Background and Objectives: Primary care physician (PCP) shortages and uneven geographic distribution are well-documented. Black populations have less access to primary care and worse health outcomes, with a lack of provider-patient racial concordance playing a role. Addressing these disparities requires targeted approaches that produce more Black PCPs in high-need areas, including expanding community-based residency programs (CBRPs), which are more likely to produce physicians in high-need areas. This research explores the relationship between high-need Black counties and the location of CBRPs.
Methods: We used geographic information systems to identify high-need counties—defined as those in the bottom quartile for PCP capacity for every year from 2013 to 2020 and in the top quartile for percentages of Black populations (2017–2021). Next, we applied proximity analysis to identify high-need counties within 25 and 50 miles of CBRPs.
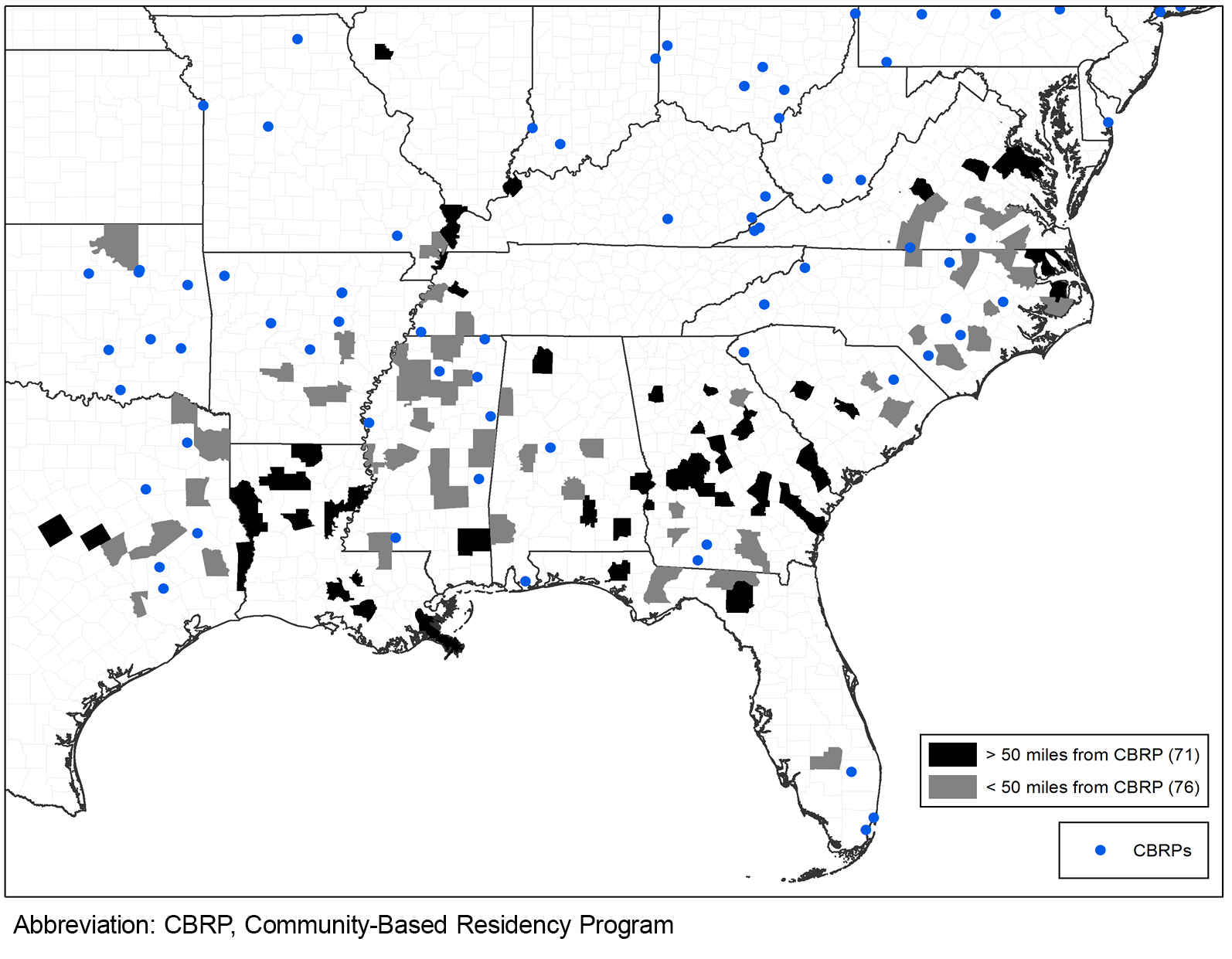
Results: More than 3 million people live in the 147 high-need counties, which are mostly in the Southern United States. Nearly 60% of the 867,000 Black people living in these counties can be found in Georgia, Mississippi, North Carolina, and Virginia. About one-half of high-need counties do not have any CBRPs located within 50 miles. More than one-third of these counties are in Georgia, Louisiana, and Virginia.
