Background and Objectives: For years, family medicine has taught patient-centered communication through observations and observation checklists. We explored the utility of one checklist, the Patient-Centered Observation Form (PCOF), to teach and evaluate patient-centered communication in our family medicine residencies.
Methods: We conducted a mixed-method study of five University of Minnesota Family Medicine Residencies’ seven years of experience teaching and evaluating residents’ patient-centered communication skills. All programs have a behavioral health (BH) faculty-led observation curriculum that uses the PCOF to assess resident skills and give feedback. We conducted a BH faculty focus group and interviews, generated themes from the BH responses, and then queried family medicine (FM) faculty regarding these themes through an online survey.
Results: Ten BH faculty participated in the focus group/interviews, and 71% (25/35) of FM faculty completed the survey about themes derived from the BH interviews. The residencies complete between 1 to 11 observations per resident per year. Since implementation, four programs have continuously used the PCOF due to its versatility, design as a formative rather than summative feedback tool, and relative ease of use. BH faculty believe longitudinal observations with the PCOF resulted in improved resident patient-centered communication. Most importantly, all faculty described a shift in family medicine culture toward patient-centered communication. Time for observations and feedback is the primary curricular barrier.
Conclusions: Our findings support the utility of the PCOF for teaching and evaluating patient-centered communication in family medicine training.
In 2013, the medical specialties defined milestones residents should achieve to demonstrate competency. For the primary care specialties, those milestones include patient-centered communication behaviors. Therefore, the Accreditation Council on Graduate Medical Education (ACGME) strongly recommends faculty conduct observations of resident-patient interactions to assess resident milestone competency.1,2 Research supports the incorporation of direct observation to teach and assess learner competence in meeting patient communication skills.2-5 Family medicine has for many years prioritized resident observation as a tool to help teach patient-provider communication.6,7
Despite limited reliability data, the most commonly used observation tool for teaching patient-centered communication skills in family medicine is the Patient-Centered Observation Form (PCOF).7 The PCOF is a two-page checklist that breaks down the patient visit into well-defined components that are supported by measurable, discrete clinician behaviors.8-10
In 2009, the University of Minnesota Department of Family Medicine and Community Health (UMN-DFMCH) charged its residency programs to implement a patient-centered communication curriculum using the PCOF.8-10 Although the PCOF is one of the most commonly used forms used for assessing patient-centered communication, there is limited published data on how programs have implemented use of the PCOF and its impact on resident communication skills. We conducted a mixed-methods study aimed at characterizing the experiences of five residency programs over 7 years of PCOF implementation and use. Our goal was to explore the utility of the PCOF to teach and evaluate patient-centered communication in our family medicine programs.
The UMN-DFMCH is comprised of eight sponsored or affiliated family medicine residencies. Each residency has one or two behavioral health (BH) faculty.
The PCOF includes 12 skill sets of patient-centered communication behaviors starting with “establishes rapport” and ending with “closure.” Each skill is divided into observable elements and is organized as a checklist. The more boxes the observer checks, the more patient-centered the communication. During the study period, the newest version of the PCOF was utilized as it became available (http://courses.washington.edu/pove/files/PCOF_9_27_2013_clinician.pdf).
Phase 1: Behavioral HealthFaculty Focus Group/Interviews
Seven out of 10 behavioral health (BH) psychologist faculty from five of the UMN-DFMCH residencies participated in a 60-minute focus group exploring their experiences using the PCOF to evaluate and teach patient-centered communication. Participants were asked semistructured questions about the original implementation plan, current use of the PCOF, and successes and barriers in teaching patient-centered communication. The three remaining BH faculty had 30-45 minute phone interviews using the same questions. The focus group and phone interviews were audio recorded and transcribed verbatim. A single, trained investigator conducted the focus group and interviews. Phase 1 data analysis was informed by the social constructivist version of grounded theory (used when researchers have some a priori experience/knowledge in the qualitative question being asked).11 First, each investigator independently reviewed and coded the transcripts. After independent review, investigators then met and reached consensus about emerging themes through an iterative discussion process. Phase 1 BH interview and focus group themes informed development of the Phase 2 family medicine (FM) survey items.
