Background and Objectives: Many past studies have focused on uncertainty in medical practice, yet it is still not well understood in the field of family medicine, especially among residents. The aim of this study was to examine situations in which residents experience uncertainty and the coping strategies they use to deal with it. The results may have implications for advanced training programs and the specialist training in family medicine.
Methods: We conducted semistandardized interviews with 15 residents and young family doctors from Hesse, Germany and asked them to describe cases in which they experienced uncertainty. In total, 40 cases were reported. Using established methods, we derived a coding system with different categories.
Results: Uncertainty occurred in a broad and heterogenous range of cases, and it often involved complex interaction of biomedical, interpersonal, and psychosocial factors. The participants described various strategies that were helpful in dealing with the three different types of uncertainty. To deal with biomedical uncertainty, the residents primarily found information-seeking and consulting more experienced colleagues to be useful. In dealing with interpersonal and psychosocial uncertainty, they applied reflective strategies. Participants suggested open communication and honest dialogue about uncertainty and the thematization of the topic at much earlier stages (eg, during medical studies).
Conclusions: Family medicine residents experience uncertainty as an important part of their daily work. They do not necessarily interpret it as a negative phenomenon. Instead, uncertain situations often accompany learning effectiveness and an increase of self-confidence.
The phenomenon of uncertainty in medical practice has been the focus of many previous studies. Some of this research has led to the creation of various taxonomies as a means of classifying the causes of uncertainty. For example, Beresford identified three types of uncertainty based on its source: technical, conceptual, or personal. 1 Hamui-Sutton et al examined critical incidents in which residents coped with the perception of uncertainty, and they distinguished technical, conceptual, communicational, ethical, and systemic uncertainty. 2 Han et al developed a three-dimensional integrative concept of uncertainty in health care settings among patients and doctors, with uncertainty being defined as the subjective perception of ignorance and being classified according to source, issue, and locus. 3 Pomare et al developed a revised model of complex health care settings, which should be universally applicable to various health care settings. 4
Research also has been conducted to explore physicians’ reactions to uncertainty and their strategies for dealing with it. To examine the affective reaction of physicians to uncertainty, Gerrity et al developed the Physicians’ Reaction to Uncertainty scale. They found that internal medicine subspecialists and surgeons reported less stress from uncertainty than generalists. 5 Farnan et al found that information-seeking strategies and consultation with more experienced colleagues in a defined hierarchy of assistance were particularly helpful for residents in internal medicine in dealing with uncertainty. 6 Han et al identified different strategies for dealing with uncertainty within a conceptual taxonomy. Specifically, a temporal evolution exists in the context of uncertainty that coincides with a higher level of flexibility, humility, and openness. 7 According to Light, a tempered control of uncertainty in medical practice is needed. Knowledge of uncertainty and possible human errors is important; sometimes overcoming uncertainty to make medical decisions is necessary. 8 Virtues such as courage, curiosity, and diligence help to avoid pitfalls caused by uncertainty. 9
Among family doctors, researchers identified an association between intolerance of uncertainty and a higher level of diagnostic activity. 10 Personality traits such as neuroticism can influence how individuals handle uncertainty. 11 In addition, experience appears to be a factor. For example, compared to more experienced doctors, residents in family medicine seem to be more afraid of committing medical errors and use different strategies for dealing with uncertainty. 12 They also experience higher levels of anxiety related to uncertainty and are more concerned about potential adverse outcomes. 13 This same group of physicians also demonstrated an association between a lower tolerance of uncertainty and a higher risk of burnout. 14 During a 6-month clinical rotation in a family physician’s office, a reduction of anxiety related to uncertainty was noted among first- and second-year family medicine residents.15 Residents describe uncertainty as inherent in their specialty and as an implicit part of their personality. Information-seeking strategies seem to be particularly helpful for residents in dealing with uncertainty, and the reluctance to disclose it to patients associated with a higher level of medical experience has increased. 