Background and Objectives: National initiatives have encouraged oral health training for family physicians and other nondental providers for almost 2 decades. Our national survey assesses progress of family medicine residency programs on this important health topic since our last survey in 2011.
Methods: Family medicine residency program directors (PDs) completed an online survey covering various themes including number of hours of oral health (OH) teaching, topics covered, barriers, evaluation, positive influences, and program demographics.
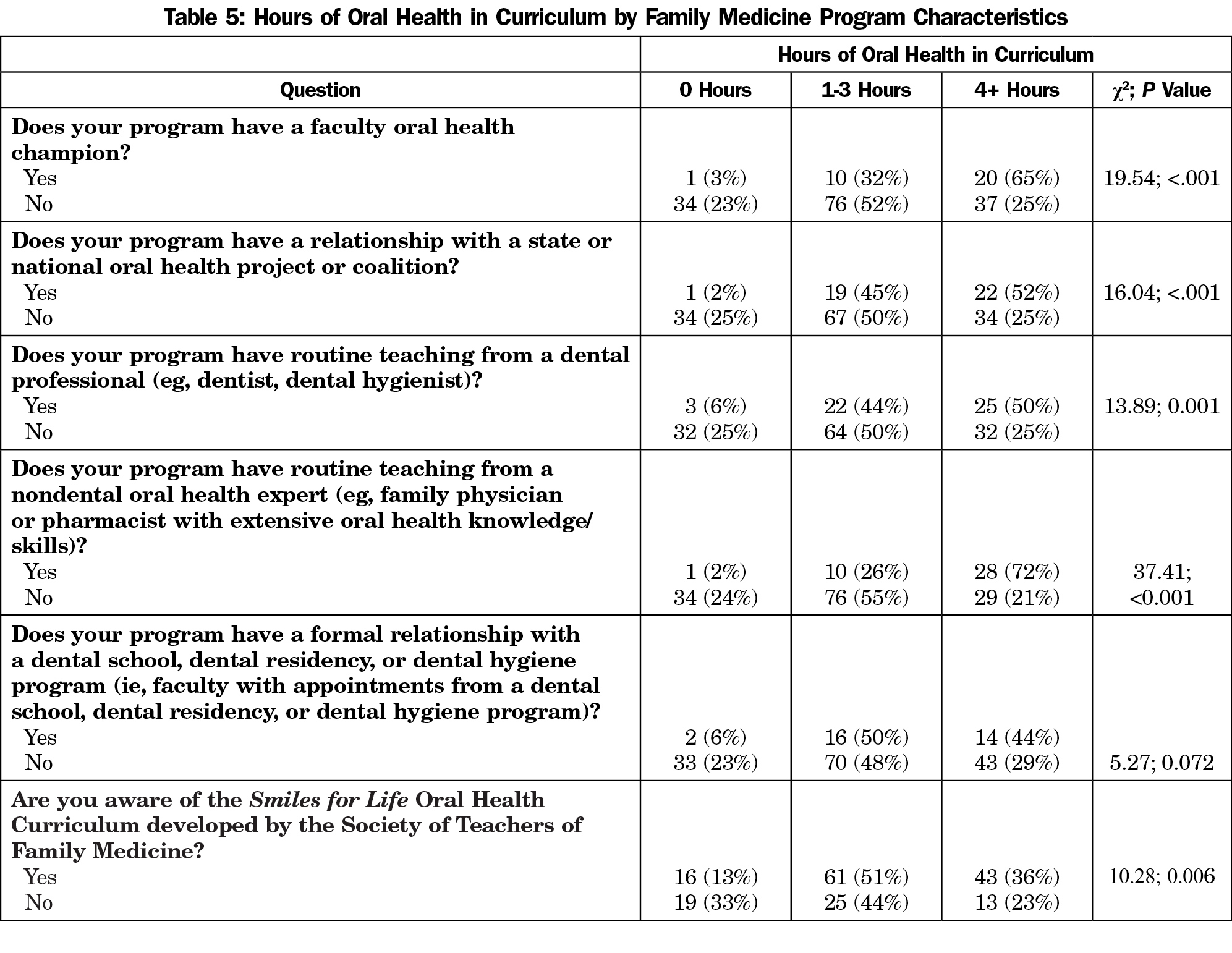
Results: Compared to 2011, more PDs feel OH should be addressed by physicians (86% in 2017 vs 79% in 2011), yet fewer programs are teaching OH (81% vs 96%) with fewer hours overall (31% vs 45% with 4 or more hours). Satisfaction with the competence of graduating residents in OH significantly decreased (17% in 2017 vs 32% in 2011). Program directors who report graduates being well prepared to answer board questions on oral health topics are more likely to have an oral health champion (P<0.001) and report satisfaction with the graduates’ level of oral health competency (P<0.001). Programs with an oral health champion, or having a relationship with a state or national oral health coalition, or having routine teaching from a dental professional are significantly more likely to have more hours of oral health curriculum (P<0.001).