Phase 2: Family Medicine Faculty Survey
Family medicine physician faculty from the five residency programs (n=35) subsequently completed a 21-item anonymous online survey (5-point Likert scale; strongly agree to strongly disagree) regarding experiences with the PCOF as a training tool. Items included FM faculty training on the PCOF, frequency of use, comfort using the PCOF, perceptions of utility/impact of the PCOF, and questions specific to the PCOF as a tool.
The University of Minnesota Institutional Review Board deemed this study exempt from review.
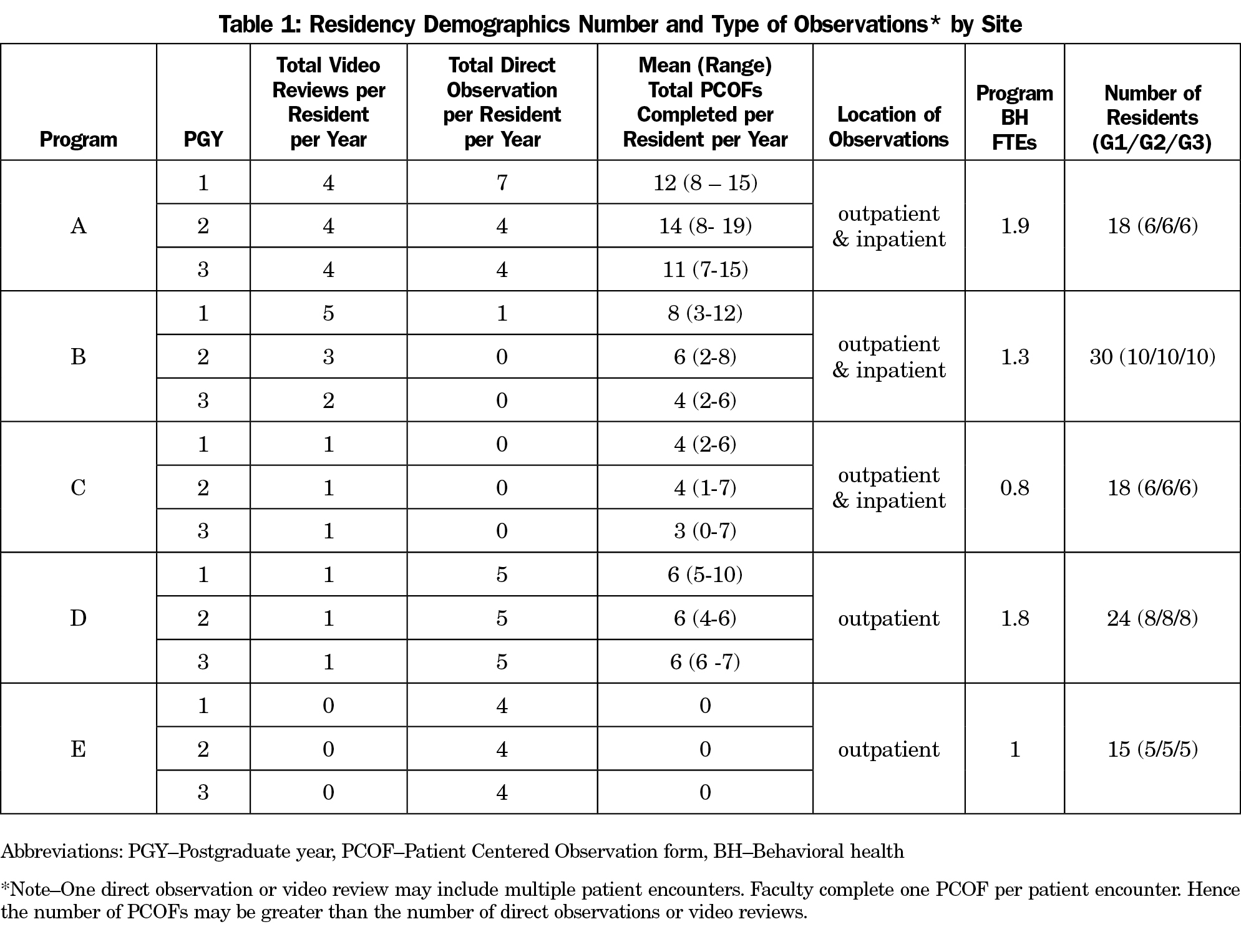
Table 1 describes the family medicine residency programs’ demographics and their use of the PCOF.
