Background and Objectives: Family medicine has experienced wide variation in the proportion of allopathic medical students it attracts, ranging from a high of 16.8% to a low of 6.8%. We sought to measure the changes in specialty choice between the start of medical school and graduation.
Methods: We compared the specialty choice reported on the American Association of Medical Colleges annual allopathic Matriculating Student Questionnaire (MSQ) from 2014 to 2017 with the Graduation Questionnaire (GQ) from 2018 to 2021.
Results: Among 55,635 students who completed both the MSQ and the GQ, more than 70% changed their specialty choice between matriculation and graduation. Just 45% of students who reported family medicine at matriculation chose family medicine at graduation. However, 70% of students entering family medicine at graduation had selected some other specialty at the start of medical school. This increase of more than 3,000 students who made their family medicine specialty choice during medical school represents a net gain of nearly 1,000 students entering family medicine over the 4 years.
Conclusions: Most allopathic medical students change their specialty choice during medical school. The historic concern about students being talked out of family medicine during medical school is still partially valid, yet the data reported here show that the majority of students entering family medicine at graduation had reported a different specialty when they entered medical school. While increasing family medicine recruitment into medical school is crucial, these data also show the critical importance of family medicine departments helping recruit and support medical students’ family medicine choice during medical school.
Family medicine has experienced wide variation in the proportion of medical students it attracts into the specialty, with a high of 16.8% of graduating allopathic students in 1998 to a low of 6.8% in 2009. 1-3 Over the past 10 years, we have seen a modest increase in allopathic medical school graduates entering family medicine, from 6.8% to 8.1%. When combined with a higher percentage of osteopathic graduates and international graduates, the overall number of graduates entering family medicine residency in 2024 reached an all-time high of 4,595. 4, 5 Despite modest gains, the United States still needs more family doctors, along with other primary care clinicians. Many reasons for students not choosing family medicine have been proposed: 6, 7 who gets into medical school 8, massive medical school debt, 9 lower family physician income, 10, 11 and the unsupportive culture of medical schools for family medicine. 12-14
Growing out of the Family Medicine for America’s Health initiative, the leading organizations in family medicine proposed an ambitious effort to increase medical student interest in family medicine. 15 The 25 × 2030 Campaign aims to have 25% of medical school graduates entering a family medicine residency program by 2030. 16
Each year the American Association of Medical Colleges (AAMC) surveys incoming medical students 17 and graduates. 18 The matriculation survey includes the students’ planned specialty choice; the graduation survey includes their final specialty choice. 19-21 The purpose of this paper is to compare specialty choice at matriculation with specialty choice at graduation.
We compared the results of the AAMC annual Matriculating Student Questionnaire (MSQ) from 2014 to 2017 with the Graduation Questionnaire (GQ) from 2018 to 2021. 18 These survey years were chosen to ascertain the final specialty choice for the cohort of students who entered medical school from 2014 to 2017. The annual survey response rates ranged from 65% to 83% during this time. We obtained de-identified data from AAMC that included intended specialty choice on the MSQ and final specialty choice on the GQ. We included only those respondents who completed both the MSQ and the GQ; however, response rates for each question on the extensive surveys also varied. Not every respondent answered the questions about specialty choice. While both the MSQ and GQ are extensive surveys, not every survey question is answered. For privacy, security, and cost reasons, no other survey data were available for comparative analysis.