Conclusions: Family medicine PDs are more aware of the importance of oral health, yet less oral health is being taught in residency programs. Developing more faculty oral health champions and connecting programs to dental faculty and coalitions may help reduce this educational void.
Oral health (OH) has received increased recognition for almost 2 decades as an important health topic. Dental caries cause local pain and infections, have important social implications such as missed school and failure to gain employment, and can even lead to death.1 In addition, periodontitis influences systemic illness such as heart disease, pregnancy outcomes, and autoimmune disorders.2 In fact, one study shows that dental treatment of periodontitis alone can reduce hospitalizations for diabetic patients by 39%.3
In 2000, the Surgeon General Report stimulated interest in oral health.4 David Satcher concluded with a clear statement, “You are not healthy without good oral health.” In 2003, another report, A National Call to Action to Promote Oral Health, encouraged physicians to address oral health in their patients.5 By 2005, family medicine program directors (PDs) were acknowledging the importance of OH. In a nationwide study, 95% felt it was their responsibility to train residents to identify oral health problems; 87% indicated they would implement modules if they existed, and a 4-hour curriculum was the average amount of time PDs felt their residents should devote to OH training.6 Also in 2005, family doctors formed a Group on Oral Health at the Society of Teachers of Family Medicine (STFM), and created a curriculum called Smiles for Life: A National Oral Health Curriculum funded by DentaQuest Foundation and others.7 In 2011, family medicine residency PDs were resurveyed. While only 72% of PDs now felt it was important to address OH issues, 96% of programs had some OH curriculum. And while only 45% had 3 or more hours of OH training, 74% were aware of Smiles for Life (SFL) and 22% were using it for teaching.8
Meanwhile, national oral health efforts continued to evolve. In 2011, the Institute of Medicine (IOM) issued two reports on this subject amplifying that nondental health professional training programs should have well-defined OH competencies and curricula.9,10 The Accreditation Council for Graduate Medical Education (ACGME) added oral health care requirements for family medicine in 2006 with the aim of promoting increased resident training in oral health11 (but by 2015, they removed them when streamlining requirements).12 Meanwhile, other specific movements have positively affected family medicine. Qualis Health made it a priority for OH to have a key role in medical homes and piloted systems approaches in Federally Qualified Health Centers (FQHCs).13,14,15 STFM added oral health topics in the Family Medicine Residency Curriculum Resource and the American Academy of Family Physicians created an Oral Health Member Interest Group.16,17 Finally, in 2014 the US Preventive Services Task Force (USPSTF) designated the application of fluoride varnish by medical providers a level B recommendation for children under the age of 6 years,18 which led to all 50 states reimbursing pediatric primary care providers to perform fluoride varnish.19
Our study assesses the impact over the last 5 years of the above-noted efforts and the influence on oral health care training in family medicine residency programs nationwide. We are unaware of any other studies of this impact over this time period. We aimed to learn what OH topics family medicine residency programs are currently teaching, how much they are teaching, how they evaluate this teaching, influences on the quality and quantity of curriculum, and resource materials being used. Our research is a project of the recently formed Center for Integration of Primary Care and Oral Health (CIPCOH), a joint endeavor of the Harvard Schools of Medicine and Dental Medicine and the University of Massachusetts Medical School’s Department of Family Medicine and Community Health.
Study Population
We developed and distributed electronically a 19-item survey to all 520 family medicine program directors (both allopathic and osteopathic) listed on the FREIDA website (the AMA Residency & Fellowship Database,20 accessed January 25, 2017). Efforts were made via web searches to update contact information for the PDs if the FREIDA database only included administrative support personnel. Program directors were encouraged to have a designee complete the survey (eg, associate PD/curriculum director) if they were likely to be more knowledgeable to answer questions about OH inclusion in residency training.
Data Collection
The present survey was based upon our previous 2011 survey (very similar questions, same use of FRIEDA) taking into account more recent, relevant published literature.8,21,22 Our survey included 13 questions about oral health training (eg, hours and days of training, curricular topics), the presence of dental professionals in teaching curricular components, the awareness and use of educational resources (eg, SFL oral health curriculum), barriers to the inclusion of OH curriculum, evaluation methods of learners regarding OH competence, attitudes toward the integration of oral health and primary care, and satisfaction with learners’ competence in OH. These 13 questions were either multiple choice, yes/no, or Likert-scaled; five had opportunities for free text. Next, five demographic questions asked about program location, size of community served, number of residents trained per year, length of tenure as a residency training site, and current position of person completing the survey. One final question asked respondents who self-identify as a “best practice” residency training program in OH curriculum about their willingness for us to contact them for an in-depth, phone-based interview to gather data for phase two of our study (the results of these interviews are not reported in this paper). Total estimated completion time was 15 minutes maximum. The survey was reviewed and edited by a panel of national health experts with oral health interests. We piloted the survey with five family medicine residency faculty (former PDs) and edited for final distribution based on their feedback.
