Background and Objectives: Physician demographics in North America do not yet reflect the diversity of the communities they serve, accounted to systemic barriers targeting underrepresented in medicine (URiM) groups. URiM medical graduates are more likely to pursue generalist specialties, including family medicine. Mini Med Schools (MMSs) are pathway programs intended to motivate URiM youth to pursue medicine. A gap in literature exists regarding the potential of MMSs to provide youth with useful information. We examined the extent to which youth reported a change in knowledge about medicine as a career before and after attending an MMS.
Methods: Asclepius Medical Camp for Youth is a weeklong MMS for high school students, held at one Canadian university. In 2022, 50 youth participants were invited to complete surveys and quizzes measuring their knowledge about pursuing a career in medicine.
Results: The mean self-reported knowledge differed significantly precamp (n=34, M=5.87/10, SD=1.9) versus postcamp (n=26, M=8.28/10, SD=1.4; t[35]=7.07, P<.05). Likewise, participants’ scores demonstrated a significant difference in mean scores precamp (n=43, M=7.12, SD=2.39) versus postcamp (n=39, M=9.31, SD=1.13; t[42]=5.08, P<.05).
Conclusions: These findings highlight MMSs as a promising strategy to provide knowledge about medical careers beyond instilling motivation. By both inspiring and informing URiM youth, the long-term outcome of diversifying medicine may be achieved.
Physician demographics are not yet representative of the patient populations they serve. Underrepresented in medicine (URiM) populations include low socioeconomic status (SES), rural, Indigenous, Black, and Hispanic.1, 2 Persistent systemic barriers limit equity in medical school admissions.3 In addition to high costs associated with a successful application,4 lack of knowledge about preparing to apply to medical school may likewise contribute.
Optimizing diversity benefits physicians and patients through several mechanisms. For example, Saha et al found that White medical students in a diverse medical student body reported increased confidence in cultural competency and motivation to provide equitable care.5 Furthermore, URiM physicians are more likely to become generalist practitioners and serve diverse patient populations.6, 7 Dowell et al found that physicians from rural upbringings were more likely to practice in rural settings;8 similarly, Komaromy et al identified that Black physicians cared for more Black patients than other physicians.6 In a systematic review, Gomez and Bernet revealed that patient health outcomes were superior with diverse health care teams. 9
Diversifying medicine must start with medical school admissions. Strategies to address systemic barriers include free initiatives for Medical College Admission Test (MCAT) instruction, mentorship, and interview preparation.3, 10 Another strategy is the implementation of Mini Med Schools (MMSs). These are pathway programs that invite URiM youth to learn about careers in medicine through hands-on activities and interactions with medical students. These programs are especially important for high school youth as they begin to consider career options. 10, 11
Existing MMS studies primarily have used qualitative methods to examine students’ interest in medicine pre- versus postattendance, establishing that MMSs are effective in inspiring youth to pursue medicine.11, 12 Motivation alone, however, does not fully address the underlying barriers facing URiM youth. In this study, we examined the extent to which one MMS resulted in changes in knowledge about the training required to pursue a career in medicine.
Asclepius Medical Camp for Youth
Established in 2009, Asclepius Medical Camp for Youth is a free weeklong summer camp MMS organized by medical student volunteers at the University of Alberta in Edmonton, Alberta, Canada. High school students engage in clinical skills and networking with medical students (supplemental material). Students from low SES backgrounds are prioritized to attend Asclepius, followed by other URiM youth. Fifty URiM students attended Asclepius in 2022.
Providing Knowledge and Tools for Success
The camp programming included two practical information sessions and two discussion panels with medical students. Furthermore, participants received a gift bag that included brochures from health care profession training programs, scholarship information, contacts for medical students offering ongoing mentorship, and a free local MCAT and interview preparation program.
Evaluation of Changes in Knowledge
We measured camp participants’ knowledge about pursuing medicine before and after the camp. We used two different measures: a self-report online survey and an objective verbal quiz. The survey asked participants to rate their knowledge about the field of medicine and the process of applying to medical school. The verbal quiz (Table 1) tested the participants’ knowledge of the process of becoming a physician. The quiz was administered by volunteers who were trained as a group to minimize interrater differences. We used paired-sample t tests to compare (a) change in score on objective quiz and self-report precamp to postcamp, (b) precamp knowledge score in the two conditions (objective quiz versus self-report), and (c) postcamp knowledge score in the two conditions. We collected and managed study data using REDCap (REDCap Consortium) electronic data capture tools hosted by the Women & Children’s Health Research Institute at the University of Alberta.13 This study was reviewed and approved by the Research Ethics Board at the University of Alberta (Pro00118041). Informed consent was obtained from all study participants.
|
Question
|
Correct answer
|
|
Test prior to medical school?
|
Yes, the MCAT
|
|
After high school?
|
Undergraduate/bachelor’s degree
|
|
Which undergraduate major is acceptable?
|
Any major is acceptable
|
|
Years to complete an undergraduate degree?
|
4 years
|
|
Do medical school applications include extracurriculars?
|
Yes
|
|
Years to complete medical school?