16 An exploratory study tested the effects of a novel curriculum created to improve the tolerance of ambiguity among residents in family medicine. 17 When family medicine residents start to work in a doctor’s office, they encounter a lot of differences from the circumstances they knew from their work in a hospital. Diagnostic and therapeutic strategies differ, and residents often use a strategy of stalling for time. Ruling out and avoiding dangerous developments and coping with the related risk can be challenging for them. In some cases, a concrete diagnosis is not necessary, yet the residents feel the need to conclude something even when no medical indication for a specific treatment exists. In addition, the patient population differs from that of hospitals, and the doctor-patient relationships are much closer and cooperative. 18 These close relationships need to be established by the doctors when they begin to work in the outpatient setting. Coping with these differences can increase residents’ self-confidence but also can cause stress and uncertainty. The phenomenon of uncertainty in this group has received little attention by researchers. This study aims to delve deeper into the situations that evoke feelings of uncertainty among family medicine residents in Hesse, Germany. In Germany, the curriculum of the specialist training in family medicine includes a 12-month inpatient rotation in internal medicine and a 24-month outpatient rotation in a family doctor’s office. Furthermore, a course in psychosomatic care is mandatory. 19 The analysis of cases where residents in family medicine describe the perception of uncertainty reveals new perspectives on its origins and coping strategies. Particularly, the essential role of interpersonal and psychosocial sources on the emergence of uncertainty becomes clear. This role characterizes the unique field of family medicine, where doctor-patient relationships are often long-lasting and examination techniques are more focused on the case history and clinical examination than on new imaging techniques. Family doctors frequently encounter the psychosocial environment of their patients, which also influences medical decision-making. Strategies to cope with uncertainty in this field, therefore, also address these interpersonal and psychosocial issues. This finding demonstrates a new view on uncertainty, considering it as a multimodal phenomenon influenced by biomedical, interpersonal, and psychosocial factors.
Fifteen residents and young family doctors from Hesse participated in this qualitative study. We recruited the participants via workshops for specialist training in family medicine between December 2019 and September 2021. To qualify, the participants had to be in a family medicine rotation for more than 3 months and had to have completed the specialist examinations within the last 3 months.
We conducted semistandardized interviews with the participants between February 2020 and September 2021. Due to COVID-19-related contact restrictions, most of the interviews were performed via phone or video call. Prior to the interviews, every participant signed a declaration of consent. The participants had to prepare two to four cases that took place in the outpatient setting and were associated with a feeling of uncertainty. The participants received a questionnaire as a support to help them reflect on cases particularly in view of the kind of consultation, demographic characteristics of the patient, reaction, feelings, satisfaction with the outcome of the situations, and reasons they chose to highlight the case. The participants used this questionnaire as a memory aid in the interviews; it wasn’t included in the final analysis. At the beginning of the interview, each participant was asked to describe one of the cases with regard to the topics guided by the questionnaire. Furthermore, topics related to the reported case were discussed, such as issues of the health care system, the COVID-19 pandemic, and residency programs. All prepared cases were discussed following this format.
The study design was reviewed and approved by the institutional review board of the University of Marburg. The transcription of the interviews was performed using the software program F4 (Audiotranskription IT company, Marburg, Germany). We developed a coding system by applying Kuckartz’s methods of qualitative content analysis. 20 These include a systematic, software-supported approach. Two independent members of our research group performed the analytical process. We used free, inductive coding, without preconceived theories. First, we reviewed the narrative material and identified patterns and key ideas. From that analysis, we then developed preliminary codes, which were applied across the dataset. Through an iterative process, we refined and consolidated these codes and developed a classification system with themes and subthemes. During regular discussions among our interdisciplinary research group members, we evaluated the classification system to incorporate our diverse perspectives, reduce individual biases, and arrive at a profound and nuanced understanding of our data. We used the 2020 version of MAXQDA (VERBI Software) for coding.