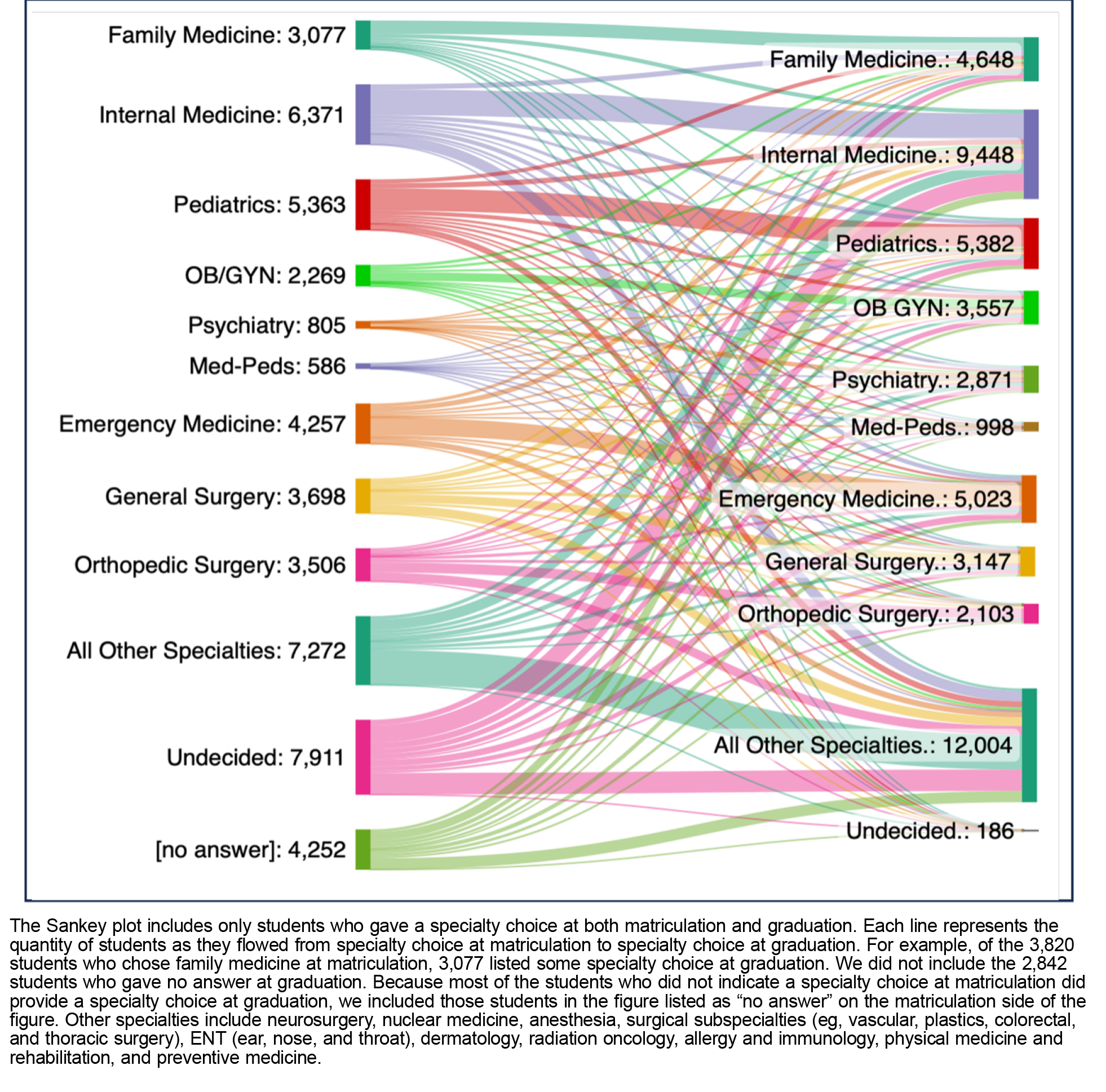
We measured the total number and proportion of survey respondents who selected each specialty at matriculation and graduation. To measure the proportion of students who maintained the same specialty choice from matriculation to graduation, we calculated the number of respondents who chose a specialty at matriculation divided by the number who chose the same specialty at graduation. We calculated the proportion of respondents choosing each specialty at matriculation and what their final specialty was at graduation. We used a Sankey plot to visualize the flow of specialty choice from matriculation to graduation across all specialties, where the width of the line is proportional to the quantity of students it represents.
The overall data included 70,828 students who completed the MSQ and 55,635 who also completed the GQ. At matriculation, 6,917 gave no answer to the question of specialty choice, and 10,775 answered “undecided.” At graduation, only 192 reported they were undecided, and 2,842 did not answer the question of specialty choice. After excluding those that gave no answer to the question of specialty choice, the final sample included matriculation specialty choice for 63,911 respondents, including the 10,775 who answered “undecided,” and graduation specialty choice for 52,793, of whom only 192 reported “undecided.” Table 1 presents matriculation and graduation specialty choice for selected specialties.