Conclusions: Increasing the number of PCPs in high-need areas requires targeted funding for expanding current and creating new CBRPs with the greatest potential of producing physicians in these areas. Future research will explore all family medicine residency programs relative to high-need areas and identify potential new program locations.
Black/White health disparities continue to persist, with Black populations having less access to care, poorer quality care, and worse health outcomes compared to White populations. 1-3 A lack of provider-patient racial concordance contributes to these disparities. 4 Increasing the number of Black people entering the physician workforce can help address these health disparities; greater representation of Black primary care physicians (PCPs) has been associated with lower mortality rates and higher life expectancy for Black populations. 5, 6 Moreover, research has found that better access to primary care is associated with improved health outcomes. 7,8
However, PCP shortages and uneven geographic distribution are well-documented and expected to worsen in coming years. 9-11 The National Academies of Science, Engineering, and Medicine report on primary care outlined steps for improving access to high-quality primary care; having an adequate supply of PCPs and training primary care teams where people live and work are both needed to make this happen. 12 Expanding graduate medical education training programs, particularly community-based residency programs (CBRPs), in high-need areas is one way to do this.
CBRPs, which we define as teaching health centers (THCs) and programs with rural training tracks (RTTs), produce physicians that are more likely to practice in rural and other underserved areas. 13-18 A recent evaluation of the THC program found that graduates were more likely to practice in rural areas and to care for populations in medically underserved areas. 13 Further, THC residents are more likely to come from rural or disadvantaged backgrounds.1 Substantial evidence exists that shows that rural CBPRs produce physicians that are more likely to practice in rural areas. 14- 17 The location of residency programs matters, because most family medicine residents remain within 50 miles of their residency graduate location. 19
Improving Black/White health disparities requires that Black populations have adequate access to PCPs. One way to do this is to ensure that CBRPs are in areas with high percentages of Black populations. This research has two primary objectives: first, to identify counties that have consistently low rates of PCP supply and high percentages of Black populations (high-need Black counties); second, to explore high-need counties within 25 and 50 miles of CBRPs.
We used the Robert Wood Johnson County Health Rankings trend data (2023) to find the number of PCPs per 100,000 population for years 2013 to 2020. 20 We also included the percentage of Black populations from the American Community Survey Five-Year Estimates (2017–2021). 21
We identified CBRPs from two sources: data on residency programs with an RTT came from the RTT Collaborative, while the data for THCs came from the Health Resources and Services Administration THC Graduate Medical Education (THCGME) program dashboards. 22, 23 This research was considered exempt by the Institutional Review Board at the American Academy of Family Physicians.