Characteristics of the Participants and Interviews
The 15 participants in this study described a total of 40 cases. Table 1 summarizes the characteristics of the participants and the interviews.
|
Characteristics of the sample
|
n (%)
|
Mean (range)
|
Median
|
|
Gender
|
|
|
|
|
Male
|
4 (26.67)
|
|
|
|
Female
|
11 (73.33)
|
|
|
|
Other
|
0
|
|
|
|
Age (years)
|
|
35.67 (31-44)
|
35
|
|
Professional experience in family medicine (years)
|
|
<1
|
8 (53.33)
|
|
|
|
1–2
|
2 (13.33)
|
|
|
|
>2
|
5 (33.33)
|
|
|
|
Mother tongue
|
|
German
|
15 (100)
|
|
|
|
Other
|
0
|
|
|
|
Completed residency in another medical specialization
|
|
Yes
|
3 (20.00)
|
|
|
|
No
|
12 (80.00)
|
|
|
|
Characteristics of the interviews
|
|
Interview duration
|
|
45.54 (23:35-71:44)
|
|
|
Method
|
|
|
|
|
Phone call
|
11 (73.33)
|
|
|
|
Video call
|
3 (20.00)
|
|
|
|
Face-to-face meeting
|
1 (6.67)
|
|
|
Three Types of Uncertainty
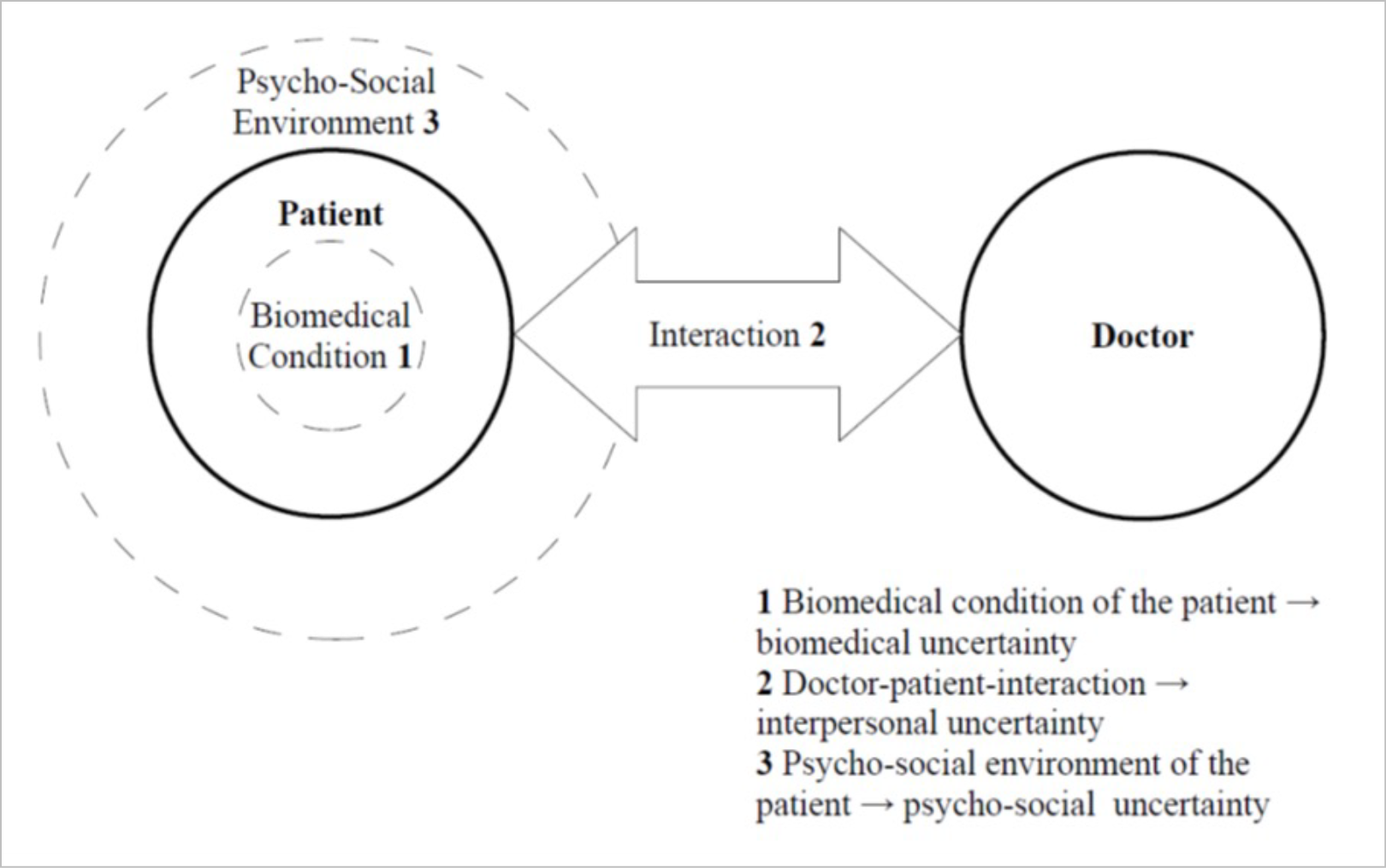
The participants’ case descriptions enabled us to distinguish three different types of uncertainty: biomedical, interpersonal, and psychosocial. Biomedical uncertainty occurs as a doctor tries to understand and treat the patient’s condition, and it involves aspects such as diagnostic or therapeutic decision-making. Interpersonal