Family Medicine Faculty Survey Findings
Although, 71% (25/35) of the FM faculty completed the survey, only 80% (20/25) had actually completed a PCOF on a resident, usually through video review (72%) or direct observation in clinic (64%). Only 36% of the FM faculty had formal training on how to use the form. Despite the lack of training, 80% of faculty with PCOF experience were comfortable using the form to evaluate residents. Sixty-five percent believed the PCOF improved their effectiveness in teaching patient-centered communication. Twenty-two percent of FM faculty believed they were less competent in teaching patient-centered communication compared to BH faculty, 31% were not sure how they compared, and 47% believed they were as competent. Three themes emerged from Phase 1 and informed the Phase 2 survey: (1) a family medicine residency culture shift, (2) PCOF functionality, and (3) barriers to teaching patient-centered communication.
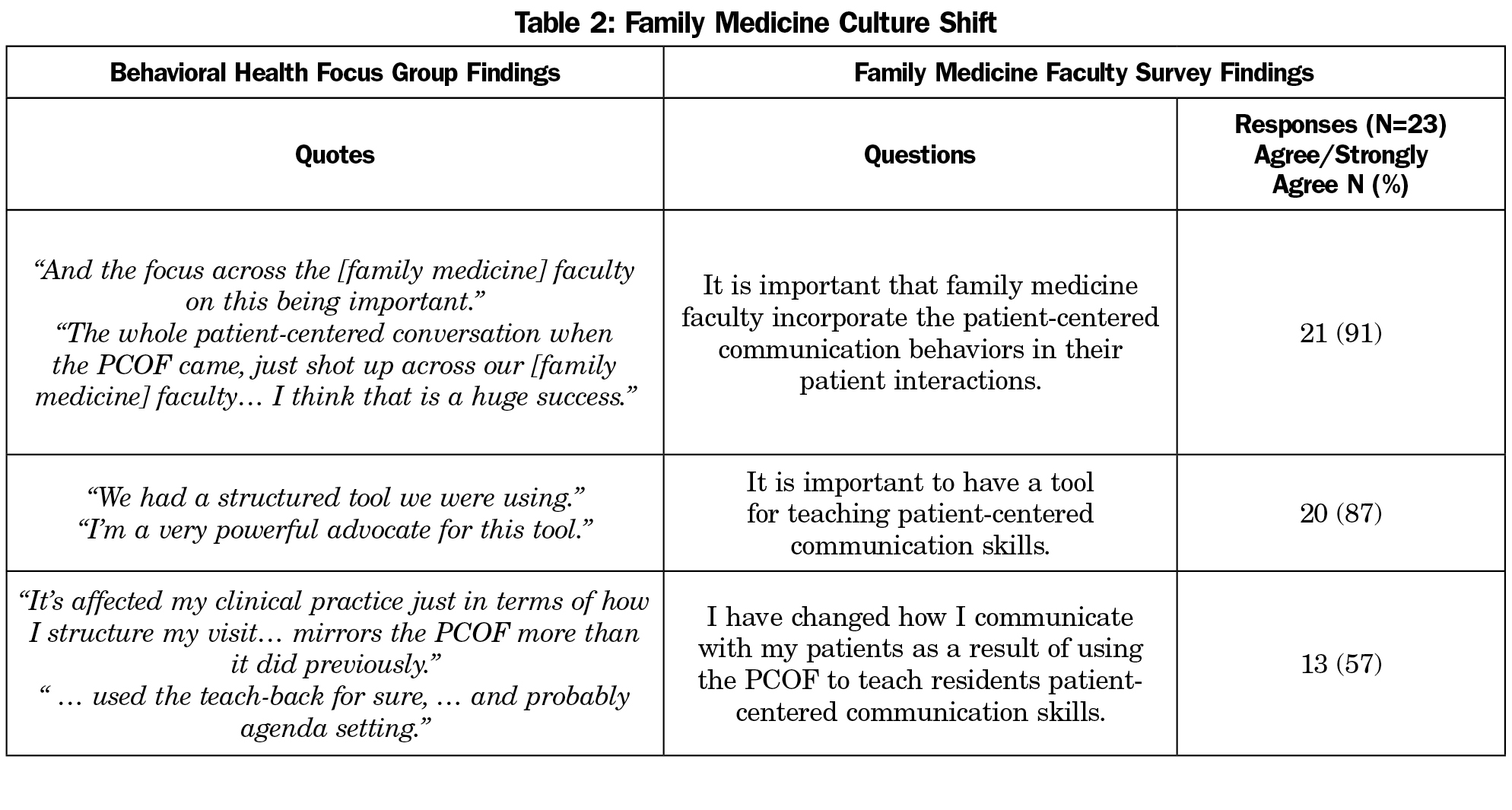
Theme 1: Family MedicineResidency Culture Shift
