Background and Objectives: International medical graduates (IMGs) are a quarter of US practicing physicians and residents, with higher numbers in family medicine. Our objective was to determine whether the progression of milestone ratings varies between IMGs and US medical graduates based on a residency’s historical percentage of IMGs.
Methods: Data, which were all from the American Board of Family Medicine, included milestone ratings of each family medicine graduate from 2018 to 2020. We calculated the mean milestone rating for each core competency at each assessment. The main exposure was the 10-year percentage of residency graduates who were IMGs: very low (<10%), low (10%–33%), medium (34%–66%), and high (67%–100%). We used repeated measures multilevel regression to test for adjusted associations of resident and residency characteristics with milestone performance. Interactions between IMG status and historical percentage of IMGs tested for differential milestone growth.
Results: Our sample included 12,302 residents from 538 residencies. Of the family medicine residencies, 41.8% had less than 10% IMGs. Across milestones, mean growth between rating periods ranged from 0.46 to 0.54. In adjusted regression analysis, both being an IMG (β=–0.003 to –0.07) and training in a higher historical IMG residency (β=–0.01 to –0.08) were associated with lower milestone ratings. IMGs in high IMG programs had higher ratings for medical knowledge and professionalism (β=0.07).
Conclusions: We found comparable milestone ratings between IMGs and US medical graduates, with IMGs getting a small boost if they were trained in a program with a higher percentage of IMGs. Our results demonstrate that the performance of IMGs may be enhanced in residencies with a history of acculturating them.
International medical graduates (IMGs) account for approximately 25% of all currently practicing physicians in the United States. 1 IMGs are increasing their presence in the US workforce; they were 9,045 of 35,984 (25.1%) of incoming resident physicians matched in 2024. IMGs are increasingly matching in family medicine residencies with 31.6% of positions filled by IMGs in 2024. 2 In the last 10 years, the total number of family medicine residency positions has increased from 2,940 in 2003 to 5,213 in 2024; concomitantly, a slow rise is happening in the percentage of IMGs matching to family medicine residencies. 3, 4
IMGs face a unique set of challenges during their residency training. 5-10 While adjusting to a new country, IMGs also must adapt to a new medical culture in the United States, which is often different from their country of origin. 11 IMGs struggle with language barriers, social isolation, and overall understanding of the health care system in a foreign country. 12 A study comparing US medical graduates (USMGs) to IMGs showed significant deficiencies at multiple skill levels in IMGs at the beginning of residency training. 13 Studies also have shown that IMGs are more resilient and less inclined to burnout during residency training, 14-16 but providing a supportive environment for their personal and professional growth is crucial. Intuitively, IMGs may have an easier time adjusting to the US health care system in residencies with experience training a greater number of IMGs.
The Accreditation Council for Graduate Medical Education (ACGME) milestones provide a framework to assess professional development of individual residents in the form of six core competencies: (a) patient care, (b) medical knowledge, (c) systems-based practice, (d) practice-based learning and improvement, (e) professionalism, and (f) interpersonal and communication skills. Many of these assess how the resident functions in the health care system. In family medicine, 22 specific subcompetencies are listed within or under the six core competencies. The competencies are assessed and scored by each residency program from zero (not yet completed level 1) to five (resident/fellow expert), with a four being the goal at time of graduation. 17 The milestone reporting system is a reliable way to track individual resident progress. 18 Multiple studies have compared the effect of race, gender, and ethnicity with milestone progression. 19-22 Data are lacking when comparing IMG and USMG progression on milestone ratings. Therefore, our objective was to determine whether progression on the milestones varies among IMGs and USMGs based on their residency’s historical percentage of IMGs. Our hypothesis was that IMGs will have a more standard progression on nonmedical knowledge milestones in residencies with higher historical percentages of IMGs.
Our sample included three cohorts of family medicine residents in ACGME-accredited residency programs who graduated from 2018 to 2020. We excluded residents in 4-year or combined programs and those who transferred programs and included residents who completed training in 36 months. The American Board of Family Medicine (ABFM) receives milestone ratings from ACGME, which are assigned by the programs. Residents’ demographic information, including site of medical school training and site of residency training program, was obtained from the ABFM administrative database. Postgraduate year 1 (PGY-1) in-training examination (ITE) scores were obtained from the ABFM administrative database. Race and ethnicity were self-reported by the residents when they registered for the ABFM initial certification examination.