uncertainty can arise from the direct interaction between doctor and patient, such as in communication processes. Psychosocial uncertainty can appear in the doctor’s direct or indirect reaction or understanding of the psychosocial environment of the patient (eg, employment, family situation, or housing situation). Table 2 shows some examples of these three types of uncertainty from the narrative material. Figure 1 presents a visualization of the emergence of these three types of uncertainty.
|
Type of uncertainty
|
Example from the narrative material
|
|
Biomedical uncertainty
|
A doctor has to decide which measures are indicated for a patient who has high fever but no other symptoms: “And then I took her history and measured the vital parameters—blood pressure, heart rate, and I examined her completely to see if there’s a reason for this high fever. . . . But it was strange that there was no other symptom which explained the high fever. I was concerned about this one value although the other parameters were totally normal.” (Interview 4, case 2)
|
|
Interpersonal uncertainty
|
A doctor feels stressed and manipulated in a conversation with a patient: “Then he talked about his drug trips and that he tried suicide several times. Then he changed the topic to his trauma therapy. And then he told me again that he wants to get the codeine. The conversation was totally confusing. I was totally involved in this situation, and it wasn’t possible for me to distance in this moment. . . . And then I realized that I was totally overwhelmed in this moment.” (Interview 4, case 1)
|
|
Psychosocial uncertainty
|
A doctor feels helpless and uncertain in caring for a patient who lives in difficult psychosocial life circumstances: “Finally, she got in conflict with her new partner, and he wanted to throw her out. She went to another appointment where she was very confused because of the separation of her previous partner, the conflicts with her family, and now with her new partner. In this situation I felt helpless because the patient told me she is homeless now and she also has to care for some pets.” (Interview 10, case 1)
|
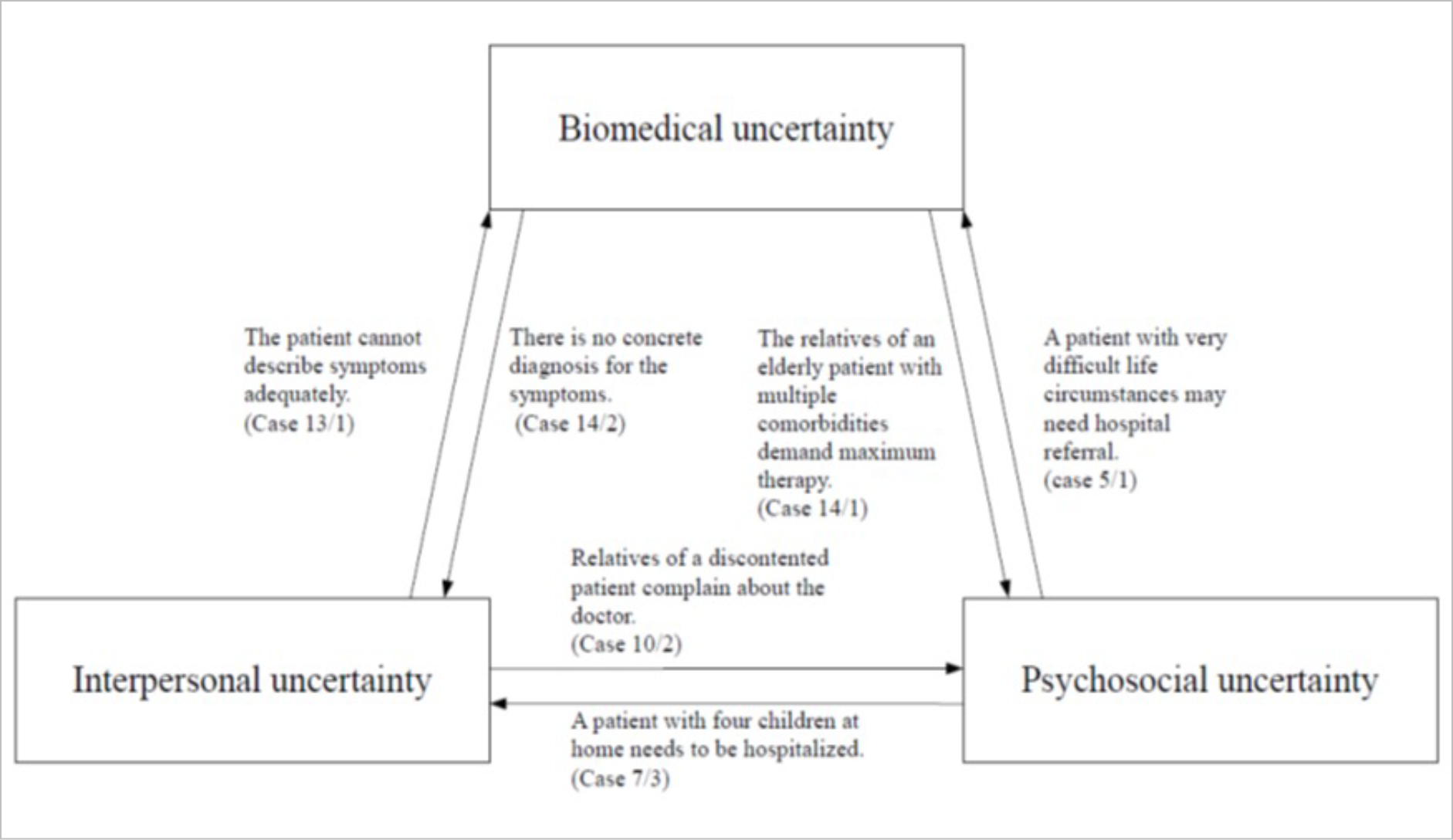
Interactions Among the Three Types of Uncertainty
Most of the described situations featured more than one type of uncertainty, which suggests that the interactions among biomedical, interpersonal, and psychosocial sources of uncertainty are often complex. Table 3 presents examples from the narrative material of these interactions, and Figure 2 provides a visual of the examples.