BH and FM faculty described a change in practice since PCOF implementation, evidenced by the adoption of a common language and faculty incorporation of the communication behaviors in direct patient care (Table 2). BH faculty hypothesized that this culture shift was enabled by a clear leadership directive for implementing a standardized patient-centered communication teaching tool, a required number of resident observations, and use of an evidence-based tool for evaluating and providing feedback. BH faculty reported improved resident patient-centered communication.
In terms of physician communication, I feel like, just observationally, they’re so much better than they used to be… I feel like the quality of the communication that I see in our resident physicians has improved over that time. (BH Focus Group)
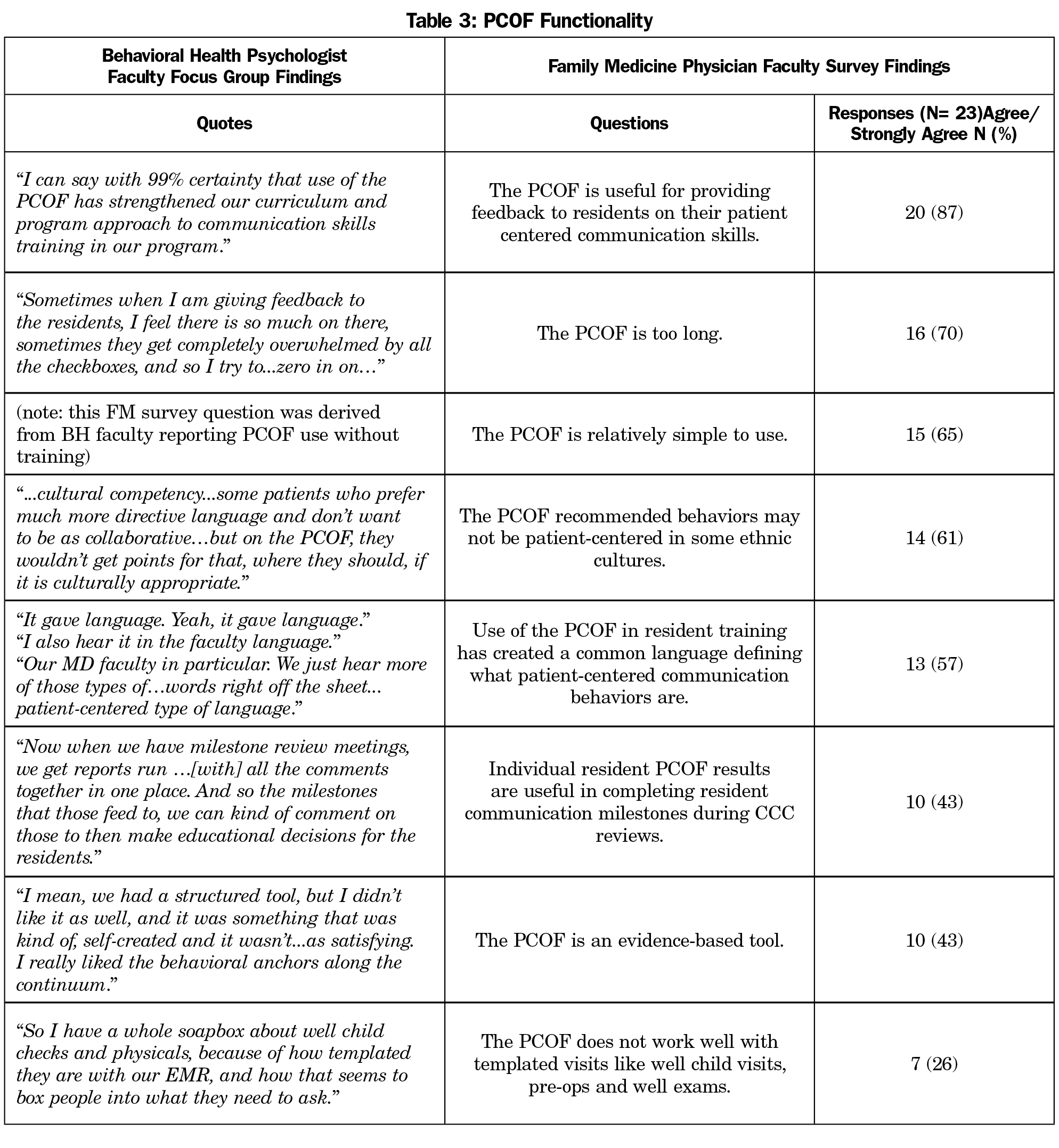
Theme 2: PCOF Functionality
BH and FM faculty agreed the PCOF is a useful, relatively easy tool to use, although it is lengthy and at times not culturally appropriate. FM and BH faculty opinions differed regarding tool functionality with the EHR, helpfulness for milestone competency assessment, and whether the tool is evidence-based (Table 3). BH faculty reported the PCOF helped learners and faculty identify specific patient communication issues and improve communication techniques while emphasizing growth along a continuum rather than a “grade.” By anchoring feedback to behaviors, BH faculty noted feedback is more specific and improvement becomes measurable.
BH faculty described the PCOF as adaptable to different curricular venues (live observations, video reviews, group reviews, self reviews) and goals (resident or program-directed). They recommended the PCOF be used longitudinally with incorporation into learner portfolios to track individual feedback and promote skill building over time. One BH participant noted the PCOF lacked advanced patient-centered communication behaviors, did not match milestones well, and was not flexible for all encounters (eg, basic medication recheck vs noncompliant patient with diabetes). Their program stopped using the PCOF and has developed their own checklist.
