated that they planned to introduce curricula in the upcoming 2 years. A minority (n=72, 25.7%) of responding programs already taught about climate change, with most programs providing less than 2 hours per year. Responses to this question differed considerably among US states (Figure 3B; P=.018). While in New England and Pacific states only a minority of programs neither had nor planned to set up respective curricula (n=2, 25.0% and n=17, 40.5%, respectively), this proportion was particularly higher in East South Central (n=12, 92.3%) and East North Central (n=30, 69.8%) states. This proportion also was considerably higher among responding directors who doubted the impact of humans on climate change (n=60, 82.2%; P<.001) and among programs in communities with less than 30,000 inhabitants (n=24, 75.0% vs n=19, 40.4% in communities >1 million inhabitants; P=.025).
Importance of Climate Change Topics in Current Education
Most respondents considered heat-related illness and disaster preparedness as “very important” or “moderately important” (n=171, 60.6% and n=174, 62.2%, respectively). Principles of climate change (n=78, 27.8%), impact of the health care system on carbon emissions (n=81, 28.9%), and discussion of climate change related topics with patients (n=43, 15.3%) were perceived only by a minority of responding residency program directors as “very important” or “moderately important” (Figure 4 ). Those directors who did not acknowledge the impact of humans on global warming stated significantly more often that principles of climate change, impact of the health care system on carbon emissions, and discussion of climate change related topics with patients were “not important” or “slightly important” versus those who did (each P<.001). However, this was not the case for heat-related illness and disaster preparedness (P=.846 and P=.622, respectively). Furthermore, responding program directors’ worries about global warming showed strong positive correlation with perceiving the principles of climate change (r=0.51, P<.001), impact of the health care system on carbon emissions (r=0.47, P<.001), and discussion of climate change related topics with patients (r=0.38, P<.001) as important.
Barriers to Implementing Climate Change Education
Major barriers mentioned by responding program directors to implementing seminars/lectures on climate change were competing priorities (“climate change won’t directly impact my residents as much as other topics”; n=215, 36.1%), lack of available curriculum on climate change (n=161, 27.0%), and lack of knowledge/awareness by faculty (n=134, 22.5%). Less often mentioned were “negative attitudes with faculty or residents” on climate change topics (n=53, 8.9%) and other barriers (n=16, 2.7%). A minority of respondents (n=17, 6%) stated that no barriers were hindering them from introducing a climate change education curriculum. None of the barriers were significantly associated with the existence of or plan to implement a lecture/seminar on climate change in the residency program (P>.05).
Our results on climate change awareness of family medicine residency program directors are similar to those of other surveys among health care professionals, indicating that a vast majority understand that climate change is occurring, that human activity is a contributor, and that they are personally concerned about climate change for themselves and their patients. 30, 40, 41 Despite these concerns, more than half of our survey respondents had no climate change curricular content and no plans to introduce content in the near future, particularly in the East South Central states. Only a quarter of responding residency programs had dedicated lectures/seminars on climate change, and those that did frequently provided curricular content less than 2 hours per year. This finding stands contrary to material published by national medical associations 28 and the most cited medical journals, which repeatedly and jointly have stressed that global warming is a major issue to health. 42 The AMA adopted a policy affirming that climate change is occurring and that implications of climate change should be incorporated into medical education, 43 and models for integrative curricula for medical schools 44 and nursing colleges 45, 46 have been proposed. Furthermore, a general framework for climate change resident curricula has already been published 29 as well as specific curricula for pediatric residencies. 47, 48
However, 27% of program directors in our study perceived the unavailability of curricula as a barrier to implementation. Our finding, therefore, indicated a disconnect among beliefs, knowledge, and action. The data suggested that responding program directors’ current focus was on the results and direct impacts of climate change (ie, heat-related illness and disaster preparedness) rather than on the root causes of climate change. Program directors in our study were not taking a proactive role of entrusted authority in their communities to educate and raise awareness to the already existing impacts of climate change on health. The high proportion of responding program directors with climate change concerns contrasted with a significant minority of program directors who had considered how they could reduce carbon emissions at their workplace. This finding suggests that respondents were struggling to translate their personal concerns into actions. This inaction is understandable because of the lack of guidelines, evidence-based knowledge, and recommendations for action; therefore, climate change might be perceived as a difficult-to-grasp and therefore difficult-to-teach topic. In the last decade, scientific articles began to show how and where carbon emissions in the health care system occur, for example in diagnostic imaging, 49 critical care, 50 and hemodialysis; 51 still, a comprehensive repository on carbon emissions on medication, diagnostics, lab measures, and the like is still lacking. A previous survey of primary care providers regarding prescribing hypothetical medications showed that, if providers have a choice, the clear majority decide to prescribe the more climate-friendly medication. 