We used geographic information systems to identify high-need Black counties—defined as counties in the bottom quartile (25th percentile or lower) for PCP capacity for every year from 2013 to 2020 and counties in the top quartile (75th percentile or higher) for percentages of Black populations (2017–2021). Next, we identified counties within 25 and 50 miles of CBRPs using the proximity analysis buffer tool in ArcMap version 10.2.2 (Environmental Systems Research Institute). Distance buffers were created around each of the CBRPs, and a spatial join function was used to identify high-need counties with any part of their boundary intersecting with the 25 and 50 mile buffers. Finally, we mapped the location of CBRPs relative to high-need counties and stratified high-need counties based on their location within or outside of the 50-mile buffer (Figure 1).
Figure 1 displays high-need Black counties (N=147). More than 3 million people live in these counties, about 95% of which are in the southern United States. Nearly 60% of the 867,000 Black people living in these counties can be found in just four states (ie, Georgia, Mississippi, North Carolina, Virginia). Almost half of the population in these high-need counties can be found in nonmetropolitan areas. Not surprisingly, PCP capacity is low in these areas, with only 472 PCPs spread across almost 150 counties (a rate of 15 per 100,000, compared to the US average of about 76 per 100,000). More than one-fifth of these counties do not have a single PCP.
Figure 1 also displays the 147 CBRPs relative to high-need Black counties. More than one-quarter of CBRPs (n=44) have a high-need Black county within 50 miles, and about one-fifth (n=31) have a high-need Black county within 25 miles. While many of the CBRPs are located near high-need Black counties, almost one-half of these counties do not have any CBRPs located within 50 miles. About one-third of these counties are in just three states (ie, Georgia, Louisiana, Virginia) and comprise more than 70% of Black populations in high-need counties outside of 50 miles of a CBRP.
.
.
This research identified high-need Black counties based on consistently low rates of PCPs and high percentages of Black populations, highlighting a concentration of these areas in the Southeastern United States. Our finding is consistent with recent research documenting persistently lower rates of PCPs in high-minority counties and counties in the Southern United States. 24
Increasing the number of primary care residents training in CBRPs in high-need areas has the potential to improve access to care for high-need populations. This research found that while some CBRPs are located near high-need Black counties, many high-need areas still do not have any CBRP located within 50 miles. Increasing primary care capacity in high-need Black counties requires targeted funding for CBRPs that have the highest potential of producing physicians in these areas and creating new CBRPs in high-need counties, because family physicians often practice in areas near their training location. 16-19
Expanding CBRPs is just one part of a strategy for increasing the number of Black physicians in high-need Black counties. While graduates of CBRPs are more likely to serve in underserved areas, the percentage of Black graduates of CBRPs remains similar to other residency programs (between 5% and 8%), and training in underserved or rural areas does not guarantee future practice in that location. 13, 14 Thus, upstream efforts also are needed to support primary care pathway programs to increase the number of Black people becoming primary care providers.
This research had a few limitations, including our definition of high-need Black counties based on quartiles. The PCP quartile threshold was chosen because it is the midpoint for the two criteria for defining primary care health professional shortage areas. However, choosing other criteria for low rates of PCPs or high percentages of Black populations would have produced different results. Sensitivity analysis using other criteria (ie, terciles, outliers) produced similar results. A second limitation involved our narrow definition of CBRPs, realizing that other residency programs are producing physicians for high-need areas. Future research will explore other types of high-need areas relative to all family residency programs, including a broader definition of CBRPs, and a focus on other types of high-need populations such as other racial and ethnic minorities and those in high social deprivation areas.
The disparities in primary care access across US counties highlight the urgent need for a strategic policy approach. Ensuring that all individuals have access to high-quality primary care requires increasing the number of PCPs, improving geographic distribution, and diversifying the workforce. By expanding and targeting funding to residency programs in underserved areas, we can take significant steps toward improving health outcomes for the nation’s most vulnerable populations.
Presentations
This research was presented at the North American Primary Care Research Group Annual Meeting, November 20–24, 2024, Quebec City, Ontario, Canada.