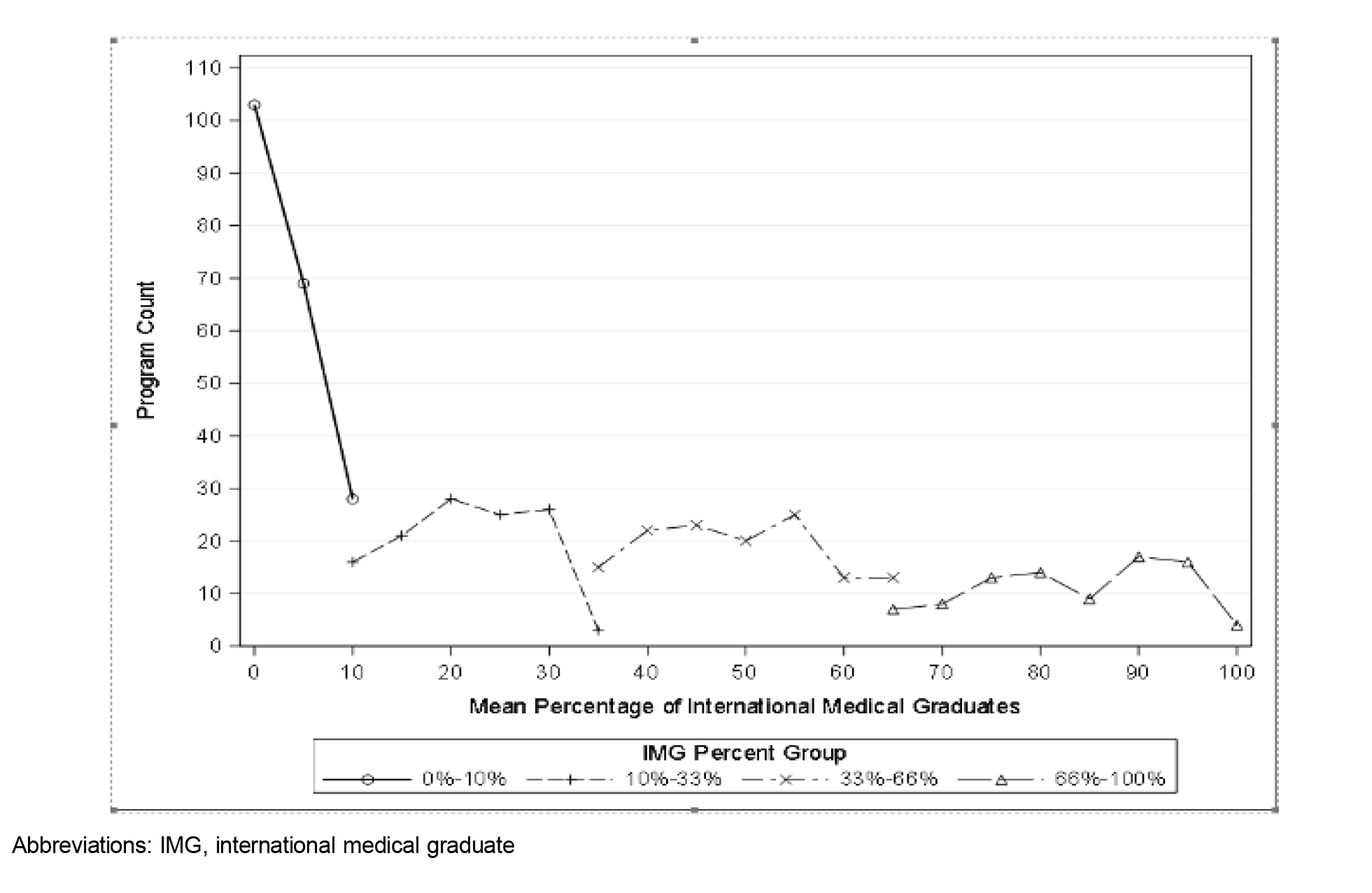
To create our outcome measure for each resident at each measurement period, we calculated the mean milestone rating in a core competency by averaging all the specific milestone scores (patient care 1, patient care 2, etc) in that competency. To create our exposure variable, we calculated the percentage of residency graduates in ABFM data who were IMGs from 2013 to 2023. We used the percentage to create categories to reflect very low (<10%), low (10%–33%), medium (34%–66%), and high (67%–100%) historical IMG presence in the residency. While residencies exist that never had an IMG graduate, the test for interaction between being an IMG and being in a 0% IMG residency is impossible, hence the need for the less than 10% category.