Using a web-based survey development and data collection software application (SurveyMonkey, Inc, Palo Alto, CA) with accepted online survey methodology strategies,23 an initial electronic cover letter describing the study’s purpose, its voluntary nature, and respondent anonymity was emailed to potential respondents a week in advance of the survey’s distribution. The survey was fielded between February and June of 2017. Three reminders were sent at 3-week intervals (based on Dillman’s Total Design Method).24 In an effort to increase our response rate, the PI sent a personal email reminder or had a fellow OH expert colleague send a personal email to all nonresponders encouraging their participation. The study was approved by the University of Massachusetts Medical School Institutional Review Board and received an exemption waiver.
Data Analysis
Data were analyzed using SPSS statistical software (SPSS V23, IBM Corporation, 2015). Univariate statistics (frequencies, percentages, means, and other measures of central tendency) were used to describe all survey items. Based on the categorical or continuous nature of the study variables (using chi-square tests and t-tests, as appropriate), relationships were examined using an alpha of .05 to denote statistical significance. The Likert-scaled responses (1=“strongly disagree” to 5=“strongly agree”) were dichotomized for bivariate analyses to “strongly agree/agree” versus “neutral/disagree/strongly disagree.” Our objectives for subanalysis included assessing relationships that influenced OH in the curriculum including, but not limited to, the influence of having a faculty oral health champion, residency program demographics, and the number of hours of oral health education. Finally, tests of proportions were used to assess changes between our 2011 and 2017 survey results.
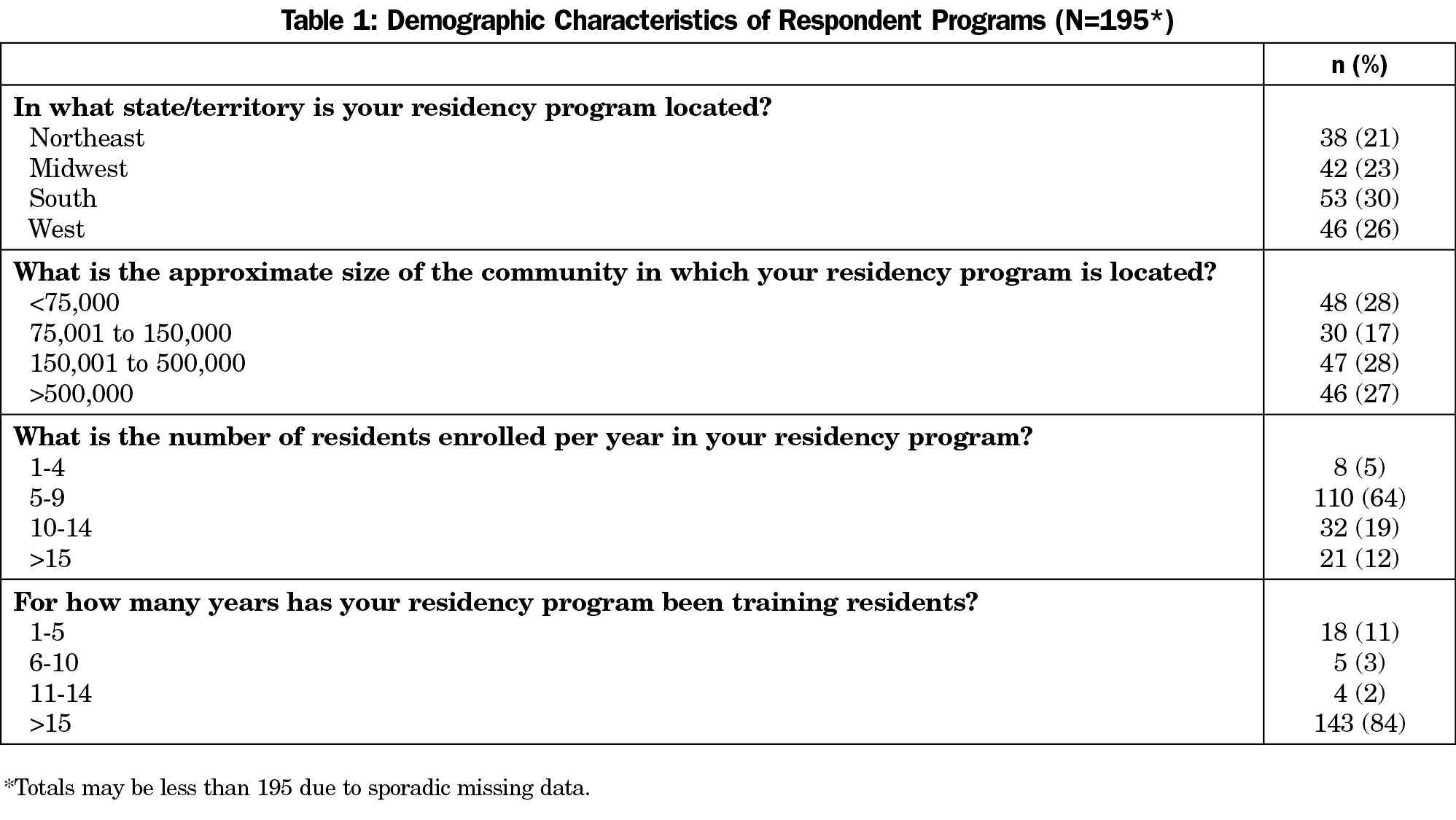
Of the initial sample of 520 PDs, 195 responded to at least one question. Thirty-eight PDs were excluded either because their email address was nondeliverable or the program responded that they did not have residents matriculating at the time of the survey. The 195 respondents represent 40% of the eligible 482 PDs. Characteristics of the region of the country, size of community served, program size, and program longevity are shown in Table 1.
