Background and Objectives: Effective public provision of contraceptive services depends upon regular interventions at the primary care level. Recognizing the need to improve the frequency and quality of contraceptive counseling at a rural family medicine residency, this study sought to determine if the introduction of a simple teaching tool would lead to an increase in the rates of such counseling.
Methods: Resident physicians at a rural clinic provided contraceptive counseling to all eligible women, utilizing a simple educational table as a teaching aid. Rates of counseling were compared before, during, and after the intervention.
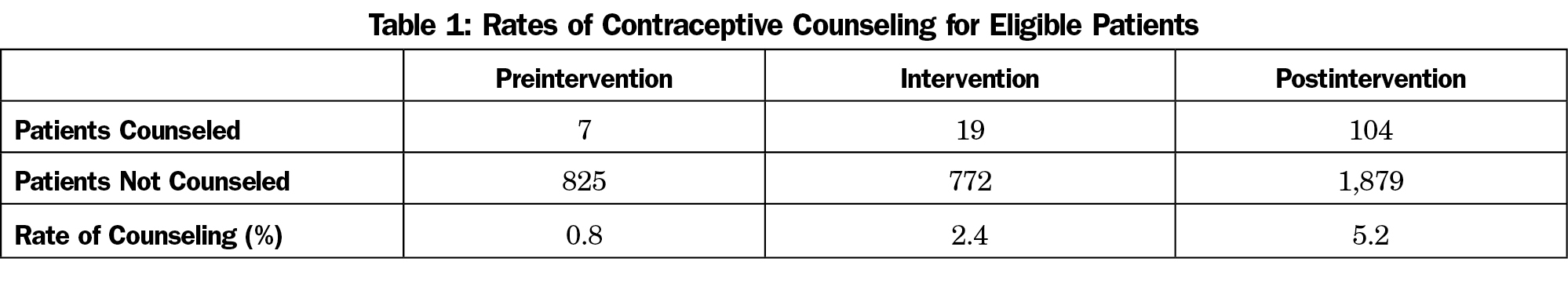
Results: A total of 3,606 patient encounters were included for analysis. Rates of contraceptive counseling in the preintervention period (n=832) and postintervention period (n=1,983) increased significantly (0.8% vs 5.2%, P<0.001). In addition, rates of counseling increased from the intervention phase (n=791) to the postintervention period (2.4% vs 5.2%, P<0.001).
Conclusion: The introduction of educational tools may increase rates of contraceptive counseling without being an undue burden upon providers.
Inadequate contraceptive services at the primary care level is a significant public health problem. Though the exact definition of “unplanned” pregnancies remains controversial and somewhat arbitrary, recent scholarship suggests that half of all pregnancies in the United States may fall into this category.1Unintended pregnancy has also been linked to domestic violence, and substance abuse.2,3 The need for efficacious and widely-available contraceptive education and treatment is clear.
Primary care providers (PCPs) play a key role in filling this need. Prior research has suggested a strong link between contraceptive counseling by PCPs and subsequent contraceptive utilization.4 Despite recommendations by the Centers for Disease Control for contraceptive counseling as a part of routine care, this service is frequently omitted.5 The rate of such contraceptive counseling in adolescents during general medical/physical exam visits is as low as 8% to 10%.6,7 In addition, previous research has found no increased rates of counseling to women prescribed category D or X medications.8
The etiology of this disparity between the need for and provision of contraceptive counseling is multifactorial. Providers frequently cite a lack of time, reimbursement, and training.9 Limited perceived need or interest from both providers and patients may further reduce the rate of counseling.10,11 Finally, there is inconsistent knowledge about contraceptive modalities among PCPs.11,12
Prospective research in the field of contraceptive counseling by PCPs remains limited. The aim of this quality improvement study was to determine if the implementation of a simple educational tool by residents at a family medicine clinic would increase the frequency of contraceptive counseling to women of reproductive age during annual exams.