|
Interaction
|
Example from the narrative material
|
|
Biomedical → interpersonal
|
The doctor has to tell the patient that there’s no concrete diagnosis for the symptoms and now has to cope with the expectations of the patient: “All you see are just the expectations of the patients and you think I have to make a diagnosis or schedule a therapy. But there are so many things where you can’t make a concrete diagnosis, or you just can start an unspecific therapy. And this is very unsatisfying for many patients.” (Interview 14, case 2)
|
|
Interpersonal → biomedical
|
A patient isn’t able to describe her symptoms adequately. Therefore, it’s complicated for the doctor to assess the situation: “It wasn’t clear for me what happened because the patient told me about a previous hospital stay all the time and that she’s not doing well. And when I asked her about it, she always told me that she had a feeling of dizziness when she took a shower. . . . But it was very difficult because even on direct demands she didn’t answer adequately.” (Interview 13, case 1)
|
|
Interpersonal → psychosocial
|
Relatives of a discontented patient complain about the doctor in the village: “I wasn’t very satisfied with the outcome of the situation, because it’s always inappropriate if the interaction isn’t between the patient and me as the doctor, but through the relatives.” (Interview 10, case 2)
|
|
Psychosocial → interpersonal
|
A doctor has to tell a patient who she knows is caring for four children that she has to go to the hospital shortly: “And then I told her that I know she’s the mother of four children and that this is very abrupt for her. But she should go to the appointment tomorrow, because there’s just one chance to get an appointment that fast. And then she understood it.” (Interview 7, case 3)
|
|
Psychosocial → biomedical
|
A doctor has to decide whether a patient she knows is living in difficult psychosocial circumstances has to be referred to the hospital: “A very young woman, from who I knew her father died recently because of a heart attack. . . . I knew she doesn’t want to go to hospital for clinical monitoring and that she’s afraid of hospitals.” (Interview 5, case 1)
|
|
Biomedical → psychosocial
|
Relatives of an elderly patient with multiple comorbidities demand maximum therapy: “And that was a case where it was difficult to find an adequate therapy. There was always a lot of uncertainty to strike a balance between medical over- and undersupply. . . . Especially in a palliative setting when relatives have different goals than the doctor, then there’s often a lot of uncertainty.” (Interview 14, case 1)
|
Coping Strategies
Different strategies are helpful to deal with the three types of uncertainty reported by participants. These can be prospective, retrospective, or effective short-term or long-term strategies.
To cope with biomedical uncertainty, the participants often described the use of information-seeking strategies. For example, consulting more experienced colleagues seemed to be helpful and also was described as a sharing of responsibility. The application of diagnostic and therapeutic strategies such as safety netting and the sharing of uncertainty with the patient also could help to reduce biomedical uncertainty. Furthermore, a deliberate and thorough approach with detailed documentation of the case and objective examination results (eg, scores) could simplify medical decision-making.
In dealing with interpersonal and psychosocial uncertainty, reflective and retrospective strategies such as Balint groups and mentoring groups were identified as being useful. Balint groups, which focus on analyzing critical doctor-patient interactions, are a mandatory part of the specialist training in family medicine in Germany. The reflection is performed in a group setting with trained supervisors such as psychologists, psychiatrists, or family physicians. In mentoring groups, the participants are supported by experienced family doctors. These groups focus on organizational and personal topics such as professional concerns. In Hesse, these groups are organized by academic departments of family medicine, which provides structured further education and support for physicians in their training in general and in pediatric medicine from medical school to specialist certification. Reflection with the medical trainer or in private surroundings also plays an important role.
To reduce uncertainty in the doctor-patient interaction, the participants often applied communication skills such as active listening and paraphrasing. An emphatic communication style with a positive attitude toward the patient can create a trusting atmosphere between the doctor and the patient. Furthermore, preparing for a difficult conversation or undertaking critical conversations together with the medical trainer can reduce interpersonal uncertainty.
Psychosocial care in family medicine can be implemented through frequent and short-term appointments for patients in critical psychosocial life circumstances. This approach enables the doctor to establish a trustful doctor-patient relationship and to evaluate the dynamic of the psychosocial situation of the patient.
Reflection on the Topic of Uncertainty
Uncertainty was not necessarily interpreted as a negative phenomenon. Rather, the participants described the perception of uncertainty as a motivation to reflect on their own behavior and to consider alternative strategies. They considered this topic as important and relevant for their daily work and their specialist training in family medicine. They also expressed that an open exchange regarding uncertainty is important for dealing with it. In addition, they noted that this topic should be addressed much earlier, for example, in a mentoring program during medical studies. Through a reflection of uncertain situations with experienced physicians, students can grasp the ubiquitous existence of uncertainty in medicine and learn to deal with it early.
Moreover, the residents indicated that an acceptance of the risk of making mistakes should be supported. In some of the cases, bad outcomes were reported even though the doctors were acting according to medical standards and to the best of their knowledge. These pseudo-errors are random results and cannot be prevented by doctors. 21, 22
The perception of uncertainty did not necessarily decline during the time spent in specialist training in family medicine. One of the participants who worked in family medicine for 2 years described initially having a more naïve approach at the beginning of his work in the doctor’s office. He said that the increase in his professional experience also was accompanied by an increase in knowledge of the potential consequences of his own decisions.