|
Specialty
|
Matriculating Student Questionnaire 2014–2017
|
Graduation Questionnaire 2018–2021
|
Percent change between MSQ and GQ (%)
|
|
Dermatology
|
1,545
|
1,128 ↓
|
27 ↓
|
|
Emergency medicine
|
5,419
|
5,142 ↓
|
5 ↓
|
|
Family medicine
|
3,820
|
↑ 4,759
|
↑ 25
|
|
Internal medicine
|
8,648
|
↑ 9,852
|
↑ 14
|
|
Neurosurgery
|
1,500
|
559 ↓
|
63 ↓
|
|
Neurology
|
2,385
|
1,408 ↓
|
41 ↓
|
|
Ob/Gyn
|
2,898
|
↑ 3,671
|
↑ 27
|
|
Ophthalmology
|
1,153
|
1,141 ↓
|
1 ↓
|
|
Orthopedics
|
4,773
|
2,170 ↓
|
55 ↓
|
|
Pathology
|
445
|
↑ 513
|
↑ 15
|
|
Pediatrics
|
6,756
|
5,534 ↓
|
18 ↓
|
|
General surgery
|
5,223
|
3,339 ↓
|
36 ↓
|
|
Anesthesia
|
1,323
|
↑ 3,087
|
↑ 233
|
|
Psychiatry
|
1,169
|
↑ 2,949
|
↑ 252
|
|
Radiology
|
966
|
↑ 2,209
|
↑ 229
|
|
Urology
|
295
|
↑ 901
|
↑ 305
|
|
Med-Peds
|
808
|
↑ 1,026
|
↑ 27
|
|
Undecided
|
10,775
|
192 ↓
|
98 ↓
|
|
No answer
|
6,917
|
2,842 ↓
|
95 ↓
|
At matriculation, 3,820 respondents reported their choice of specialty as family medicine, of which 3,077 also answered the graduation survey. Of the 3,077, just 1,396 chose family medicine at graduation (45%). Table 2 provides the change from family medicine to other specialties at graduation and the change from other specialties at matriculation to family medicine at graduation. Family medicine had a net gain at graduation from most of the specialties selected at matriculation. That is, more students switched from these specialty choices to family medicine from matriculation to graduation than switched from family medicine to these specialty choices. Family medicine had a net loss to several specialties, however. More students switched from family medicine at matriculation to Med-Peds (internal medicine and pediatrics), radiology, psychiatry, and anesthesiology at graduation than switched to family medicine from these specialty choices.
|
Specialty
|
Switched from family medicine to this specialty
|
Switched to family medicine from this specialty
|
|
Net increase into family medicine from:
|
|
|
|
Dermatology
|
27
|
67
|
|
Emergency medicine
|
160
|
330
|
|
Internal medicine
|
440
|
537
|
|
Neurosurgery
|
1
|
18
|
|
Neurology
|
41
|
72
|
|
Ob/Gyn
|
172
|
300
|
|
Ophthalmology
|
15
|
32
|
|
Orthopedics
|
18
|
166
|
|
ENT
|
13
|
21
|
|
Pathology
|
19
|
26
|
|
Pediatrics
|
274
|
415
|
|
General surgery
|
74
|
178
|
|
Undecided
|
4
|
569
|
|
Net decrease from family medicine into:
|
|
|
|
Anesthesia
|
67
|
43
|
|
Psychiatry
|
162
|
53
|
|
Radiology
|
41
|
29
|
|
Urology
|
7
|
5
|
|
Med-Peds
|
109
|
65
|
|
Total
|
1,640
|
2,926
|
At graduation, 4,759 respondents reported their choice of specialty as family medicine. While 45% of those choosing family medicine when they entered medical school ultimately chose family medicine at graduation, hundreds of medical students switched their specialty choice to family medicine during medical school. In fact, 70% of students who reported family medicine as their specialty choice at graduation had selected a different specialty or were undecided when they entered medical school. We identified a net gain to family medicine of 939 students (3,820 at MSQ to 4,759 at GQ) during the 4 years included in this analysis.
We found that the 4-year totals for family medicine, internal medicine, and emergency medicine from the AAMC data were about 73% to 80% of the totals reported by the National Resident Matching Program for the same time period. 22 This is consistent with the AAMC report on 65% to 80% completion rates. We found minimal variation in survey completion rates and agreement between AAMC data and Match data (family medicine 75%, pediatrics 80%, internal medicine 73%, emergency medicine 77%).