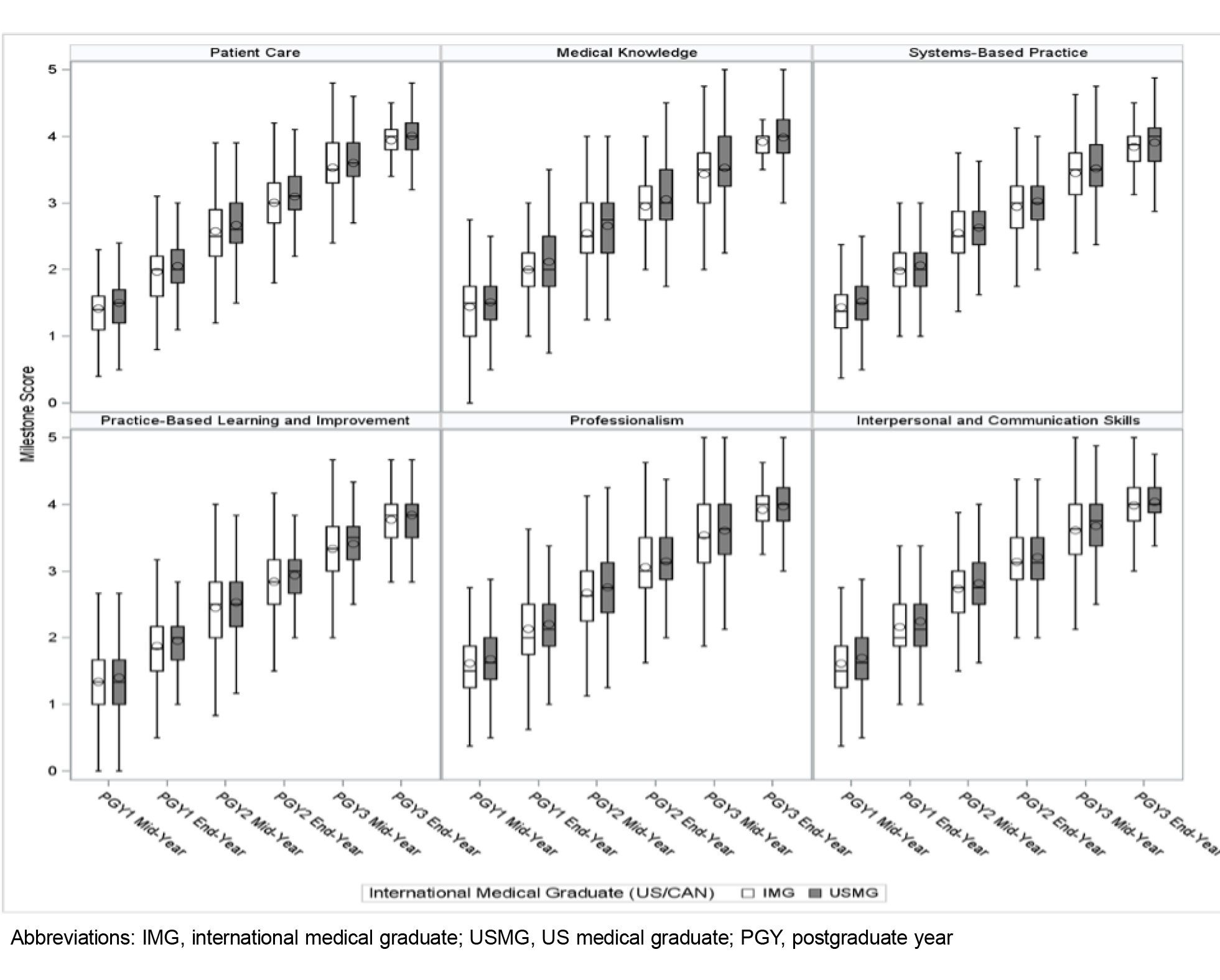
We first performed descriptive analysis of our data. We then performed bivariate testing of variables by historical residency IMG percentage. We used a false discovery rate adjusted P value to account for multiple testing. We plotted the mean milestone score over time for each competency by IMG versus USMG status.
Finally, we performed a repeated measures multilevel regression to test for adjusted associations of resident and residency characteristics associated with milestone performance in each competency. Each model controlled for resident characteristics (age, gender, degree type, race, and ethnicity) and baseline medical knowledge via PGY-1 ITE score. We included interactions between IMG status and historical percentage of IMGs to test for whether IMGs in programs with a higher percentage of IMGs had differential growth in milestone ratings. Multicollinearity of variables was assessed during model building. SAS version 9.4 (SAS Institute) was used for all analyses. This study was approved by the American Academy of Family Physicians Institutional Review Board.