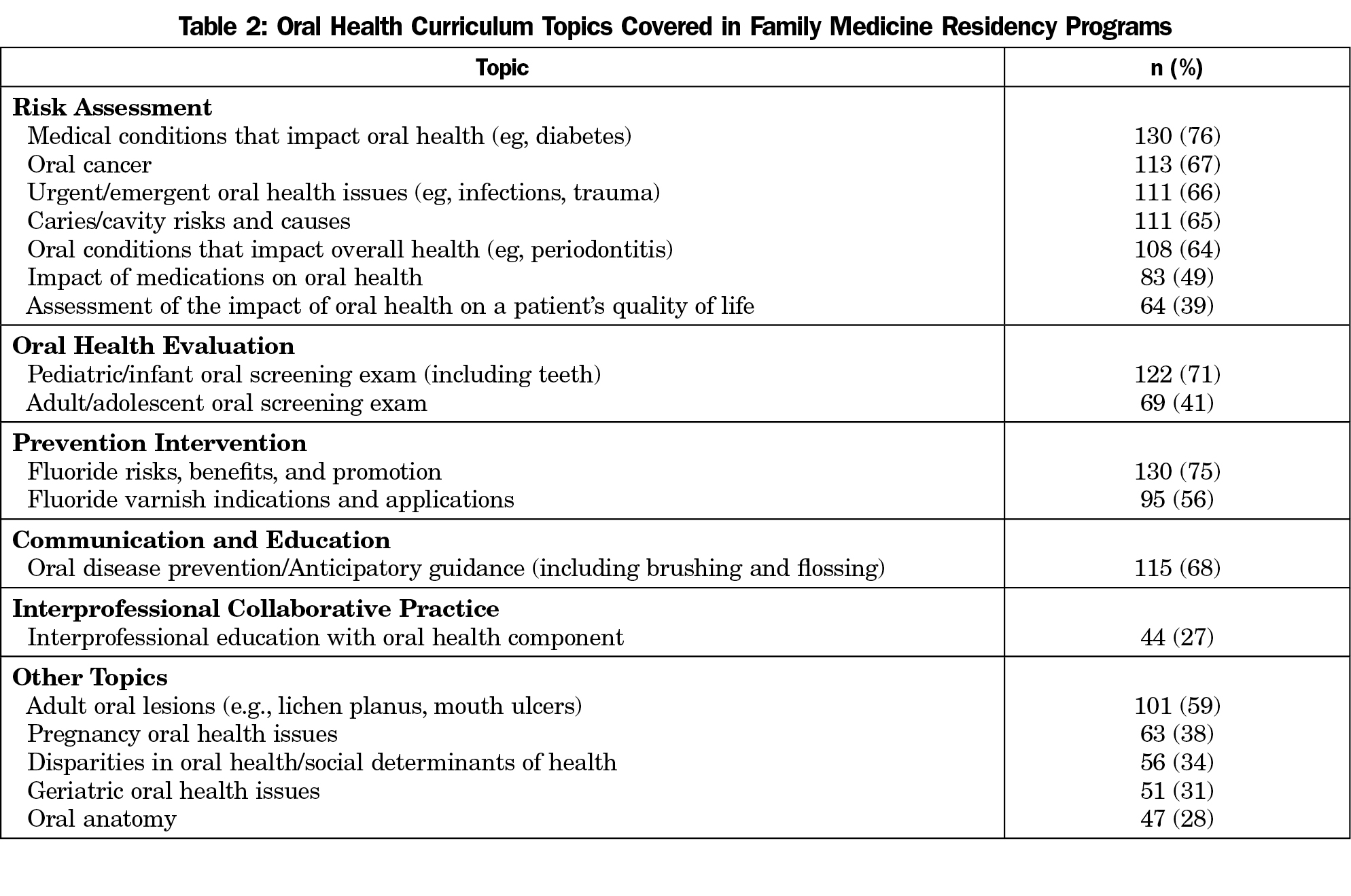
Almost one-fifth (19%) of responding PDs report 0 hours of OH curriculum, with 51% reporting 1-3 hours and 31% reporting 4 or more hours spent on this topic. The most prevalent topics covered include: medical conditions that impact oral health (76%); fluoride—risks, benefits and promotion (75%); and the infant/pediatric oral health screening exam (71%, Table 2). Interprofessional OH is the topic least addressed (27%). Only one-fifth (20%) of responding programs have residents spend any time in dental settings, down from 27% in 2011. While the majority (56%) of programs reported teaching their residents about indications of fluoride varnish, less than half (42%) require them to apply varnish in the clinical setting.