DISCUSSION AND CONCLUSIONS
In this qualitative study, the participating residents reported a broad spectrum of patient cases, reflecting the professional broadness that characterizes the field of family medicine. An analysis of the narrative material indicated that residents in family medicine are faced with three types of uncertainty: biomedical, interpersonal, and psychosocial. To deal with these types, different coping strategies are promising. In dealing with biomedical uncertainties, the residents described the use of information-seeking strategies, whereas interpersonal and psychosocial challenges often can be handled by applying reflective strategies. Furthermore, our material has given evidence that the three types sometimes intersect. This intersection may evoke critical questions regarding their validity or usefulness but reflects the practice environment experienced by our interviewees, where parallel and sometimes contradicting challenges occurred. In the field of family medicine, long-term doctor-patient relationships with an intimate understanding of psychosocial contexts still prevail. Furthermore, diagnostic efforts are more focused on the case history, with technical investigations having much less relevance. Consequently, the influence of interpersonal and psychosocial factors on medical decision-making is much higher than in other medical fields.
From these insights, recommendations for medical training can be deduced. The integration of self-reflection in the curriculum could enhance young physicians’ intuitive skills and their ability to use emotional cues effectively in patient interactions. This integration currently is being addressed with Balint groups, mentoring groups, or supervision programs, as available in residency programs in Hesse. Here, the supportive role of the medical trainer regarding the management of uncertainties, with implications regarding professionalism and emotional support, is extremely important. Regular appointments to reflect on critical cases with the medical trainer offer an opportunity to deal with the interpersonal or psychosocial uncertainties described earlier.
Furthermore, development of communication skills such as active listening and empathy should be supported. During some workshops, by including role-play or innovative techniques such as virtual reality, complex doctor-patient interactions can be simulated. These workshops should be offered early, such as during basic medical training, to increase students’ awareness of the importance of these skills. At a more general level, through the strengthening of psychology and social science in the medical curriculum, young doctors can improve their understanding of the complex psychosocial and interpersonal influences on patient care. Here, a close collaboration with other professional groups such as social workers and psychologists could be supportive in realizing this goal.
For the interpretation of our findings, paying attention to potential limitations concerning the generalization of the participant population of the study is necessary. Regarding demographic characteristics, the sample reflected the population of residents in family medicine in Hesse. All the participants were German native speakers. Therefore, examining the influence of linguistic and cultural factors on the perception of uncertainty in this sample was not possible. Moreover, many of the participating residents had prior medical training in other disciplines. The identification with the role as a physician as a possible source of uncertainty could be underestimated in this sample. Additionally, the participants in this study may have been more open-minded and empathic than average family doctors. Lastly, we cannot exclude social desirability affecting their responses.
Generally, the results of our study provide unique insights into young family doctors’ perception of uncertainty during their daily work in the doctor’s office. Clearly, uncertainty is not necessarily understood as something adverse by the doctors. Rather, the doctors have seen uncertainty as a possibility for reflecting on one’s own behavior and decisions. The participants in this study demand stronger emphasis on uncertainties and appropriate coping strategies in residency programs and basic medical training. Future research should focus on long-term effects of coping strategies and the creation of learning opportunities regarding this topic.
References
-
Beresford EB. Uncertainty and the shaping of medical decisions.
Hastings Cent Rep. 1991;21(4):6-11.
doi:10.2307/3562993
-
Hamui-Sutton A, Vives-Varela T, Gutiérrez-Barreto S, Leenen I, Sánchez-Mendiola M. A typology of uncertainty derived from an analysis of critical incidents in medical residents: a mixed methods study.
BMC Med Educ. 2015;15(1):198.
doi:10.1186/s12909-015-0459-2
-
Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy.