Prior to initiating the study, the first author developed a table of nonpermanent forms of contraception, designed to be used by trainee residents for patient education during contraceptive counseling sessions. Approval for the study was obtained through the Institutional Review Board of Heritage Valley Health System. A rural ambulatory clinic at which residents were the primary providers was selected as the study site, and all 18 resident physicians agreed to participate. At the beginning of a 2-month intervention period, residents were educated on the importance of regular contraceptive counseling, about each of the contraceptive methods which their practice could offer, and specifically on the use of the contraceptive educational table. They were instructed to complete a checklist on all female patients presenting for their annual exam to determine eligibility for participation. Included in the study were women aged 18 to 49 who had not previously had a tubal ligation or hysterectomy, and who were not considering pregnancy within the following 12 months. If resident physicians felt counseling was warranted, and patients consented, a contraceptive counseling session was performed utilizing the above-mentioned table as an educational tool. Residents were also asked to document this encounter utilizing an appropriate ICD-10-CM diagnosis code.
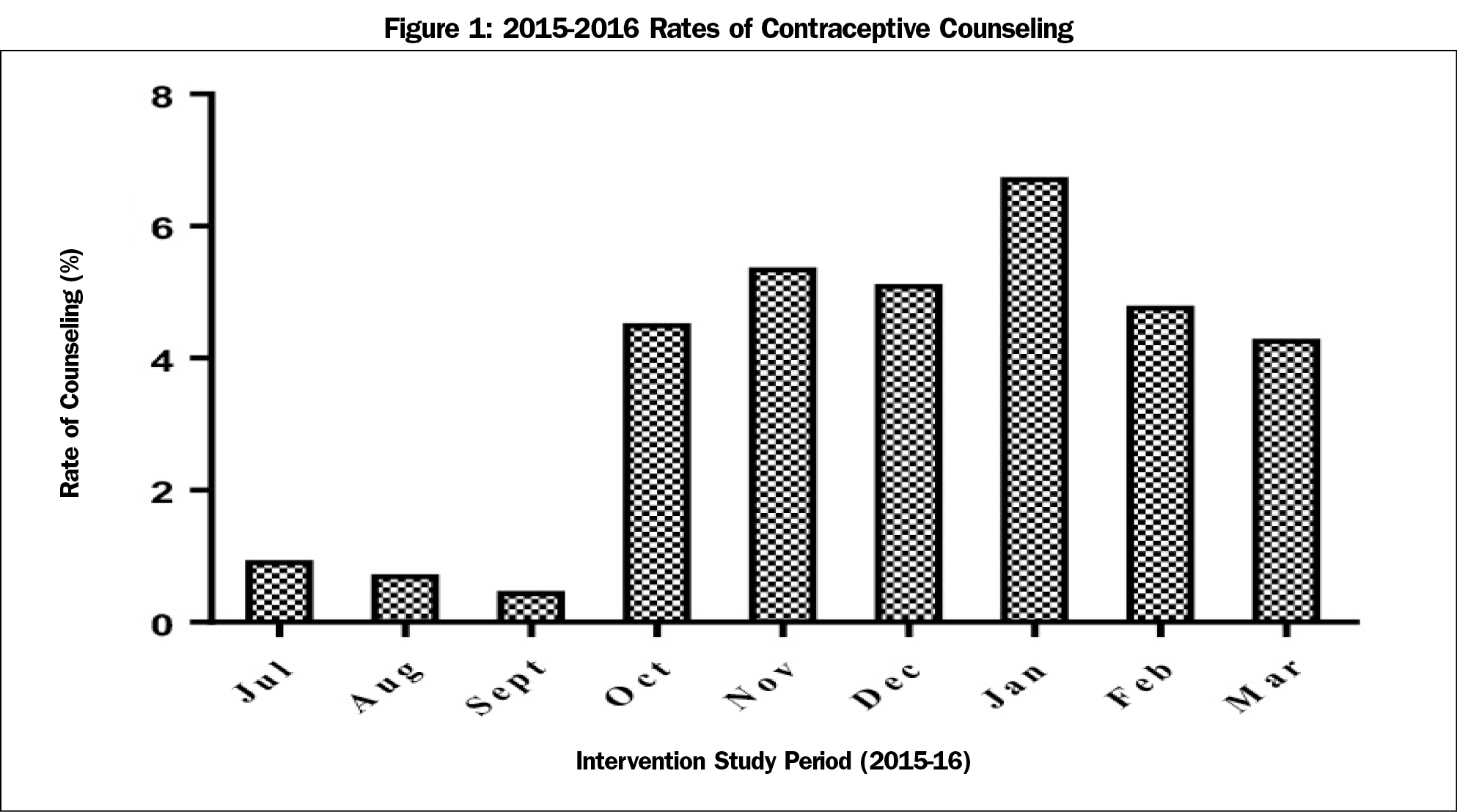
Rates of contraceptive counseling were documented for a preintervention period, intervention period, and postintervention period. The preintervention period (July through August, 2015) was designed to correspond with the first 2 months of the academic year, thus ensuring that the cohort of residents remained consistent throughout the study. The intervention period lasted from September to October, 2015. The postintervention period (November, 2015 through March, 2016) consisted of the 5 months following the intervention. Rates were determined by dividing the number of patient encounters in which an ICD-10 code corresponding with contraceptive counseling was documented by the number of eligible patient encounters. Rates of counseling were compared between the pre- and postintervention periods, the preintervention and intervention periods, and the intervention and postintervention periods, utilizing chi-square analyses, with two-sided P values of less than 0.05 representing statistically significantly results (GraphPad Prism 7.01, GraphPad Software Inc, La Jolla, CA).
Finally, at the end of the intervention period, residents were asked to provide subjective feedback on their experiences utilizing the educational tool in providing contraceptive counseling.