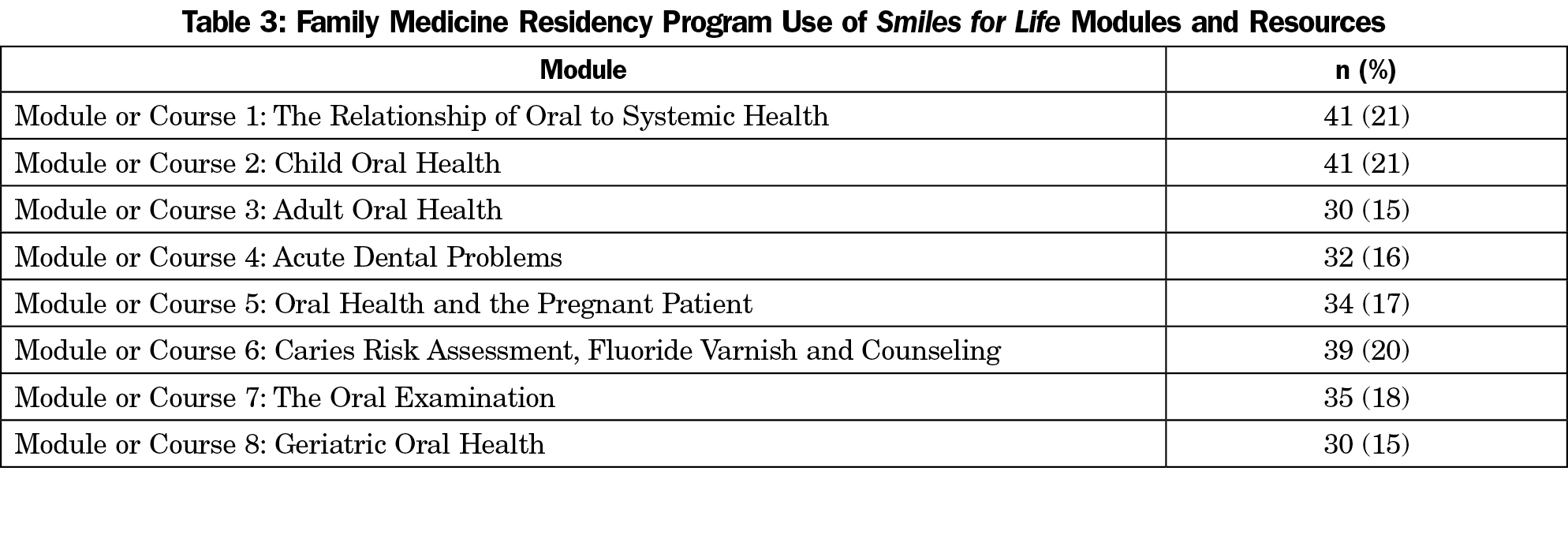
Regarding specific OH curricula, 68% of responders are aware of STFM’s SFL program, but only one-fifth (21%) of all PDs reported using any of the SFL modules. This finding is similar to our 2011 survey. Programs vary in their use of these eight modules (Table 3). The SFL downloadable app and prepared test questions are used by only 3% of programs (data not shown). There is a fairly even split in how SFL resources are used, with 15% of programs having residents complete the modules online individually versus 17% downloading the modules for faculty to give as a lecture. Programs that reported awareness of SFL are significantly more likely to have 4 or more OH hours in their curriculum (36% vs 23%; P=0.006). The most frequently used external curricula after SFL are OH articles from American Family Physician (13%) and the American Academy of Family Physician FP Essentials on Oral Health (10%).