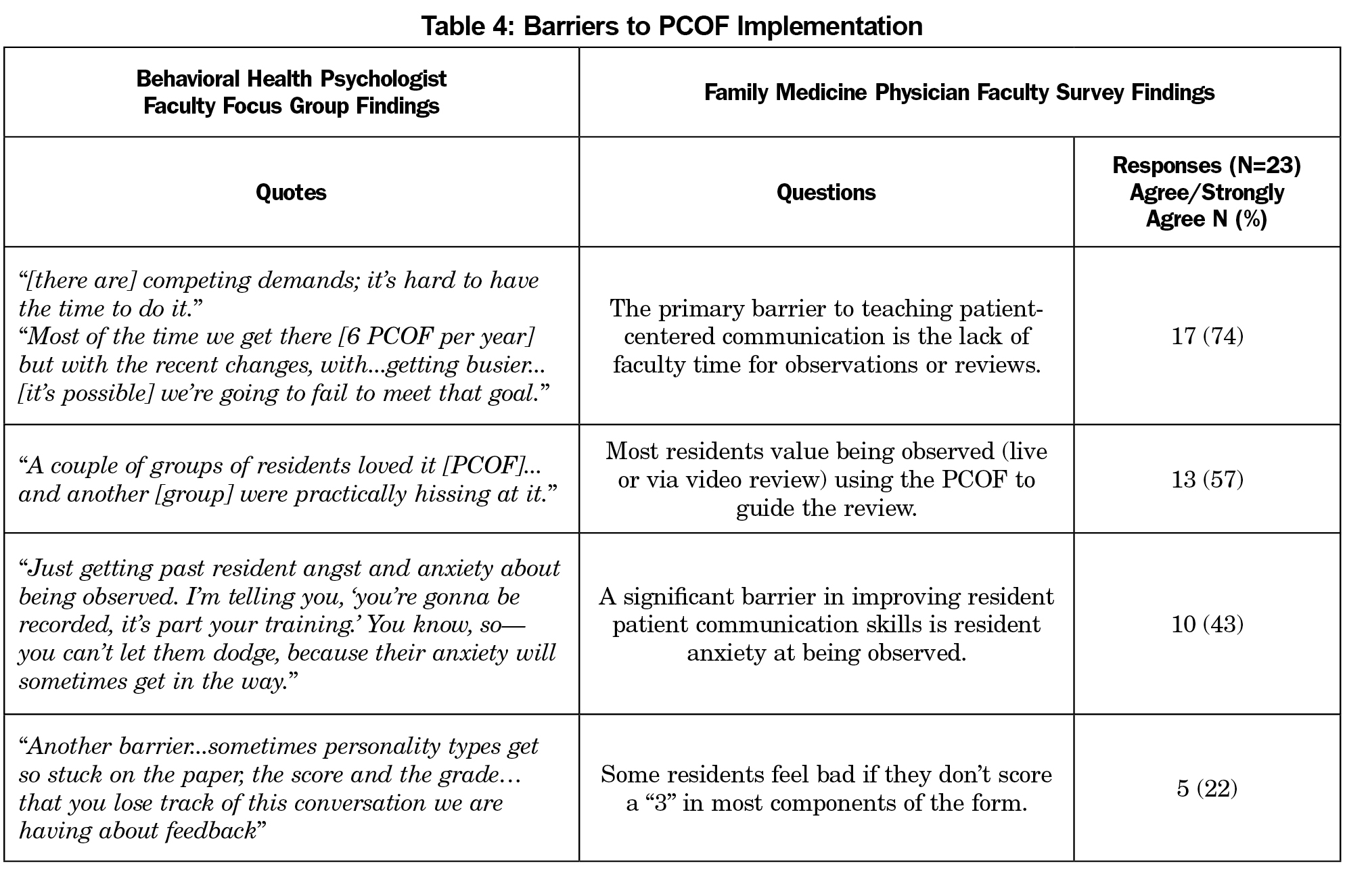
Theme 3: Barriers to PCOFImplementation
Barriers to PCOF implementation are listed in Table 4. Additional barriers noted by BH faculty included inconsistent faculty training and equipment/logistical barriers. They also noted residents earlier in training, whose priority is to “avoid killing their patient,” may not be developmentally ready for communication feedback.
Our findings support the utility of the PCOF for teaching and evaluating patient-centered communication in family medicine training. As we discovered, use of an appropriate,12,13 established tool consistently over an extended period of time2,14 is important. Since implementation in 2009, four of the five programs have continuously used the PCOF due to its versatility, design as a formative rather than summative feedback tool, and relative ease of use. Despite inconsistent training on the PCOF form, BH faculty believe longitudinal observations resulted in improved resident patient-centered communication, and FM faculty believe they are more effective teaching and comfortable evaluating patient-centered communication behaviors. Most importantly, faculty described a shift in family medicine residency culture toward patient-centered communication. As cited frequently in the literature, the primary barrier for PCOF implementation was time.2,3,5,7,12,15 The literature supports our findings of learner anxiety and grade focus over skill focus,3,9,16,17 along with the need for consistent faculty training2,8,9,16 as ongoing barriers.