Our analytic sample included 12,302 residency graduates of 538 residencies from 2018 to 2020. Most residents trained in residencies with a low historical percentage of IMGs, with 5,066 (41.8%) in less than 10% and 2,577 (20.9%) in 10% to 33% (Table 1). Only 14.2% of residents trained in a residency with a high historical percentage of IMGs. Of note, 13% of programs had no IMG graduates from 2013 to 2023 (Figure 1). Not surprisingly, resident characteristics differed by program historical IMG status. Resident-specific characteristics associated with higher IMG percentage groups were older age, male gender, Hispanic ethnicity, origin in Asian countries, and lower ITE score. The percentage of residents who are female decreased with the percentage of IMGs, with 55.7% being female in the lowest historical percentage of IMGs group going down to 50.1% in the highest historical percentage of IMGs group. Based on historical IMG percentage, we found statistically significant but small differences in mean milestone assessment for all six milestones; the average rating varied by only 0.03 between groups (Table 1). Similarly, we found no difference in growth pattern when comparing IMG versus USMG residents in the overall progression of milestones (Figure 2).
|
|
Historical Percentage of IMGs in the
Residencies
|
|
|
0%–10%
|
10%–33%
|
34%–66%
|
67%–100%
|
All
|
|
Total
|
5,066
|
2,577
|
2,910
|
1,749
|
12,302
|
|
Age (in years), n (%)
|
<35
|
4,408 (87.0)
|
2,115 (82.1)
|
2,258 (77.6)
|
1,224 (70.0)
|
10,005 (81.3)*
|
|
≥35
|
658 (13.0)
|
462 (17.9)
|
652 (22.4)
|
525 (30.0)
|
2,297 (18.7)
|
|
Gender, n (%)
|
Female
|
2,820 (55.7)
|
1,331 (51.6)
|
1,463 (50.3)
|
876 (50.1)
|
6,490 (52.8)*
|
|
Male
|
2,229 (44.0)
|
1,244 (48.3)
|
1,446 (49.7)
|
873 (49.9)
|
5,792 (47.1)
|
|
Nonbinary
|
13 (0.3)
|
1 (0)
|
|
|
14 (0.1)
|
|
Prefer not to answer
|
3 (0.1)
|
1 (0)
|
1 (0)
|
|
5 (0)
|
|
Prefer to self-describe
|
1 (0)
|
|
|
|
1 (0)
|
|
Degree type, n (%)
|
DO
|
1,348 (26.6)
|
755 (29.3)
|
467 (16.0)
|
76 (4.3)
|
2,646 (21.5)*
|
|
MD
|
3,718 (73.4)
|
1,822 (70.7)
|
2,443 (84.0)
|
1,673 (95.7)
|
9,656 (78.5)
|
|
Site of training, n (%)
|
IMG
|
141 (2.8)
|
622 (24.1)
|
1,622 (55.7)
|
1,488 (85.1)
|
3,873 (31.5)*
|
|
US/CAN
|
4,925 (97.2)
|
1,955 (75.9)
|
1,288 (44.3)
|
261 (14.9)
|
8,429 (68.5)
|
|
Race, n (%)
|
American Indian or Alaska Native
|
43 (0.8)
|
12 (0.5)
|
17 (0.6)
|
14 (0.8)
|
86 (0.7)*
|
|
Asian
|
774 (15.3)
|
519 (20.1)
|
797 (27.4)
|
650 (37.2)
|
2,740 (22.3)
|
|
Black or African American
|
275 (5.4)
|
177 (6.9)
|
301 (10.3)
|
172 (9.8)
|
925 (7.5)
|
|
Native Hawaiian or Other Pacific Islander
|
12 (0.2)
|
11 (0.4)
|
14(0.5)
|
3 (0.2)
|
40 (0.3)
|
|
Other
|
280 (5.5)
|
176 (6.8)
|
289 (9.9)
|
240 (13.7)
|
985 (8.0)
|
|
White
|
3,682 (72.7)
|
1,682 (65.3)
|
1,492 (51.3)
|
670 (38.3)
|
7,526 (61.2)
|
|
Ethnicity, n (%)
|
Hispanic or Latino
|
402 (7.9)
|
217 (8.4)
|
277 (9.5)
|
244 (14.0)
|
1,140 (9.3)*
|
|
Non-Hispanic
|
4,664 (92.1)
|
2,360 (91.6)
|
2,633 (90.5)
|
1,505 (86.0)
|
11,162 (90.7)
|
|
PGY-1 ITE score, Mean (SD)
|
|
397.82 (74.89)
|
373.89 (72.13)
|
361.09 (72.60)
|
349.42 (70.41)
|
377.14 (75.48)*
|
|
Mean change in mean milestone rating between assessments, Mean (SD)
|
PC
|
0.50 (0.11)
|
0.50 (0.12)
|
0.49 (0.14)
|
0.49 (0.17)
|
0.50 (0.13)*
|
|
MK
|
0.51 (0.13)
|
0.50 (0.14)
|
0.49 (0.15)
|
0.49 (0.19)
|
0.50 (0.15)*
|
|
SBP
|
0.53 (0.13)
|
0.53 (0.14)
|
0.52 (0.16)
|
0.51 (0.18)
|
0.52 (0.15)*
|
|
PBLI
|
0.48 (0.13)
|
0.47 (0.13)
|
0.46 (0.15)
|
0.46 (0.18)
|
0.47 (0.14)*
|
|
Prof.