In the preintervention period, 0.8% of all eligible encounters included contraceptive counseling (Table 1). This rate increased in the intervention period to 2.4% (χ2=6.27, P=0.012). In the postintervention period, the rate of counseling (5.2%) remained elevated when compared to the preintervention period (χ2 =30.1, P<0.001). This trend continued throughout the postintervention period (Figure 1). There was also a significantly increased rate of counseling in the postintervention period when compared to the intervention period (χ2=10.78, P=0.001).
When asked to provide subjective, voluntary feedback on the intervention, resident physicians’ responses (which included 8 of 18 participants) were strongly positive. One reported that “the table made teaching medical students and patients much easier!” A second commented that the intervention made them “more eager to have contraceptive conversations with patients.”
This study was designed to determine if simple, standardized educational tools help facilitate contraceptive counseling between PCPs and their patients. There was a significant increase in the rates of counseling during the intervention period, when providers were required to complete checklists on their patients to determine study eligibility, and were actively encouraged to complete and document counseling sessions. Rates of counseling increased again in the postintervention phase, suggesting that at least some of the providers had incorporated counseling into their regular practice. Given that all participating physicians were trainees, these changes have the potential to impact their clinical behaviors throughout their career, incorporating contraceptive counseling as part of their armamentarium of preventive care. It should be noted, however, that while rates of counseling increased sixfold over the course of the study, in no month did it rise above 7% of eligible encounters. This low proportion would suggest considerable room for further improvement.
A number of limitations to this work should be noted. This was a single center study and did not include advanced practice providers or attending physicians. Patterns of contraceptive care following intervention were measured in the short and medium term, but not in the long term. In addition, billing data was used to calculate rates of contraceptive counseling, rather than direct provider-patient observation. Though the results of this study suggest that simple changes can make a significant impact on the rate of contraceptive counseling among primary care providers, further research in a variety of practice locations (urban, suburban, and rural) and settings (private practice in addition to academic), is necessary to determine if such interventions lead to measurable changes in the rates of contraceptive use. Moreover, further studies on the effects of such interventions on the incidence of unplanned pregnancy are needed.
