Background and Objectives: Dementia often goes undiagnosed. A workshop was developed to provide primary care clinicians with a structured clinical reasoning approach to dementia diagnosis and brain map tool to differentiate type of dementia. The purpose of this study was to examine the impact of this approach on self-perceived changes in knowledge, confidence, and ability to assess and manage memory problems and on self-reported application of learning to clinical practice.
Methods: Participants of 20 workshops (N=392) were invited to complete a reaction survey and of these, participants of 12 consecutive workshops (N=242) were invited to complete a 3-month follow-up survey to assess application of new learning to clinical practice and challenges experienced in doing so.
Results: In total, 355 reaction and 108 follow-up surveys were completed. Mean ratings of usefulness reflected that participants considered the clinical reasoning approach and brain map very useful to learning and knowledge transfer. At follow-up, the majority of respondents reported they were more confident (79%) and better able to assess (79%) persons with cognitive impairment and more confident (88%) and better able to manage (86%) persons with cognitive impairment. A number of practice changes and challenges were identified.
Conclusions: These results add to a growing literature on strategies to improve dementia care with effective continuing medical education. A structured clinical reasoning approach to cognitive impairment is effective in improving confidence and ability to assess and manage patients with cognitive impairment, although participants continue to experience challenges in managing this complex condition.
Diagnostic uncertainty and the complexity of care required for patients with dementia remain considerable barriers to the early diagnosis and optimal management of dementia in primary care.1,2 As many as two-thirds of persons in the community with dementia remain undiagnosed3; the global prevalence rate of undiagnosed dementia has been estimated to be 61%.4 Delayed diagnosis results in a higher burden of suffering, excessive emergency department (ED) visits and hospitalizations, higher rates of care in hospitals while waiting for more appropriate alternate levels of care (ALC), premature institutionalization, and higher avoidable health care costs.5,6 Early detection of dementia has many benefits, including earlier initiation of treatment for persons with dementia and their caregivers, education, counseling, and other services that can delay decline, prevent crises (including preventing ED use), ease caregiver burden, and reduction of the heavy societal costs associated with hospitalizations and long-term institutionalization7,8 Currently, there is a heavy reliance on specialist physicians for the diagnosis and management of dementia, with as many as 80% of patients with dementia being referred to specialists.9 Yet Canada faces a critical shortage of specialists,10 and wait times to access specialist care can be lengthy,11 further impeding early diagnosis and intervention.
Delayed and missed diagnosis of dementia has been attributed in part to inadequate physician knowledge and lack of relevant training.1,3 Studies have also found that physicians have difficulty differentiating types of dementia,12 lack knowledge of early signs and symptoms of cognitive impairment,13 and lack confidence in their diagnostic skills.14,15 They may perceive that specialists are most appropriate for making dementia diagnoses,3,15 yet national consensus guidelines have recommended that the diagnosis and management of patients with dementia should largely be the responsibility of primary care.16 Enhanced training in clinical assessment and access to diagnostic tools have been identified as critical to improving the diagnosis of dementia.1,3,15
To build capacity for dementia care, a continuing medical education (CME) workshop was developed by family physicians for family physicians with the support of the Ontario College of Family Physicians, Canada. The workshop was adapted from the curriculum of a comprehensive 5-day interprofessional training program designed to develop primary care-based collaborative memory clinics.17 Building on the knowledge and resources created as a result of the memory clinic training program, the 3-hour CME workshop was developed to build capacity for dementia care among family physicians working in practice settings that do not have a memory clinic to which they can refer patients.