30 This finding indicates that if practical knowledge is available, providers are likely to act. Recent articles have suggested ways that carbon emissions can be reduced in primary care, such as by considering climate and environment harmfulness in drug prescriptions; 14 these recommendations have only started to be integrated into guidelines. 52
In addition to our study revealing an overall gap between climate change concerns and actionable strategies, we observed considerable proportions of participants in certain regions questioning fundamental mechanisms of climate change. For example, we found that study participants from the East and West South Central regions, as well as those serving smaller communities, were significantly more likely to disbelieve that climate change is due to human activity. Similar regional findings have been shown among the US population. 37
Program directors’ beliefs and concerns were linked to the existence of climate change curricular content. In contrast, programs lacking such content were associated with directors doubting human impact on climate change. Notably, perceived implementation barriers were not associated with the existence of curricular content or plans to implement curricular content on climate change.
Importance of the Findings
Understanding the current state of family medicine residency curricula, program directors’ beliefs, and their plans for change is a starting point to bridging the current gap in climate change education. Program location and community size are linked to climate change perceptions and existing curricula/plans. Strategies to include climate change in curricula will need to address individual beliefs and may require regional approaches to be successful.
Strengths and Limitations
Strengths of our study were the sampling frame of all ACGME-accredited US family medicine residency programs and the relatively high response rate of 41.1% for an online survey. However, our ability to confirm the representativeness of our sample was somewhat limited. We did a basic comparison of our sample’s key characteristics with those of program directors affiliated with AFMRD. Although our survey sample closely resembled AFMRD members concerning program directors’ demographics and the location of the residency programs, our results do not represent family medicine residency programs throughout the entire United States. Program directors making the effort to return surveys may have had stronger beliefs—either positive or negative—introducing a self-selection bias. Furthermore, participants may have been prone to recall bias or satisficing. 53 We were limited to the number and type of questions in this survey (eg, no open-ended questions were allowed). This restriction prevented deeper understanding of the specific curricular content and program directors’ beliefs regarding climate change. For example, we were unable to fully assess the content of programs with global warming curricula. Furthermore, we only could determine the perceived barriers but not explore the reasons for lack of implementation more deeply.
Climate change is a pressing topic in society, politics, and the medical community; and the AMA recently has articulated the need for more climate change curricula in medical education. Despite the existence of a framework for resident curricula on climate change and the widespread personal concerns of responding program directors about climate change, more than half of the family medicine residency programs in our study did not currently teach their residents about climate change related topics and did not plan to add climate change to the curricula in the future. Similarly, they had not taken measures to reduce carbon emissions in their residency programs/clinics. Despite climate change’s implications for health and health care systems, our findings indicated that only a minority of program directors currently viewed it as a pertinent medical education topic. Without a shift in this perspective, future family medicine physicians in the United States may lack preparation for the health challenges associated with a changing climate and may not be equipped to educate patients on climate change mechanisms and their impact on health.
Acknowledgments
The authors thank the CERA team for their help and efforts in conducting this study.
References
-
-
-
Vashishtha D, Sieber W, Hailey B, Guirguis K, Gershunov A, Al-Delaimy WK. Outpatient clinic visits during heat waves: findings from a large family medicine clinical database.
Fam Pract. 2018;35(5):567-570.
doi:10.1093/fampra/cmy013
-
Alsaiqali M, De Troeyer K, Casas L, Hamdi R, Faes C, Van Pottelbergh G. The effects of heatwaves on human morbidity in primary care settings: a case-crossover study.
Int J Environ Res Public Health. 2022;19(2):832.
doi:10.3390/ijerph19020832
-
Burns PL, Aitken PJ, Raphael B. Where are general practitioners when disaster strikes?