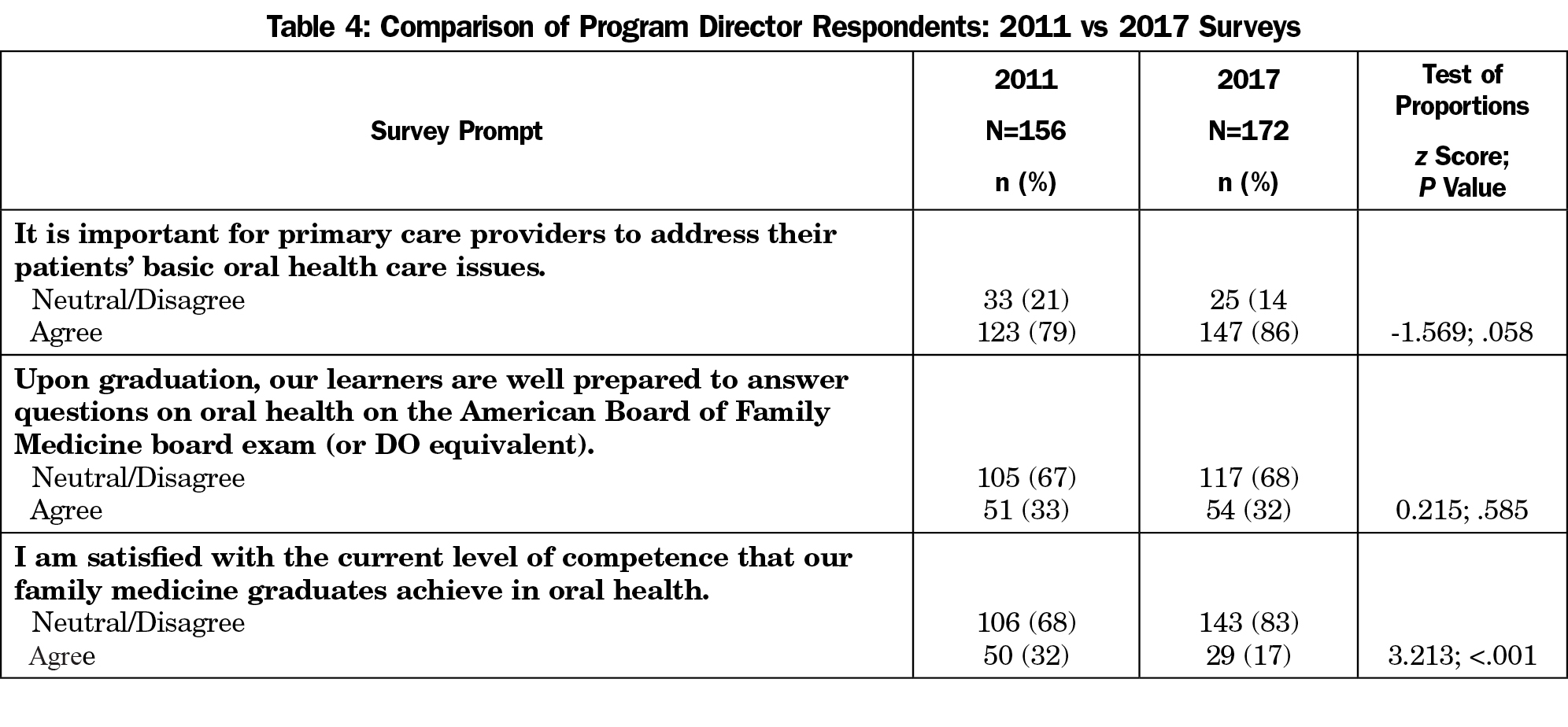
Compared to our 2011 survey, more responding PDs reported feeling oral health should be addressed by physicians (P=.058, Table 4). About the same percentage of PDs agree that their residents are well prepared to answer American Board of Family Medicine questions on oral health (P=.585); however, responding PDs reported being significantly much less satisfied with the competence of their residents in OH (17% in 2017 vs 32% in 2011 P<.001).
In terms of influences on OH curriculum, less than one-fifth (18%) of responding programs reported having a formal relationship with a dental school, dental residency or dental hygiene program. Despite this lack of a formal relationship, 28% have routine teaching from a dental professional (similar to 2011 at 32%). Only one-quarter (24%) of responding PDs noted having a relationship with a state or national OH project or coalition. While less than one in five (17%) responding programs reported having an OH champion, more than double that number (43%) agreed or strongly agreed there is support within their department for integrating oral health into primary care training.
Programs that do have an OH champion are significantly more likely to have more hours of oral health curriculum (65% with 4 or more hours had a champion vs 25% with no champion; P<0.001, Table 5). This is also true for responding programs that have a relationship with a state or national oral health project or coalition (52% with 4 or more hours vs 25%; P<0.001) and routine teaching from a dental professional (50% vs 25% with 4 or more hours; P<0.001). Notably, having a formal relationship with a dental school, residency or dental hygiene program is not significantly related to hours of OH training (Table 5). Demographic variables are also not significant when assessing relationships to the number of OH hours taught, including program size, geographic location, program longevity, or size of community (data not shown).
Responding programs that reported graduates being well prepared to answer board questions on oral health topics are more likely (39% vs 8%) to have an OH champion (P<0.001), as are those reporting satisfaction with level of graduates’ OH competency (55% vs 10%; P<0.001). Programs in the northeast are significantly more likely to have an OH champion (Northeast 38%, Midwest 10%, South 8%, West 19%; P=0.001) but other demographic characteristics (ie, program size, longevity, and size of community) had no similar significant effect.
The most common barrier to oral health curricular coverage is competing priorities/lack of time (75%) followed by lack of faculty expertise (54%). Prevalence of these barriers is similar to our 2011 findings: competing priorities (85%), lack of time (69%), and lack of faculty expertise (52%). Lack of faculty interest decreased from 35% in 2011 to 19% in 2017. The most common barrier, competing priorities, is not significantly related to the total hours of OH teaching (30% reported this was a barrier among programs with 4 or more hours of OH teaching vs 32% not teaching at this level of commitment; P=0.795). A few PDs free-texted a wide range of other barriers, such as “I can’t even find a dentist to take care of my patients, trying to find one to teach my residents for free is like trying to find a unicorn,” and “Given how many other health issues for which we are responsible, why not leave this area to dentists?”