|
0.53 (0.18)
|
0.53 (0.21)
|
0.53 (0.45)
|
0.51 (0.24)
|
0.53 (0.28)
|
|
ICS
|
0.54 (0.17)
|
0.54 (0.17)
|
0.52 (0.34)
|
0.51 (0.18)
|
0.53 (0.22)*
|
In adjusted regression analyses for each milestone (Table 2), we found that residents in a higher historical percentage of IMGs residency tended to have lower but statistically nonsignificant milestone ratings. The exception was for professionalism and interpersonal and communication skills in residencies with 34% to 66% IMGs having significantly lower ratings (–0.10130 and –0.08733, respectively). Testing for interactions between being an IMG and the historical percentage of IMGs, associations were positive and generally increased with a higher percentage of IMGs. For example, in medical knowledge, IMGs in a residency with 10% to 33% IMGs would expect an increase in milestone rating of 0.01826, which increases to 0.02910 in 34% to 66%, and 0.70630 in 67% to 100%. However, the magnitudes were small and only two interactions—being an IMG in a residency with 67%–100% IMGs for professionalism and medical knowledge—were statistically significant.
|
|
Estimate
|
|
Effect
|
PC
|
MK
|
SBP
|
PBLI
|
Prof.
|
ICS
|
|
Intercept
|
2.9000
|
2.7136
|
2.8356
|
2.7421
|
2.9135
|
3.0471
|
|
Residency characteristics
|
|
Historical IMG percentage
|
0%–10%
|
0
|
0
|
0
|
0
|
0
|
0
|
|
10%–33%
|
0.02387
|
0.03861
|
0.01624
|
0.01505
|
0.00626
|
0.01853
|
|
34%–66%
|
–0.05878
|
–0.02584
|
–0.04486
|
–0.05863
|
–0.10130*
|
–0.08733*
|
|
67%–100%
|
–0.01011
|
0.00501
|
–0.02949
|
–0.03398
|
–0.07466
|
–0.02658
|
|
Interaction of IMG and historical IMG percentage
|
0%–10% × IMG
|
0
|
0
|
0
|
0
|
0
|
0
|
|
|
0%–10% × USMG
|
0
|
0
|
0
|
0
|
0
|
0
|
|
|
10%–33% × IMG
|
0.01169
|
0.01826
|
0.02929
|
0.03059
|
0.01283
|
0.00839
|
|
|
10%–33% × USMG
|
0
|
0
|
0
|
0
|
0
|
0
|
|
|
34%–66% × IMG
|
0.01572
|
0.02910
|
0.02656
|
0.02810
|
0.02880
|
0.01137
|
|
|
34%–66% × USMG
|
0
|
0
|
0
|
0
|
0
|
0
|
|
|
67%–100% × IMG
|
0.03530
|
0.07063*
|
0.04258
|
0.04923
|
0.07516*
|
0.05183
|
|
|
67%–100% × USMG
|
0
|
0
|
0
|
0
|
0
|
0
|
|
Resident characteristics
|
|
Gender
|
Female
|
0.03017*
|
0.01633*
|
0.02438*
|
–0.00586
|
0.03613*
|
0.02548*
|
|
Male
|
0
|
0
|
0
|
0
|
0
|
0
|
|
Race
|
Asian
|
–0.08738*
|
–0.07528*
|
–0.06485*
|
–0.04811*
|
–0.07593*
|
–0.08986*
|
|
Black or African American
|
–0.11010*
|
–0.11810*
|
–0.07687*
|
–0.08903*
|
–0.08332*
|
–0.09633*
|
|
Other
|
–0.03820*
|
–0.05418*
|
–0.02030*
|
–0.02648*
|
–0.04508*
|
–0.03948*
|
|
White
|
0
|
0
|
0
|
0
|
0
|
0
|
|
Ethnicity
|
Hispanic or Latino
|
0.00588
|
–0.00889
|
0.00366
|
–0.01943*
|
0.00912
|
0.00427
|
|
Non-Hispanic
|
0
|
0
|
0
|
0
|
0
|
0
|
|
Degree type
|
DO
|
–0.01168
|
–0.04635*
|
–0.00790
|
–0.02747*
|
0.00598
|
0.00431
|
|
MD
|
0
|
0
|
0
|
0
|
0
|
0
|
|
Age (in years)
|
<35
|
0.04818*
|
0.06141*
|
0.02926*
|
0.03635*
|
0.03719*
|
0.05083*
|
|
≥35
|
0
|
0
|
0
|
0
|
0
|
0
|
|
PGY-1 in-training examination score
|
High
|
0.17240*
|
0.03861*
|
0.13370*
|
0.19090*
|
0.14810*
|
0.12340*
|
|
Medium
|
0.07969*
|
0.18000*
|
0.06198*
|
0.08246*
|
0.05989*
|
0.05314*
|
|
Low
|
0
|
0
|
0
|
0
|
0
|
0
|
|
Site of medical training
|
IMG
|
–0.05427*
|
–0.07547*
|
–0.05817*
|
–0.06819*
|
–0.03732
|
–0.03703
|
|
US/CAN
|
0
|
0
|
0
|
0
|
0
|
0
|
Across all milestones we found consistent patterns of a positive relationship between being female, younger, and having higher ITE scores and milestone ratings. For example, being female was associated with an increase in five of six milestone ratings between 0.01633 and 0.03613.