Med J Aust. 2015;202(7):356-358.
doi:10.5694/mja14.00477
-
Burns PL, FitzGerald GJ, Hu WC, Aitken P, Douglas KA. General practitioners’ roles in disaster health management: perspectives of disaster managers. Prehosp Disaster Med. 2022;37(1):124-131. doi:10.1017/S1049023X21001230.
-
Schoenbaum M, Butler B, Kataoka S, et al. Promoting mental health recovery after hurricanes Katrina and Rita: what can be done at what cost.
Arch Gen Psychiatry. 2009;66(8):906-914.
doi:10.1001/archgenpsychiatry.2009.77
-
Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health.
PLOS ONE. 2016;11(6):e0157014.
doi:10.1371/journal.pone.0157014
-
Pichler PP, Jaccard IS, Weisz U, Weisz H. International comparison of health care carbon footprints.
Environ Res Lett. 2019;14(6):064004.
doi:10.1088/1748-9326/ab19e1
-
Eckelman MJ, Huang K, Lagasse R, Senay E, Dubrow R, Sherman JD. Health care pollution and public health damage in the United States: an update: study examines health care pollution and public health damage in the United States.
Health Aff (Millwood). 2020;39(12):2,071-2,079.
doi:10.1377/hlthaff.2020.01247
-
-
Xie E, de Barros EF, Abelsohn A, Stein AT, Haines A. Challenges and opportunities in planetary health for primary care providers.
Lancet Planet Health. 2018;2(5):e185-e187.
doi:10.1016/S2542-5196(18)30055-X
-
Fidler L, Green S, Wintemute K. Pressurized metered-dose inhalers and their impact on climate change.
CMAJ. 2022;194(12):E460.
doi:10.1503/cmaj.211747
-
Holman HT, Bouthillier MJ, Müller F. Thinking “green” when treating “pink puffers” and “blue bloaters”—reducing carbon footprint when prescribing inhalers.
J Am Board Fam Med. 2023;36(2):356-359.
doi:10.3122/jabfm.2022.220292R2
-
Devlin-Hegedus JA, McGain F, Harris RD, Sherman JD. Action guidance for addressing pollution from inhalational anaesthetics.
Anaesthesia. 2022;77(9):1,023-1,029.
doi:10.1111/anae.15785
-
White SM, Shelton CL, Gelb AW, et al; representing the World Federation of Societies of Anaesthesiologists Global Working Group on Environmental Sustainability in Anaesthesia. Principles of environmentally-sustainable anaesthesia: a global consensus statement from the World Federation of Societies of Anaesthesiologists.
Anaesthesia. 2022;77(2):201-212.
doi:10.1111/anae.15598
-
Last J, Guidotti TL. Implications for human health of global ecological changes. Public Health Rev. 1990-1991;18(1):49-67.
-
-
Bell EJ. Climate change: what competencies and which medical education and training approaches?
BMC Med Educ. 2010;10(1):31.
doi:10.1186/1472-6920-10-31
-
Gomez J, Goshua A, Pokrajac N, et al. Teaching medical students about the impacts of climate change on human health.
J Clim Change Health. 2021;3:100020.
doi:10.1016/j.joclim.2021.100020
-
Leffers J, Levy RM, Nicholas PK, Sweeney CF. Mandate for the nursing profession to address climate change through nursing education.
J Nurs Scholarsh. 2017;49(6):679-687.
doi:10.1111/jnu.12331
-
Wellbery C, Sheffield P, Timmireddy K, Sarfaty M, Teherani A, Fallar R. It’s time for medical schools to introduce climate change into their curricula.
Acad Med. 2018;93(12):1,774-1,777.
doi:10.1097/ACM.0000000000002368
-
Maxwell J, Blashki G. Teaching about climate change in medical education: an opportunity.
J Public Health Res. 2016;5(1):673.
doi:10.4081/jphr.2016.673
-
Green EIH, Blashki G, Berry HL, Harley D, Horton G, Hall G. Preparing Australian medical students for climate change. Aust Fam Physician. 2009;38(9):726-729.
-
Müller L, Kühl M, Kühl SJ. Climate change and health: Changes in student environmental knowledge and awareness due to the implementation of a mandatory elective at the Medical Faculty of Ulm?
GMS J Med Educ. 2023;40(3):Doc32.
doi:10.3205/ZMA001614
-
Nordrum OL, Kirk A, Lee SA, et al. Planetary health education in medical curricula in the Republic of Ireland.