Other specialties experienced similar trends, with a few variations. Figure 1 provides a visual description of change in specialty choice from matriculation to graduation for the nine most frequently selected specialties. The specialty with the highest percentage choosing the same specialty at matriculation and graduation was psychiatry, at 59%. Table 3 shows this fidelity to matriculation specialty choice for the nine specialties with the highest concordance from matriculation to graduation. Several specialties that had the largest drop between matriculation and graduation include general surgery, dermatology, and ENT, with more than 80% switching to another specialty; 95% of those who had initially selected Med-Peds switched to another specialty.
|
Specialty choice at matriculation
|
Percent choosing same specialty at graduation (%)
|
|
Psychiatry
|
59
|
|
Family medicine
|
45
|
|
Emergency medicine
|
44
|
|
Pediatrics
|
43
|
|
Internal medicine
|
43
|
|
Obstetrics/gynecology
|
40
|
|
Orthopedic surgery
|
30
|
|
Surgery
|
24
|
The majority of allopathic medical students who match in family medicine have made that choice during medical school. This analysis shows that more than 70% of graduating medical students who reported they were entering family medicine residency had selected a different specialty when they first entered medical school. In fact, most students end up choosing their specialty during medical school, with dramatic changes from matriculation to graduation. 23 Family medicine has a relatively high level of fidelity from matriculation to graduation of 45%, second only to psychiatry at 59%.
Something happens during medical school that helps students refine their specialty choice. While the family medicine specialty choice decreased by more than 2,000 students during the 4 years in this analysis, it increased by more than 3,000 students. We hypothesize that family medicine predoctoral programs have an important role in recruiting students into family medicine. The conventional wisdom that students entering medical school with plans to go into family medicine change their mind is partially true. 7, 24 The hidden curriculum that denigrates family medicine is still present. 25, 26 This analysis confirms that more than half of students entering medical school who reported a plan to enter family medicine switched to another specialty. Every specialty loses students during medical school. Apparently, about two-thirds of students cannot predict their specialty choice the summer before they enter medical school. But that’s only half the picture.
The data also show that many students change their choice to family medicine during medical school, resulting in a net gain into family medicine. Family medicine experienced a net gain from most of the other specialties, even from the common primary care specialties such as internal medicine, pediatrics, and obstetrics/gynecology. Predoctoral programs, family medicine rotations, and other personal or clinical experiences in medical school impact final specialty choice. 27, 28 We may have an opportunity to expand this impact, encouraging even more students to enter family medicine. 29, 30 Though whether the specialty can meet the goal of 25 × 2030 is uncertain, 31 we appear to have an opportunity to combine our efforts to increase the number of students interested in family medicine at matriculation; coupling these efforts with ongoing support for family medicine predoctoral programs and experiences will help family medicine get closer to the 25 × 2030 goal.
Only a few specialties had a net gain from family medicine, such as psychiatry and Med-Peds; these gains were relatively small. While specialty choice changed from family medicine to Med-Peds for slightly more than 100 students, the vast majority of students selecting Med-Peds had selected some other specialty at the start of medical school. And more than 60 students switched from Med-Peds to family medicine. For some specialties, perhaps the requirements and rigor limit who can end up entering that specialty at graduation. For instance, while 1,500 students chose neurosurgery at matriculation, this highly competitive specialty had only 559 enter neurosurgery at graduation, likely due to the limited availability of neurosurgery residency spots.
Several limitations of this study should be considered. First, we included only those allopathic medical students who completed both the matriculation survey and the graduation survey. Respondents did not necessarily reply to every question, and we found a higher rate of not answering the specialty choice question on the graduation survey. Second, because the response rates for each survey ranged from 65% to 83%, our results probably account for only about half of all graduating medical students. However, that students choosing a particular specialty may have been more or less likely to complete the survey is doubtful; thus, that the results are biased toward or against any specific specialty is improbable. Finally, because these findings represent only allopathic medical students, we were unable to provide data on osteopathic medical student specialty choice. We are unaware of any comparable analysis on osteopathic students and feel that this might be an important addition to the research on the family medicine workforce.