In this large national study of family medicine residents, we found no major differences in milestone ratings between IMGs and USMGs. More than half of the residencies in the United States have less than 10% IMG graduates, though IMGs make up a large portion of the primary care workforce (23.8%). Studies have shown that IMGs provide comparable if not better care for their patients. 23-26 In the 2024 Match season, out of 5,213 family medicine residency openings, 636 of went unfilled. 4 The number of primary care physicians produced each year must increase by an estimated 21% to meet the needs of the US population by 2035. 27 If no significant difference exists in the progression of milestone achievement between IMGs and USMGs, programs should feel comfortable increasing the number of IMG residents they train in order to meet the growing primary care need in this country.
While no large differences in milestone ratings were seen when comparing IMGs and USMGs, we noticed a small statistically significant difference in interpersonal and communication skills and professionalism milestone ratings that was present only in programs with a lower historical percentage of IMGs (34%–66%). The statistically significant decrease in these two competencies was not observed for graduates who attended a program with a higher historical percentage of IMGs (67%–100%). Possible explanations for this reversal are that IMG residents get better support in residencies with a historically high percentage of IMG, or these programs have different expectations from faculty, though that would require further study.
Our findings must be interpreted with caution because the magnitudes of our findings are small. While many of our findings have statistical significance, no standard definition of a “meaningful difference” in milestones exists beyond the 0.5 increment in possible scores. Our largest association between the medical knowledge milestone and a higher ITE score was 0.18. That is slightly larger than the standard deviation for a milestone rating but is only a third of the difference between possible ratings. 17 Interpreting our findings based on these data, we are reassured that the slope of each competency in each group is moving upward, but defining a meaningful difference among two groups across subcompetencies is difficult.
Across multiple milestones, we found consistent positive associations between residents being female, younger in age, and having a higher ITE score with increased milestone ratings, while race other than White was negatively associated with milestone ratings. Female gender, younger age, and higher ITE score have shown positive association with successful passing of the initial board certification examination, but not much data or conflicting data exist comparing these characteristics with milestone ratings. 28-36 Residents who are IMGs and non-White race might have a different progression in their milestones; identifying their needs and providing an appropriate support system is crucial. Findings of this study could be helpful to programs with a lower percentage of IMGs; they could consider collaborating with programs with a higher percentage of IMGs for faculty development on ways to help IMGs get acculturated to the US health care system. Our results can help residency programs to assist residents in developing an individualized learning plan (ILP) and to focus on early intervention if needed. When developing an ILP for each resident, especially an IMG, residency programs should take into consideration age, gender, and ITE scores.
Our findings are subject to multiple limitations. First, we could not reliably distinguish US-born IMGs from foreign-born IMGs. In 2023, ABFM did add a question on self-reported national origin on the initial certification questionnaire completed by final-year residents. In an exploratory analysis, we tried to use Caribbean medical school as a proxy for US citizen IMG; but in testing this against self-reported origin, the correlation was too low to use reliably. Second, no international Doctor of Osteopathic Medicine (DO) medical schools exist, so this study cannot perform direct comparison of IMGs to USMGs from DO schools. Third, ABFM data lacked information about USMGs who did not take the ABFM board certification exam. Fourth, the milestone ratings are assigned by each residency with variability between programs 37 that likely introduces some measurement bias. Finally, this study cannot control for a resident’s life experiences, personality, and work habits, which could limit our explanatory power.