Med Decis Making. 2011;31(6):828-838.
doi:10.1177/0272989X10393976
-
Pomare C, Churruca K, Ellis LA, Long JC, Braithwaite J. A revised model of uncertainty in complex healthcare settings: a scoping review.
J Eval Clin Pract. 2019;25(2):176-182.
doi:10.1111/jep.13079
-
Gerrity MS, Earp JAL, DeVellis RF, Light DW. Uncertainty and professional work: perceptions of physicians in clinical practice.
Am J Sociol. 1992;97(4):1,022-1,051.
doi:10.1086/229860
-
Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM. Resident uncertainty in clinical decision making and impact on patient care: a qualitative study.
Qual Saf Health Care. 2008;17(2):122-126.
doi:10.1136/qshc.2007.023184
-
Han PKJ, Strout TD, Gutheil C, et al. How physicians manage medical uncertainty: a qualitative study and conceptual taxonomy.
Med Decis Making. 2021;41(3):275-291.
doi:10.1177/0272989X21992340
-
Light D Jr. Uncertainty and control in professional training. J Health Soc Behav. 1979;20(4):310-322. doi:10.2307/2955407
-
Reis-Dennis S, Gerrity MS, Geller G. Tolerance for uncertainty and professional development: a normative analysis.
J Gen Intern Med. 2021;36(8):2,408-2,413.
doi:10.1007/s11606-020-06538-y
-
Schneider A, Löwe B, Barie S, Joos S, Engeser P, Szecsenyi J. How do primary care doctors deal with uncertainty in making diagnostic decisions?
J Eval Clin Pract. 2010;16(3):431-437.
doi:10.1111/j.1365-2753.2010.01464.x
-
Schneider A, Wübken M, Linde K, Bühner M. Communicating and dealing with uncertainty in general practice: the association with neuroticism.
PLOS One. 2014;9(7):e102780.
doi:10.1371/journal.pone.0102780
-
Nevalainen M, Kuikka L, Pitkälä K. Medical errors and uncertainty in primary healthcare: a comparative study of coping strategies among young and experienced GPs.
Scand J Prim Health Care. 2014;32(2):84-89.
doi:10.3109/02813432.2014.929820
-
Cooke G, Tapley A, Holliday E, et al. Responses to clinical uncertainty in Australian general practice trainees: a cross-sectional analysis. Med Educ. 2017;51(12):1,277-1,288.
-
Cooke GP, Doust JA, Steele MC. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars.
BMC Med Educ. 2013;13:2.
doi:10.1186/1472-6920-13-2
-
Escourrou E, Bergeaut M, Gimenez L, et al. Evolution of reactions to uncertainty among residents during a clinical rotation.
Fam Med. 2020;52(5):339-345.
doi:10.22454/FamMed.2020.403807
-
-
Taylor D, Picker B, Woolever D, Thayer EK, Carney PA, Galper AB. A pilot study to address tolerance of uncertainty among family medicine residents.
Fam Med. 2018;50(7):531-538.
doi:10.22454/FamMed.2018.634768
-
Linde K, Maria Huber C, Barth N, Schneider A. How do young general practitioners experience the transition to general practice? a qualitative study [Wie erleben junge Allgemeinärzt*innen den Übergang in die hausärztliche Praxis? Eine qualitative Studie].
Z Evid Fortbild Qual Gesundhwes. 2020;150-152:96-102.
doi:10.1016/j.zefq.2020.02.001
-
-
Kuckartz U, ed. Einführung in die computergestützte Analyse qualitativer Daten. 3rd ed. VS Verlag für Sozialwissenschaften; 2010.
-
Donner-Banzhoff N. The pseudo-error—paradoxic risk for patients [Der Pseudo-Fehler in der Medizin—paradoxe Gefährdungen für Patienten].
Z Allg Med. 2014;90(5):200-206.
doi:10.3238/zfa.2014.0200-0206
-
Kassirer JP, Kopelman RI. Cognitive errors in diagnosis: instantiation, classification, and consequences.
Am J Med. 1989;86(4):433-441.
doi:10.1016/0002-9343(89)90342-2



There are no comments for this article.