Study strengths include the mixed-methods design and incorporation of both BH and FM faculty perspectives, perspectives that often concurred, thus reinforcing the findings.
This study was limited to five programs in one family medicine department, thus findings may not be generalizable.
Future research is needed to assess the long-term effect of patient-centered communication training on patient satisfaction and health outcomes.1,18
Acknowledgments
Prior Presentations: Best practice recommendations teaching residents patient-centered communication. Presented at Society of Teachers of Family Medicine Annual Spring Conference, Minneapolis, May 2, 2016.
References
- JR, Holmboe ES, Hauer KE. Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA. 2009;302(12):1316-1326.
https://doi.org/10.1001/jama.2009.1365.
- Hauer KE, Holmboe ES, Kogan JR. Twelve tips for implementing tools for direct observation of medical trainees’ clinical skills during patient encounters. Med Teach. 2011;33(1):27-33.
https://doi.org/10.3109/0142159X.2010.507710.
- Donato AA. Direct observation of residents: a model for an assessment system. Am J Med. 2014;127(5):455-460.
https://doi.org/10.1016/j.amjmed.2014.01.016.
- Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood). 2010;29(7):1310-1318.
https://doi.org/10.1377/hlthaff.2009.0450.
- Carr S. The Foundation Programme assessment tools: an opportunity to enhance feedback to trainees? Postgrad Med J. 2006;82(971):576-579.
https://doi.org/10.1136/pgmj.2005.042366.
- Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011;9(2):100-103.
https://doi.org/10.1370/afm.1239.
- Jansen KL, Rosenbaum ME. The state of communication education in family medicine residencies. Fam Med. 2016;48(6):445-451.
- Chesser A, Reyes J, Woods NK, Williams K, Kraft R. Reliability in patient-centered observations of family physicians. Fam Med. 2013;45(6):428-432.
- Ross V, Mauksch L, Huntington J, Beard JM. Interdisciplinary direct observation: impact on precepting, residents, and faculty. Fam Med. 2012;44(5):318-324.
- Keen M, Cawse-Lucas J, Carline J, Mauksch L. Using the Patient Centered Observation Form: evaluation of an online training program. Patient Educ Couns. 2015;98(6):753-761.
https://doi.org/10.1016/j.pec.2015.03.005.
- Charmaz K. Constructing grounded theory. 2nd ed. London, UK: Sage; 2014.
- Gigante J, Swan R. A simplified observation tool for residents in the outpatient clinic. J Grad Med Educ. 2010;2(1):108-110.
https://doi.org/10.4300/JGME-D-09-00090.1.
- King A, Hoppe RB. “Best practice” for patient-centered communication: a narrative review. J Grad Med Educ. 2013;5(3):385-393.
https://doi.org/10.4300/JGME-D-13-00072.1.
- Kogan JR, Holmboe ES, Hauer KE. Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA. 2009;302(12):1316-1326.
https://doi.org/10.1001/jama.2009.1365.
- Mahdi Hazavehei SM, Karimi Moonaghi H, Moeini B, Moghimbeigi A, Emadzadeh A. Investigating the key factors in designing a communication skills program for medical students: A qualitative study. Electron Physician. 2015;7(7):1441-1448.
https://doi.org/10.19082/1441.
- Edwards A, Tzelepis A, Klingbeil C, et al. Fifteen years of a videotape review program for internal medicine and medicine-pediatrics residents. Acad Med. 1996;71(7):744-748.
https://doi.org/10.1097/00001888-199607000-00006.
- Pelgrim EAM, Kramer AWM, Mokkink HGA, van der Vleuten CPM. The process of feedback in workplace-based assessment: organisation, delivery, continuity. Med Educ. 2012;46(6):604-612.
https://doi.org/10.1111/j.1365-2923.2012.04266.x.
- Hudon C, Fortin M, Haggerty JL, Lambert M, Poitras M-E. Measuring patients’ perceptions of patient-centered care: a systematic review of tools for family medicine. Ann Fam Med. 2011;9(2):155-164.
https://doi.org/10.1370/afm.1226.



There are no comments for this article.