Though not statistically significant for most milestone ratings, IMGs had slightly lower ratings compared to USMGs. However, both groups showed similarly positive progression of ratings during residency, with most becoming equivalent by graduation. This finding was most likely to be seen in IMGs who trained in residencies with a higher historical percentage of IMG residents.
While the gap in the projected need for primary care physicians is increasing 38 and evidence suggests that quality care provided by IMGs is equivalent to that of USMGs, 23-26 many residency programs do not take IMGs in the Match, leaving many unfilled positions. Residency programs that do not historically take IMGs should consider them to help bridge this gap in societal needs. Programs with a lower percentage of IMGs could build collaborations with programs with higher IMG percentages for developing appropriate support system for IMGs. Early implementation of an ILP for IMGs would be a great way to recognize barriers and support these learners to overcome barriers in acculturating to a new health care system and country.
Presentations
This work was presented at the Society of Teachers of Family Medicine Annual Conference, May 2025, Salt Lake City, UT.
Dr Songara was supported by the American Board of Family Medicine Foundation.
References
-
-
-
-
-
Dorgan KA, Lang F, Floyd M, Kemp E. International medical graduate-patient communication: a qualitative analysis of perceived barriers.
Acad Med. 2009;84(11):1,567-1,575.
doi:10.1097/ACM.0b013e3181baf5b1
-
Meghani SH, Rajput V. Perspective: the need for practice socialization of international medical graduates—an exemplar from pain medicine.
Acad Med. 2011;86(5):571-574.
doi:10.1097/ACM.0b013e318212e08b
-
Gozu A, Kern DE, Wright SM. Similarities and differences between international medical graduates and U.S. medical graduates at six Maryland community-based internal medicine residency training programs.
Acad Med. 2009;84(3):385-390.
doi:10.1097/ACM.0b013e318197321b
-
Hall P, Keely E, Dojeiji S, Byszewski A, Marks M. Communication skills, cultural challenges and individual support: challenges of international medical graduates in a Canadian healthcare environment.
Med Teach. 2004;26(2):120-125.
doi:10.1080/01421590310001653982
-
Zulla R, Baerlocher MO, Verma S. International medical graduates (IMGs) needs assessment study: comparison between current IMG trainees and program directors.
BMC Med Educ. 2008;8(1):42.
doi:10.1186/1472-6920-8-42
-
Narasimhan S, Ranchord A, Weatherall M. International medical graduates’ training needs: perceptions of New Zealand hospital staff. N Z Med J. 2006;119(1236):U2027.
-
Osta AD, Barnes MM, Pessagno R, Schwartz A, Hirshfield LE. Acculturation needs of pediatric international medical graduates: a qualitative study.
Teach Learn Med. 2017;29(2):143-152.
doi:10.1080/10401334.2016.1251321
-
Sockalingam S, Hawa R, Al-Battran M, Abbey SE, Zaretsky A. Preparing international medical graduates for psychiatry residency: a multi-site needs assessment.
Acad Psychiatry. 2012;36(4):277-281.
doi:10.1176/appi.ap.09110219
-
Boulet JR, McKinley DW, Whelan GP, Van Zanten M, Hambleton RK. Clinical skills deficiencies among first-year residents: utility of the ECFMG clinical skills assessment.
Acad Med. 2002;77(10):S33-S35.
doi:10.1097/00001888-200210001-00011
-
Davis C, Krishnasamy M, Morgan ZJ, Bazemore AW, Peterson LE. Academic achievement, professionalism, and burnout in family medicine residents.
Fam Med. 2021;53(6):423-432.
doi:10.22454/FamMed.2021.541354
-
Doe S, Coutinho AJ, Weidner A, et al. Prevalence and predictors of burnout among resident family physicians.
Fam Med. 2024;56(3):148-155.
doi:10.22454/FamMed.2024.875388
-
Al-Haddad M, Mulholland C, Gardner J. Burnout in international medical graduate trainees in the United Kingdom compared to domestic medical graduate trainees. analysis of data from the GMC’s national training survey in 2019 and 2021.
Perspect Med Educ. 2023;12(1):228-236.
doi:10.5334/pme.1036
-
-
Park YS, Hamstra SJ, Yamazaki K, Holmboe E. Longitudinal reliability of milestones-based learning trajectories in family medicine residents.
JAMA Netw Open. 2021;4(12):e2137179.
doi:10.1001/jamanetworkopen.2021.37179
-
Walters J, Paradise Black N, Yurttutan Engin N, Cohen DE, Ben Khallouq B, Chen JG. Race and gender differences in pediatric milestone levels: a multi-institutional study.