It is reassuring that the vast majority of responding family medicine PDs feel it is important for their specialty to address oral health issues. On the other hand, it is concerning that one-fifth of responding programs still have no oral health curriculum, and that the number of OH teaching hours has decreased over the past half-decade. This has taken place during the same time frame that the ACGME cut oral health as a requirement in family medicine. PDs may have a similar level of confidence in their graduates to answer board questions on oral health when compared to 2011; however, their satisfaction with the level of OH competency among their trainees of less than 20% demands attention. Family medicine training should focus on having all residencies include at least a few hours of oral health training. This may require a reinstatement of the ACGME requirement. Internally, an organization like STFM or the Association of Family Medicine Residency Directors should strongly consider defining oral health competencies for family medicine graduates to encourage efficient curricula that focus on high-yield, practical clinical skills.
There has been more than a fourfold increase in responding programs routinely having residents apply varnish clinically (9% in 2011 vs 42% in 2017). This is likely a result of the USPSTF designating fluoride varnish application by medical providers as a level B recommendation for young children and all 50 states reimbursing for the procedure; however, with less than 50% of programs offering this proven intervention, a more aggressive approach is needed around training. By comparison, a recent study with pediatric residencies shows that nearly two-thirds (63%) of pediatric and Med-Peds programs are routinely having their residents offer fluoride varnish to their patients.25
A blueprint is needed to enhance the oral health training of family medicine residents. Addressing barriers is a practical place to start. Increasing faculty interest and expertise, promoting the SFL curriculum, and increasing the number of total hours of OH training can act as strategic targets for these efforts. Furthermore, promotion of practical tools like the downloadable app and prepared test questions within SFL would help learners better address oral health in clinical settings and increase the extremely low evaluation rates. However, awareness of curricula and resources is not enough. Strategies are needed to improve implementation and maintenance. As with all efforts, there are “carrots and sticks.” ACGME requirements and defined oral health competencies, as stated above, are only part of the solution; there are other key factors.
Faculty need to be continuously engaged in the importance of oral health. Continued efforts at keeping the importance of OH visible to faculty through articles in American Family Physician, AAFP News, Family Medicine, as well as teaching conferences and other venues may help give oral health primacy and improve its position as a priority. Making it clear, for example, that for 2 to 5-year-olds, there is only one other nondental recommendation from the USPSTF (checking vision once) besides offering fluoride supplementation and applying fluoride varnish, may help family doctors realize what they are not doing. If the few open-ended comments we received in the survey are indicative of the mindset of PDs in family medicine, we need more enlightenment and also more access to resources in the form of dental teachers.
Connections need to be made with local dental professionals to establish more formal teaching relationships since this has not improved since 2011. The American Dental Association and the Academy of General Dentistry are interested in such partnerships, and the American Dental Education Association has expressed interest in more interprofessional education than in the past.26 There is also a need to train in-house faculty as oral health champions since they have profound effects on oral health hours and outcomes. This is a clear role for STFM and the SFL team. Efforts should include preconferences at the STFM Annual Meeting, webinar trainings through the Oral Health Collaborative, and visiting professor programs to get residencies up to speed. This will require financial support, something that has waned for family medicine in the last half decade. Financial capital can be stretched by pairing residencies to state oral health coalitions and initiatives, something that successful programs are already doing.
We acknowledge three limitations of our study. First, the survey was answered by the program director in most cases, and the PD may not have full knowledge of the OH curriculum within the program. Second, our response rate, while adequate for medical personnel surveys, may not be indicative of all family medicine residency programs. As we allowed participants to remain anonymous and did not ask for specific program affiliation, we were unable to compare our sample to nonresponders, further limiting the generalizability of our study. Third, our survey is based on self-report and not a formal review of the curriculum or the residents’ actual knowledge and skills. We propose that in the future, a more objective review of oral health curricula in family medicine residencies be conducted.
In summary, having an OH champion and creating connections with dental faculty has significant effects on the PDs’ perception of graduates’ abilities to address oral health board questions and clinical situations. Future efforts may need to further assess the Northeast programs to see why and how they are more likely to have an oral health champion. The AAP has deliberately and systematically created a state OH champion in all 50 states27; family medicine should replicate this model as a first step toward universal family medicine oral health champions. The AAP has also invited dental faculty onto their committees, something that family medicine should duplicate.
Acknowledgments
This project was supported by Health Resource and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant number UH1P29962, titled “Academic Units for Primary Care Training and Enhancement.” This information content and conclusions are those of the authors and should not be construed as the official policy nor position of, nor should any endorsement be inferred by HRSA, HHS, or the US Government.
References
- Guarnizo-Herreño CC, Wehby GL. Children’s dental health, school performance, and psychosocial well-being. J Pediatr. 2012;161(6):1153-1159. https://doi.org/10.1016/j.jpeds.2012.05.025.
- Arigbede AO, Babatope BO, Bamidele MK. Periodontitis and systemic diseases: A literature review. J Indian Soc Periodontol. 2012;16(4):487-491. https://doi.org/10.4103/0972-124X.106878.
- Jeffcoat MK, Jeffcoat RL, Gladowski P, Bramson JB, Blum JJ. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am J Prev Med. 2014; 47(2):166-174.