CME Workshop Curriculum
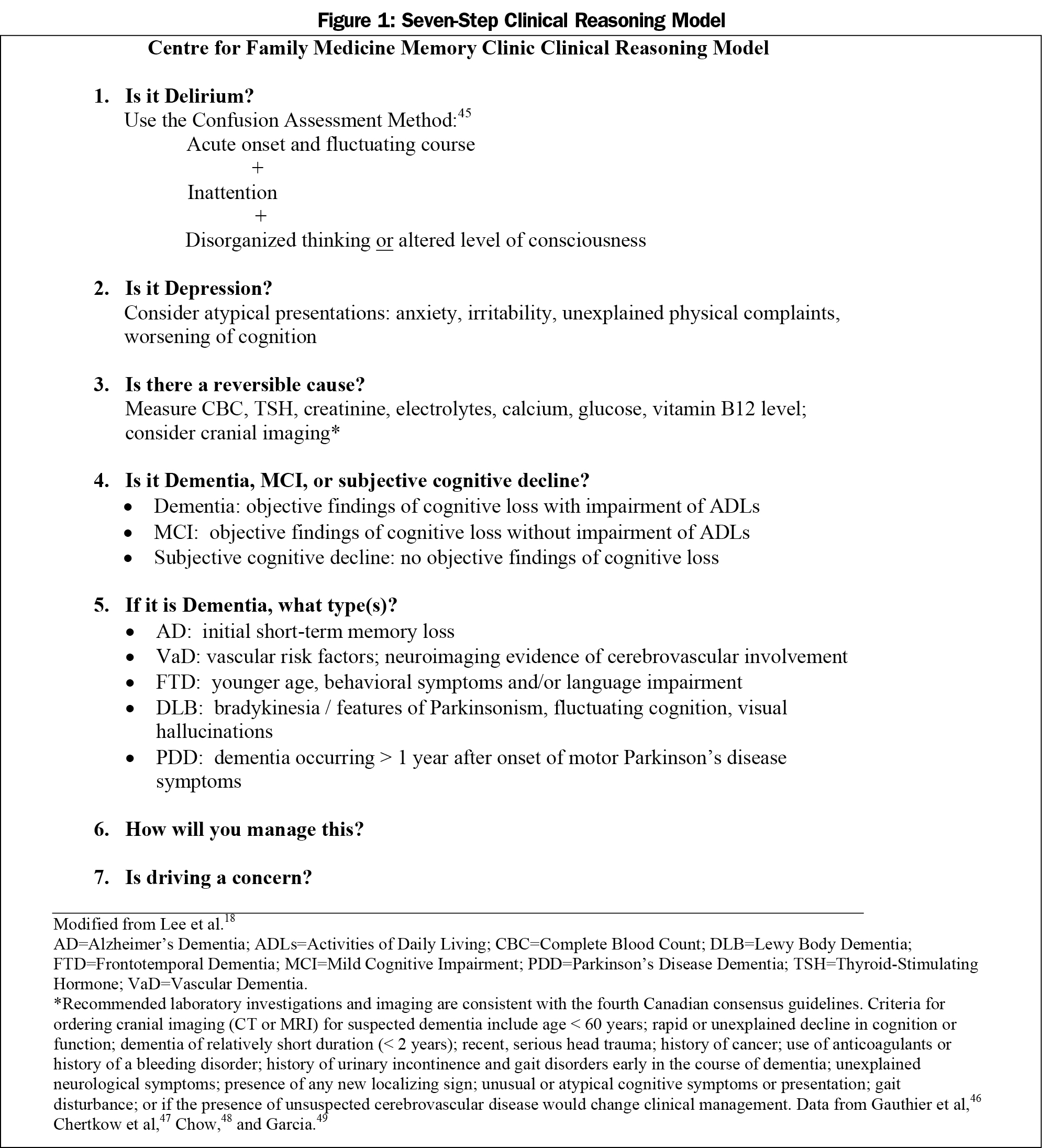
The objectives of this didactic and case-based workshop are to: (1) List features which allow the clinical differentiation between normal aging, MCI, and dementia, and between common forms of dementias; (2) Explain common office-based cognitive tests and investigations that can assist in the diagnosis; (3) Review basic initiation and monitoring of medications used in the management of patients with dementia; (4) Describe an approach to driving issues; and (5) Differentiate patients that can safely be diagnosed and managed by the family physician from those requiring a referral to a specialist. This workshop is 3 hours in length, consistent with recommendations for CME activities sponsored by the Ontario College of Family Physicians. Within the workshop, participants are presented with a seven-step clinical reasoning model to simplify the process of accurately assessing patients with memory difficulties, and to further support the diagnostic process, a “brain map” tool was developed to help organize clinical and cognitive test findings.18
The seven-step clinical reasoning model (Figure 1) and brain map19 provide clinicians with a structured approach to assessment. The process includes consideration of conditions that might present with cognitive symptoms, such as delirium or depression, as well as screening for reversible causes consistent with Canadian consensus guidelines22,23 and consideration of medication adverse effects. If these are excluded, the next step is the differentiation of dementia, mild cognitive impairment, and subjective cognitive impairment.24 Final steps in this approach address care management and assessment of driving safety concerns. The brain map assists physicians to differentiate potential types of dementia by the order in which symptoms and cognitive deficits appear over time, based on common clinical presentation features and areas of the brain typically affected by the various types of dementia. This clinical reasoning model and brain map are described in more detail elsewhere.18
Consistent with the theory of cognitive apprenticeship,20 these tools create a clinically relevant framework to facilitate the diagnostic process and impact health outcomes. A recent study of the introduction of algorithms for the assessment of patients presenting with falls or syncope demonstrated a reduction in readmission rates from 12% at baseline to 0% after implementation.21 To reinforce and sustain learning gained in the workshop, laminated cards are provided summarizing frequently-needed information such as dose titration of medications used in dementia care, drugs associated with high anticholinergic load and potential alternatives, considerations in fitness to drive, as well as the clinical reasoning approach itself. Research on CME indicates that the most effective methods to change behaviors involve multiple educational strategies including written materials or toolkits.22
The purpose of this study was to examine the impact of this workshop to provide primary care clinicians with a structured clinical reasoning approach to dementia diagnosis and brain map tool on self-perceived changes in knowledge, confidence, and ability to assess and manage memory problems and on self-reported application of learning to clinical practice.