Clin Pediatr (Phila). 2024;63(7):977-985.
doi:10.1177/00099228231200985
-
Hauer KE, Jurich D, Vandergrift J, et al. Gender differences in milestone ratings and medical knowledge examination scores among internal medicine residents.
Acad Med. 2021;96(6):876-884.
doi:10.1097/ACM.0000000000004040
-
Lett E, Tran NK, Nweke N, et al. Intersectional disparities in emergency medicine residents’ performance assessments by race, ethnicity, and sex.
JAMA Netw Open. 2023;6(9):e2330847.
doi:10.1001/jamanetworkopen.2023.30847
-
-
Norcini JJ, Boulet JR, Dauphinee WD, Opalek A, Krantz ID, Anderson ST. Evaluating the quality of care provided by graduates of international medical schools.
Health Aff (Millwood). 2010;29(8):1,461-1,468.
doi:10.1377/hlthaff.2009.0222
-
Mick SS, Comfort ME. The quality of care of international medical graduates: how does it compare to that of U.S. medical graduates?
Med Care Res Rev. 1997;54(4):379-413.
doi:10.1177/107755879705400401
-
Tsugawa Y, Jena AB, Orav EJ, Jha AK. Quality of care delivered by general internists in US hospitals who graduated from foreign versus US medical schools: observational study.
BMJ. 2017;356:j273.
doi:10.1136/bmj.j273
-
Tsugawa Y, Dimick JB, Jena AB, et al. Comparison of patient outcomes of surgeons who are US versus international medical graduates.
Ann Surg. 2021;274(6):e1,047-e1,055.
doi:10.1097/SLA.0000000000003736
-
Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035.
Ann Fam Med. 2015;13(2):107-114.
doi:10.1370/afm.1760
-
Rahimpour A, Morrison M, Denning DA, Bown P, Ray P, Barry R. A comparative American Board of Surgery In-Training Examination (ABSITE) performance analysis between international vs. domestic graduates and doctor of medicine (MD) vs. docttor of osteopathic medicine (DO) medical degrees.
Cureus. 2024;16(6):e62358.
doi:10.7759/cureus.62358
-
Kanna B, Gu Y, Akhuetie J, Dimitrov V. Predicting performance using background characteristics of international medical graduates in an inner-city university-affiliated internal medicine residency training program.
BMC Med Educ. 2009;9(1):42.
doi:10.1186/1472-6920-9-42
-
Schabort I, Esfahani MA, Couban R, et al. Predictors for success and failure in international medical graduates: a systematic review of observational studies.
BMC Med Educ. 2024;24(1):892.
doi:10.1186/s12909-024-05837-w
-
Andrew RF. How do IMGs compare with Canadian medical school graduates in a family practice residency program? Can Fam Physician. 2010;56(9):e318-e322.
-
Ost SR, Wells D, Goedecke PJ, Tolley EA, Kleinman M, Thompson NS. Relationship between standardized test scores and board certification exams in a combined internal medicine/pediatrics residency program.
Cureus. 2021;13(2):e13567.
doi:10.7759/cureus.13567
-
Rayamajhi S, Dhakal P, Wang L, Rai MP, Shrotriya S. Do USMLE steps, and ITE score predict the American Board of Internal Medicine certifying exam results?
BMC Med Educ. 2020;20(1):79.
doi:10.1186/s12909-020-1974-3
-
Seaberg PH, Kling JM, Klanderman MC, et al. Resident factors associated with American Board of Internal Medicine certification exam failure.
Med Educ Online. 2023;28(1):2152162.
doi:10.1080/10872981.2022.2152162
-
Klein R, Julian KA, Snyder ED, et al; Gender Equity in Medicine (GEM) workgroup. Gender bias in resident assessment in graduate medical education: review of the literature.
J Gen Intern Med. 2019;34(5):712-719.
doi:10.1007/s11606-019-04884-0
-
Santen SA, Yamazaki K, Holmboe ES, Yarris LM, Hamstra SJ. Comparison of male and female resident milestone assessments during emergency medicine residency training: a national study.
Acad Med. 2020;95(2):263-268.
doi:10.1097/ACM.0000000000002988
-
Santen SA, Ryan MS, Fancher TL, et al. Variability in learner performance using the ACGME harmonized milestones during the first year of postgraduate training.
Acad Med. 2025.
doi:10.1097/ACM.0000000000006053
-
Bazemore AW, Petterson SM, McCulloch KK. US Primary care workforce growth: a decade of limited progress, and projected needs through 2040. J Gen Intern Med. 2025;40(2):339-346.



There are no comments for this article.