Med Teach. 2022;44(11):1237-1243.
doi:10.1080/0142159X.2022.2072279
-
Bevan J, Blyth R, Russell B, et al. Planetary health and sustainability teaching in UK medical education: A review of medical school curricula.
Med Teach. 2023;45(6):623-632.
doi:10.1080/0142159X.2022.2152190
-
-
Philipsborn RP, Sheffield P, White A, Osta A, Anderson MS, Bernstein A. Climate change and the practice of medicine: essentials for resident education.
Acad Med. 2021;96(3):355-367.
doi:10.1097/ACM.0000000000003719
-
Müller F, Skok JI, Arnetz JE, Bouthillier MJ, Holman HT. Primary care clinicians’ attitude, knowledge, and willingness to address climate change in shared decision-making.
J Am Board Fam Med. 2023;jabfm.2023.230027R1.
doi:10.3122/jabfm.2023.230027R1
-
Xu R, Yu P, Abramson MJ, et al. Wildfires, global climate change, and human health.
N Engl J Med. 2020;383(22):2,173-2,181.
doi:10.1056/NEJMsr2028985
-
-
Rocque RJ, Beaudoin C, Ndjaboue R, et al. Health effects of climate change: an overview of systematic reviews.
BMJ Open. 2021;11(6):e046333.
doi:10.1136/bmjopen-2020-046333
-
Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research.
Ann Fam Med. 2018;16(3):257-260.
doi:10.1370/afm.2228
-
Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A consensus-based Checklist for Reporting of Survey Studies (CROSS).
J Gen Intern Med. 2021;36(10):3,179-3,187.
doi:10.1007/s11606-021-06737-1
-
-
Howe PD, Mildenberger M, Marlon JR, Leiserowitz A. Geographic variation in opinions on climate change at state and local scales in the USA.
Nature Clim Change. 2015;5(6):596-603.
doi:10.1038/nclimate2583
-
-
McCright AM, Dunlap RE. Cool dudes: the denial of climate change among conservative White males in the United States.
Glob Environ Change. 2011;21(4):1,163-1,172.
doi:10.1016/j.gloenvcha.2011.06.003
-
Kotcher J, Maibach E, Miller J, et al. Views of health professionals on climate change and health: a multinational survey study.
Lancet Planet Health. 2021;5(5):e316-e323.
doi:10.1016/S2542-5196(21)00053-X
-
Boland TM, Temte JL. Family medicine patient and physician attitudes toward climate change and health in Wisconsin.
Wilderness Environ Med. 2019;30(4):386-393.
doi:10.1016/j.wem.2019.08.005
-
Atwoli L, Baqui AH, Benfield T, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health.
N Engl J Med. 2021;385(12):1,134-1,137.
doi:10.1056/NEJMe2113200
-
-
Sullivan JK, Lowe KE, Gordon IO, et al. Climate Change and medical education: an integrative model.
Acad Med. 2022;97(2):188-192.
doi:10.1097/ACM.0000000000004376
-
-
Quinn Griffin MT, Alfes CM, Chavez F, et al. Incorporating climate change into doctor of nursing practice curricula.
J Prof Nurs. 2022;42:156-161.
doi:10.1016/j.profnurs.2022.06.008
-
Gauthier SJ. Changing degrees: incorporating the impacts of climate change on health into pediatric residency education and practice.
Yale J Biol Med. 2023;96(2):227-232.
doi:10.59249/BSGY1262
-
Goshua A, Gomez J, Erny B, et al. Child-focused climate change and health content in medical schools and pediatric residencies.
Pediatr Res. 2023.
doi:10.1038/s41390-023-02600-7
-
McAlister S, McGain F, Petersen M, et al. The carbon footprint of hospital diagnostic imaging in Australia.
Lancet Reg Health West Pac. 2022;24:100459.
doi:10.1016/j.lanwpc.2022.100459
-
Pollard AS, Paddle JJ, Taylor TJ, Tillyard A. The carbon footprint of acute care: how energy intensive is critical care?
Public Health. 2014;128(9):771-776.
doi:10.1016/j.puhe.2014.06.015
-
Lim AEK, Perkins A, Agar JWM. The carbon footprint of an Australian satellite haemodialysis unit.
Aust Health Rev. 2013;37(3):369-374.
doi:10.1071/AH13022
-
-





There are no comments for this article.