|
4 years
|
|
After medical school?
|
Residency training
|
|
List 3 types of physicians.
|
Many correct answers
|
|
List 3 types of nonphysician health care professionals.
|
Many correct answers
|
The response rate was 68% (34/50 students) for the precamp survey and 52% for the postcamp survey (26/50 students). Pairwise t tests demonstrated that students’ mean self-reported knowledge scores differed significantly precamp (M=5.87/10, SD=1.9) versus postcamp (M=8.28/10, SD=1.4); t[35]=7.07, P<.05). For the objective verbal quiz, the response rate was 86% (43/50 students) for the precamp quiz and 78% (39/50 students) for the postcamp quiz. We identified a significant difference in mean quiz scores precamp (M=7.12, SD=2.39) and postcamp (M=9.31, SD=1.13; t[42]=5.08, P<.05). We also noted a significant difference between self-report and objective verbal quiz scores postcamp (self-report M=8.28, SD=1.4; quiz score M=9.31, SD=1.13, t[27]=3.3, P<.05), but not precamp.
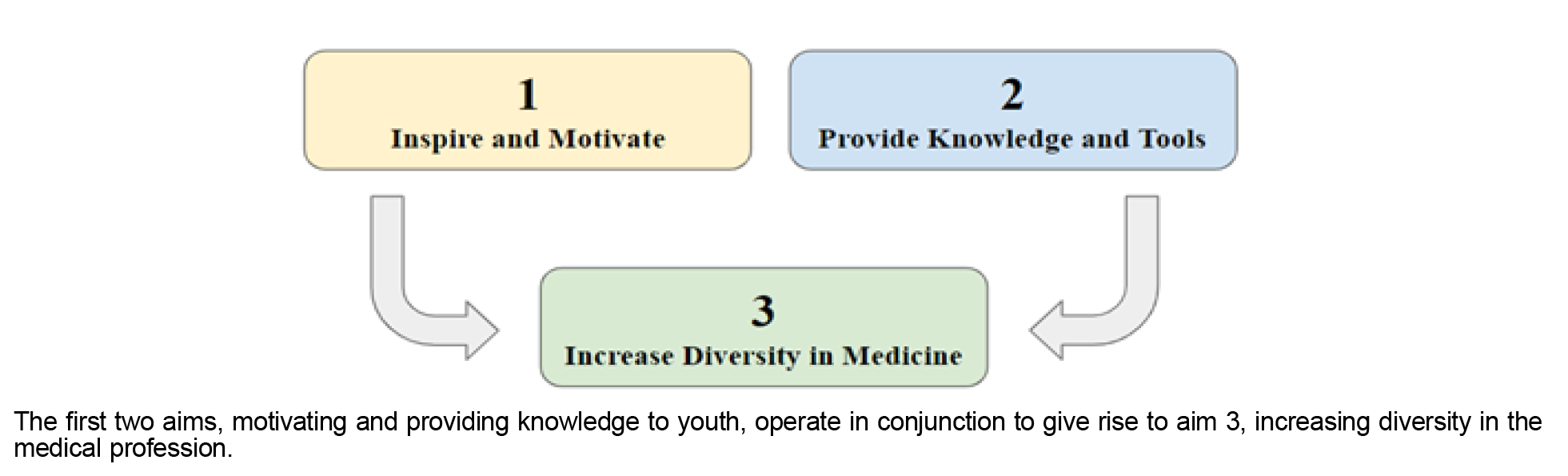
We propose three aims of MMSs (Figure 1):
-
Inspiring and motivating youth to choose medicine as their dream career
-
Providing knowledge and tools for success to pursue a career in medicine
-
Increasing diversity in medical school matriculation demographics
The first two aims work in concert to manifest the ultimate third aim of diversifying the medical profession.
The first two aims, motivating and providing knowledge to youth, operate in conjunction to give rise to aim 3, increasing diversity in the medical profession.
Existing MMS literature supports the conclusion that MMSs carry the potential to achieve aim 1 in encouraging youth to consider a career as a physician.11, 12 The 2022 Asclepius data further established that MMSs can additionally objectively increase students’ knowledge about how to pursue this career pathway to realize their aspirations, fulfilling aim 2 of MMSs. Taken together, youth attending MMSs may be both inspired and informed about pursuing a career in medicine, thereby improving diversity in medicine as the long-term outcome of aim 3.
One practical implication of the three proposed aims is that the target youth population for a given MMS ought to match the aim of the MMS. To illustrate, the Asclepius camp has an application process that results in camp attendees who often already are interested in medicine prior to attending the camp. While the camp has proven to be effective in increasing knowledge for these participants (aim 2), we will need to consider a different recruitment approach to achieve aim 1. Conversely, for MMSs that invite youth without a prior demonstrated interest in medicine (such as a general high school class), the programming ought to focus on achieving aim 1 by piquing the interests of students. Both styles of MMSs fill an equally important niche as pathway programs.
To further investigate this difference in target population affecting a program’s prioritization of aim 1 versus aim 2, we are piloting separate single-day Asclepius events, inviting youth without preexisting interest in medicine to engage in similar activities, measuring their knowledge and interest outcomes.