While some students may take longer than 4 years to complete medical school, most medical students who entered medical school between 2014 and 2017 would have graduated and entered specialty training between 2018 and 2021. The AAMC graduation survey is available to all fourth-year medical students; it opens just prior to final specialty choice decisions required for the National Resident Matching Program. Inevitably, some students who hoped to choose a specialty completed the AAMC graduation survey and then changed their specialty choice at the last minute or failed to match in their chosen specialty. This uncommon occurrence likely did not impact our results.
Family medicine is still an attractive choice for medical students, with more than 800 students each year choosing family medicine over other specialties after entering medical school. This is good news for the hardworking family medicine faculty who teach and mentor medical students. Some students leave family medicine during medical school, but many more switch into family medicine. While increasing family medicine recruitment into medical school is crucial, these data also show the critical importance of family medicine departments helping recruit medical students into family medicine during medical school.
Presentations
A prior version of this study was presented at the North American Primary Care Research Group 2023 conference, San Francisco, CA.
Disclaimer
This material is based upon data provided by the Association of American Medical Colleges (AAMC). The views expressed herein are those of the authors and do not necessarily reflect the position or policy of the AAMC.
References
-
Rosser WW. The decline of family medicine as a career choice. CMAJ. 2002;166(11):1,419-1,420.
-
-
Byun H, Jabbarpour Y. Trends in the contribution of US medical schools to the family medicine workforce.
Ann Fam Med. 2023;21(suppl 3):5361.
doi:10.1370/afm.22.s1.5361
-
-
-
-
Phillips JP, Wendling AL, Prunuske J, et al. Medical school characteristics, policies, and practices that support primary care specialty choice: a scoping review of 5 decades of research.
Fam Med. 2022;54(7):542-554.
doi:10.22454/FamMed.2022.440132
-
Senf JH, Campos-Outcalt D, Kutob R. Factors related to the choice of family medicine: a reassessment and literature review.
J Am Board Fam Pract. 2003;16(6):502-512.
doi:10.3122/jabfm.16.6.502
-
Phillips JP, Petterson SM, Bazemore AW, Phillips RL. A retrospective analysis of the relationship between medical student debt and primary care practice in the United States.
Ann Fam Med. 2014;12(6):542-549.
doi:10.1370/afm.1697
-
Sanders K, Phillips J, Fleischer S, Peterson LE. Early-career compensation trends among family physicians.
J Am Board Fam Med. 2023;36(5):851-863.
doi:10.3122/jabfm.2023.230039R1
-
Phillips JP, Wilbanks DM, Rodriguez-Salinas DF, Doberneck DM. Specialty income and career decision making: a qualitative study of medical student perceptions.
Med Educ. 2019;53(6):593-604.
doi:10.1111/medu.13820
-
-
Reynolds L. Coping with family medicine put-downs. Can Fam Physician. 2005;51(8):1,081-1,082.
-
-
Kelly C, Coutinho AJ, Goldgar C, et al. Collaborating to achieve the optimal family medicine workforce.
Fam Med. 2019;51(2):149-158.
doi:10.22454/FamMed.2019.926312
-
Prunuske J. America needs more family doctors: the 25 x 2030 collaborative aims to get more medical students into family medicine. Am Fam Physician. 2020;101(2):82-83.
-
-
-
-
-
-
-
Ali S, Vines HD, Lensing SY, et al. Factors influencing the commitment of students to radiology as a career choice during medical school education.
Academic Radiology. 2021;28(8):1,174-1,178.
doi:10.1016/j.acra.2020.07.025
-
-
Mahood SC. Medical education: beware the hidden curriculum. Can Fam Physician. 2011;57(9):983-985.
-
-
-
-
Horrey K, Davidson C, Tan A. Twelve points to consider when talking to a medical student about a career in family medicine. Can Fam Physician. 2020;66(1):74-76.
-
Horrey K, Tan A. Selling family medicine: changing our message to medical students. Presented at Family Medicine Forum, November 2016, Vancouver, BC.
-
David AK. Matching 25% of medical students in family medicine by 2030: realistic or beyond our reach? Fam Med. 2021;53(4):252-255. doi:10.22454/FamMed.2021.982403



There are no comments for this article.