For providers interested in increasing their provision of effective contraceptive counseling, a simplified version of the tool used in this intervention has been included as an appendix (https://www.stfm.org/Portals/49/Documents/FMAppendix/GoldsteinAppendix-2017.pdf). In addition, a review of effective counseling methods has been completed by Dehlendorf et al.13
Acknowledgments
The authors would like to acknowledge the help of Soo Lee, MD, and Jonathan McKrell, MD, who both assisted in developing the educational table used in this study, as well as Vikram Arora, MD, who assisted us in statistical analysis. Further, we would like to thank Roxanne Alsbury, MD; Sadia Parveen; MBBS; and Tetsuro Sakai, MD, PhD; for their critical reviews of the finished draft.
Presentations: This work was presented as a poster presentation at 2016 Family Medicine Educational Consortium Annual Meeting, Pittsburgh, PA, and at Family Medicine Residency Poster Day, Pittsburgh, PA, May 2016.
References
- Finer LB, Zolna MR. Declines in unintended pregnancy in the united states, 2008-2011. N Engl J Med. 2016;374(9):843-852.
https://doi.org/10.1056/NEJMsa1506575.
- Heil SH, Jones HE, Arria A, et al. Unintended pregnancy in opioid-abusing women. J Subst Abuse Treat. 2011;40(2):199-202.
https://doi.org/10.1016/j.jsat.2010.08.011.
- Centers for Disease Control and Prevention (CDC). Physical violence during the 12 months preceding childbirth--Alaska, Maine, Oklahoma, and West Virginia, 1990-1991. MMWR Morb Mortal Wkly Rep. 1994;43(8):132-137.
- Weisman CS, Maccannon DS, Henderson JT, Shortridge E, Orso CL. Contraceptive counseling in managed care: preventing unintended pregnancy in adults. Womens Health Issues. 2002;12(2):79-95.
https://doi.org/10.1016/S1049-3867(01)00147-5.
- Gavin L, Moskosky S, Carter M, et al; Centers for Disease Control and Prevention (CDC). Providing quality family planning services: Recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep. 2014;63(RR-04):1-54.
- Ma J, Wang Y, Stafford RSUS. U.S. adolescents receive suboptimal preventive counseling during ambulatory care. J Adolesc Health. 2005;36(5):441.
https://doi.org/10.1016/j.jadohealth.2004.08.024.
- Rand C, Auinger P, Klein J, Weitzman M. Preventive counseling at adolescent ambulatory visits. J Adolesc Health. 2005;37(2):87-93.
- Schwarz EB, Postlethwaite DA, Hung YY, Armstrong MA. Documentation of contraception and pregnancy when prescribing potentially teratogenic medications for reproductive-age women. Ann Intern Med. 2007;147(6):370-376.
https://doi.org/10.7326/0003-4819-147-6-200709180-00006.
- Petersen R, Payne P, Albright J, Holland H, Cabral R, Curtis KM. Applying motivational interviewing to contraceptive counseling: ESP for clinicians. Contraception. 2004;69(3):213-217.
https://doi.org/10.1016/j.contraception.2003.10.007.
- Chuang CH, Hwang SW, McCall-Hosenfeld JS, Rosenwasser L, Hillemeier MM, Weisman CS. Primary care physicians’ perceptions of barriers to preventive reproductive health care in rural communities. Perspect Sex Reprod Health. 2012;44(2):78-83.
https://doi.org/10.1363/4407812.
- Schreiber CA, Harwood BJ, Switzer GE, Creinin MD, Reeves MF, Ness RB. Training and attitudes about contraceptive management across primary care specialties: a survey of graduating residents. Contraception. 2006;73(6):618-622.
https://doi.org/10.1016/j.contraception.2006.01.014.
- Dehlendorf C, Levy K, Ruskin R, Steinauer J. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81(4):292-298.
https://doi.org/10.1016/j.contraception.2009.11.006.
- Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57(4):659-673.
https://doi.org/10.1097/GRF.0000000000000059.



There are no comments for this article.