As a limitation, MMSs cannot address all barriers of URiM youth as prospective applicants for careers in medicine. Youth from low SES backgrounds, for example, may face difficulty in attending this camp due to the necessity of maintaining summer employment. Rural students may face difficulty in accessing Asclepius due to the camp being held at an urban center. To address this barrier, we are piloting shorter Asclepius events to accommodate summer job demands as well as events in rural locations for rural youth.
Another notable limitation concerns aim 3 due to the lack of longitudinal data for MMSs. In response, we recently have added an element to our Asclepius surveys, which will enable future follow-up on participants’ educational and career outcomes.
We conclude that Mini Med Schools offer the potential to increase knowledge by bolstering URiM youth with tools for success in their pursuit of a career in medicine. In this way, Mini Med Schools may provide one strategy among multifaceted approaches that are required to diversify the medical profession, improving both patient and provider outcomes.
Presentations
A portion of this data was presented at the 2023 International Congress of Academic Medicine in Québec City, Québec, Canada, in April 2023.
Acknowledgments
- Kai Fan, Asha Bansal, and Julia Craig for organizing Asclepius Medical Camp for Youth 2022 as camp coordinators alongside the authors.
- Sam Shang, Dr Ronan Noble, Dr Vienna Buchholz, Dr Jordan Herst, Dr Vaishvi Patel, Dr Sydney Inthof, and Dr Abbey Pagée for volunteering as camp counselors and administering quizzes at Asclepius Medical Camp for Youth 2022.
- All physicians, health care learners and professionals, and donors for their contributions toward Asclepius Medical Camp for Youth, including the 2021 senior camp coordinators: Dr Cassandra Walmsley, Dr Jonas Szelewicki, and Dr Jamie Grunwald.
- The University of Alberta Medical Students’ Association for allocating budget toward the annual Asclepius Medical Camp for Youth initiative.
- Chris Donoff for statistical analyses.
Author Contributions
- K.P., A.K., and S.L. organized the 2022 Asclepius Medical Camp for Youth as senior coordinators and served as junior coordinators for the 2021 camp.
- K.P., A.K., S.L., and S.R. conceptualized the study design and methods, and were involved in project development and execution.
References
-
Khan R, Apramian T, Kang JH, Gustafson J, Sibbald S. Demographic and socioeconomic characteristics of Canadian medical students: a cross-sectional study.
BMC Med Educ. 2020;20(1):151.
doi:10.1186/s12909-020-02056-x
-
-
Michalec B, Hafferty FW. Examining the U.S. premed path as an example of discriminatory design & exploring the role(s) of capital.
Soc Theory Health. 2023;21:70-97. Accessed January 22, 2023.
doi:10.1057/s41285-022-00175-7
-
Pitre T, Thomas A, Evans K, Jones A, Mountjoy M, Costa AP. The influence of income on medical school admissions in Canada: a retrospective cohort study.
BMC Med Educ. 2020;20(1):209.
doi:10.1186/s12909-020-02126-0
-
Saha S, Guiton G, Wimmers PF, Wilkerson L. Student body racial and ethnic composition and diversity-related outcomes in US medical schools.
JAMA. 2008;300(10):1,135-1,145.
doi:10.1001/jama.300.10.1135
-
Komaromy M, Grumbach K, Drake M, et al. The role of Black and Hispanic physicians in providing health care for underserved populations.
N Engl J Med. 1996;334(20):1,305-1,310.
doi:10.1056/NEJM199605163342006
-
Lupton K, Vercammen-Grandjean C, Forkin J, Wilson E, Grumbach K. Specialty choice and practice location of physician alumni of University of California premedical postbaccalaureate programs.
Acad Med. 2012;87(1):115-120.
doi:10.1097/ACM.0b013e31823a907f
-
Dowell J, Norbury M, Steven K, Guthrie B. Widening access to medicine may improve general practitioner recruitment in deprived and rural communities: survey of GP origins and current place of work.
BMC Med Educ. 2015;15:165.
doi:10.1186/s12909-015-0445-8
-
-
Parsons M, Caldwell MT, Alvarez A, et al. Physician pipeline and pathway programs: an evidence-based guide to best practices for diversity, equity, and inclusion from the Council of Residency Directors in Emergency Medicine.
West J Emerg Med. 2022;23(4):514-524.
doi:10.5811/westjem.2022.2.54875
-
Henderson RI, Williams K, Crowshoe L. Mini-med school for Aboriginal youth: experiential science outreach to tackle systemic barriers.
Med Educ Online. 2015;20(1):1-7. Accessed August 7, 2023.
doi:10.3402/meo.v20.29561
-
Rosser JC Jr, Legare TB, Jacobs C, Choi KM, Fleming JP, Nakagiri J. SAGES Mini Med School: inspiring high school students through exposure to the field of surgery.
Surg Endosc. 2018;32:4,235-4,243.
doi:10.1007/s00464-018-6171-7
-
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support.
J Biomed Inform. 2009;42(2):377-381.
doi:10.1016/j.jbi.2008.08.010



There are no comments for this article.