- US Department of Health and Human Services. Oral health in America: A report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health, 2000. www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/Documents/hck1ocv.@www.surgeon.fullrpt.pdf. Accessed January 4, 2018.
- US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institutes of Health, National Institute of Dental and Craniofacial Research. NIH Publication No. 03-5303, May 2003.
- Gonsalves WC, Skelton J, Heaton L, Smith T, Feretti G, Hardison JD. Family medicine residency directors’ knowledge and attitudes about pediatric oral health education for residents. J Dent Educ. 2005;69(4):446-452.
- Clark MB, Douglass AB, Maier R, et al. Smiles for Life: A National Oral Health Curriculum. 3rd ed. Society of Teachers of Family Medicine; 2010. www.smilesforlifeoralhealth.com. Accessed January 4, 2018.
- Silk H, King R, Bennett IM, Chessman AW, Savageau JA. Assessing oral health curriculum in US family medicine residency programs: a CERA study. Fam Med. 2012;44(10):719-722.
- Institute of Medicine. Advancing oral health in America. Washington, DC: The National Academies Press; 2011. www.nap.edu/openbook.php. Accessed January 4, 2018.
- Institute of Medicine and National Research Council. Improving Access to Oral Health Care for Vulnerable and Underserved Patients. Washington, DC: The National Academies Press, 2011. www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2011/Improving-Access-to-Oral-Health-Care-for-Vulnerable-and-Underserved-Populations/oralhealthaccess2011reportbrief.pdf. Accessed January 4, 2018.
- Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in family medicine. (5) (d) Surgical subspecialties. 2007:27. IV.A.5.b).
- Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in family medicine. 2017. www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_family_medicine_2017-07-01.pdf. Accessed January 4, 2018.
- Qualis Health. Oral health integration in the patient-centered medical home (PCMH) environment. Case studies from community health centers. Sept 10, 2012. www.qualishealth.org/sites/default/files/white-paper-oral-health-integration-pcmh.pdf. Accessed January 4, 2018.
- Qualis Health. Oral health: An essential component of primary care. Case examples. June 2015. www.niioh.org/sites/default/files/Oral_Health_white_paper_case_examples.pdf. Accessed January 4, 2018.
- Hummel J, Phillips KA, Holt B, Virden M. Safety Net Medical Home Initiative. Organized, evidence-based care supplement: Oral health integration. Seattle, WA: Qualis; 2016. http://practicetransformation.qualishealth.org/sites/default/files/practicetransformation.qualishealth.org/Executive-Summary-Oral-Health-Integration.pdf. Accessed January 4, 2018.
- Society of Teachers of Family Medicine, Association of Family Medicine Residency Directors. Family Medicine Residency Resource Curriculum. www.fammedrcr.com. Accessed January 4, 2018.
- American Academy of Family Physicians. Oral Health Member Interest Group www.aafp.org/membership/involve/mig/oral-health.html. Accessed January 4, 2018.
- US Preventive Services Task Force. Final Update Summary: Dental Caries in Children from Birth Through Age 5 Years: Screening. September 2016. www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/dental-caries-in-children-from-birth-through-age-5-years-screening. Accessed January 4, 2018.
- American Academy of Pediatrics. Oral Health Initiative. www.aap.org/oralhealth. Accessed January 4, 2018.
- American Medical Association. Residency and Fellowship Database. www.ama-assn.org/life-career/search-ama-residency-fellowship-database. Accessed January 4, 2018.
- Curtis M, Silk HJ, Savageau JA. Prenatal oral health education in U.S. dental schools and obstetrics and gynecology residencies. J Dent Educ. 2013;77(11):1461-1468.
- Langelier MH, Glicken AD, Surdu S. Adoption of oral health curriculum by physician assistant education programs in 2014. J Physician Assist Educ. 2015;26(2):60-69. https://doi.org/10.1097/JPA.0000000000000024.
- Sue VM, Ritter LA. Conducting Online Surveys. Thousand Oaks, CA: Sage Publications, Inc; 2007. https://doi.org/10.4135/9781412983754.
- Dillman DA. Mail and Internet Surveys: The Tailored Design Method. New York, NY: John Wiley & Sons, Inc; 2007.
- Isong I, Silk H, Savageau J. A national survey of oral health curricula in pediatric residency programs. Poster presented at: Annual Meeting of the American Academy of Pediatrics; Sept 16-19, 2017; Chicago, IL.
- American Association of Colleges of Nursing, American Association of Colleges of Osteopathic Medicine, American Association of Colleges of Pharmacy, American Dental Education Association, Association of American Medical Colleges, and Association of Schools of Public Health. Core Competencies for Interprofessional Collaborative Practice. 2011. https://www.aamc.org/download/186750/data/core_competencies.pdf. Accessed January 4, 2018.
- American Academy of Pediatrics. AAP Section on Oral Health State Information and Resource Map. www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Oral-Health/Map/Pages/State-Information-and-Resources-Map.aspx. Accessed January 4, 2018.



There are no comments for this article.