References
-
Morgan Z, Bazemore A, Dai M, Peterson L. Racial and ethnic disparities in access to primary care during COVID-19.
Ann Fam Med. 2022;20(20, suppl 1):2790.
doi:10.1370/afm.20.s1.2790
-
Mahajan S, Caraballo C, Lu Y, et al. Trends in differences in health status and health care access and affordability by race and ethnicity in the United States, 1999-2018.
JAMA. 2021;326(7):637-648.
doi:10.1001/jama.2021.9907
-
Odlum M, Moise N, Kronish IM, et al. Trends in poor health indicators among Black and Hispanic middle-aged and older adults in the United States, 1999-2018.
JAMA Netw Open. 2020;3(11):e2025134.
doi:10.1001/jamanetworkopen.2020.25134
-
Jetty A, Jabbarpour Y, Pollack J, Huerto R, Woo S, Petterson S. Patient-physician racial concordance associated with improved healthcare use and lower healthcare expenditures in minority populations.
J Racial Ethn Health Disparities. 2022;9(1):68-81.
doi:10.1007/s40615-020-00930-4
-
Snyder JE, Upton RD, Hassett TC, Lee H, Nouri Z, Dill M. Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the US.
JAMA Netw Open. 2023;6(4):e236687.
doi:10.1001/jamanetworkopen.2023.6687
-
Peek ME. Increasing representation of Black primary care physicians—a critical strategy to advance racial health equity.
JAMA Netw Open. 2023;6(4):e236678.
doi:10.1001/jamanetworkopen.2023.6678
-
Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015.
JAMA Intern Med. 2019;179(4):506-514.
doi:10.1001/jamainternmed.2018.7624
-
Basu S, Phillips RS, Berkowitz SA, Landon BE, Bitton A, Phillips RL. Estimated effect on life expectancy of alleviating primary care shortages in the United States.
Ann Intern Med. 2021;174(7):920-926.
doi:10.7326/M20-7381
-
-
-
Markowski JH, Wallace J, Ndumele CD. After 50 years, health professional shortage areas had no significant impact on mortality or physician density.
Health Aff (Millwood). 2023;42(11):1,507-1,516.
doi:10.1377/hlthaff.2023.00478
-
-
Davis CS, Roy T, Peterson LE, Bazemore AW. Evaluating the teaching health center graduate medical education model at 10 years: practice-based outcomes and opportunities.
J Grad Med Educ. 2022;14(5):599-605.
doi:10.4300/JGME-D-22-00187.1
-
Talib Z, Jewers MM, Strasser JH, et al. Primary care residents in teaching health centers: their intentions to practice in underserved settings after residency training.
Acad Med. 2018;93(1):98-103.
doi:10.1097/ACM.0000000000001889
-
Schmitz D. The role of rural graduate medical education in improving rural health and health care.
Fam Med. 2021;53(7):540-543.
doi:10.22454/FamMed.2021.792533
-
Patterson DG, Shipman SA, Pollack SW, et al. Growing a rural family physician workforce: the contributions of rural background and rural place of residency training.
Health Serv Res. 2024;59(1):e14168.
doi:10.1111/1475-6773.14168
-
Russell DJ, Wilkinson E, Petterson S, Chen C, Bazemore A. Family medicine residencies: how rural training exposure in GME is associated with subsequent rural practice.
J Grad Med Educ. 2022;14(4):441-450.
doi:10.4300/JGME-D-21-01143.1
-
Barclift SC, Brown EJ, Finnegan SC, Cohen ER, Klink K. Teaching health center graduate medical education locations predominantly located in federally designated underserved areas.
J Grad Med Educ. 2016;8(2):241-243.
doi:10.4300/JGME-D-15-00274.1
-
-
-
-
-
-
Liu M, Wadhera RK. Primary care physician supply by county-level characteristics, 2010-2019.
JAMA. 2022;328(19):1,974-1,977.
doi:10.1001/jama.2022.15106



There are no comments for this article.