Participants
Study participants were primary care clinicians (family physicians and nurse practitioners) participating in 20 CME dementia workshops delivered between October 2012 and April 2016 (N=392). Eight workshops were delivered by two authors (LL, WW); and 12 were delivered by LL independently, in 14 cities in Canada.
Evaluation Design and Outcomes
A survey methodology was used in this study. The evaluation of this education workshop was guided by Kirkpatrick’s model for program evaluation, which focuses on four levels of evaluation: reaction (eg, satisfaction), learning (knowledge, skill acquisition), behavior (application of new knowledge), and results (anticipated impacts, eg, increased diagnosis of dementia).23 This study evaluated the first three levels of Kirkpatrick’s model focusing on overall perceptions of the workshop and relevance to practice (reactions), changes in knowledge and ability related to dementia assessment and management (learning) and application of workshop learnings to practice (behavior). Consistent with social cognitive theory,24,25 which predicts that confidence impacts engagement in practice improvements, confidence in ability to assess and manage dementia were also evaluated in this study.
Data Collection
At the end of the workshop, participants were invited to complete a paper-based survey in which they were asked to rate the workshop (fair, poor, good, very good, excellent) and its relevance to their clinical practice (5-point scale: strongly disagree to strongly agree). They were also asked to describe their practice setting, number of years in clinical practice, and to rate the extent to which their formal education prepared them to manage dementia (5-point scale: not at all to extremely well).
Three months following the workshop, participants (N=242) of 12 consecutively delivered workshops from October 2012 to November 2014 received an invitation to complete an online survey in which they were asked whether they had applied new knowledge from the workshop to their clinical practice, what challenges they experienced in doing so, and to describe at least one way in which their practice had changed following the workshop (open-ended response). Using 5-point rating scales (less now to more now), survey respondents were asked to rate their current level of knowledge, confidence, and ability to assess and manage memory problems in comparison to prior to the workshop.
In both surveys, using a 5-point rating scale (1=not at all, 5=extremely), respondents were asked to rate the helpfulness of the clinical reasoning approach, brain map, and other materials to their learning (workshop survey) and application to practice (follow-up survey).
Using SPSS 25.0 (IBM Corp, Armonk, NY), descriptive statistics (frequencies, means, standard deviations) were calculated. Chi-square analysis and analysis of variance were used, as appropriate, to test for significant differences in demographic characteristics. Open-ended responses were analyzed using descriptive content analysis, in which reoccurring themes where identified.26 This study was approved by the Hamilton Integrated Research Ethics Board, McMaster University.
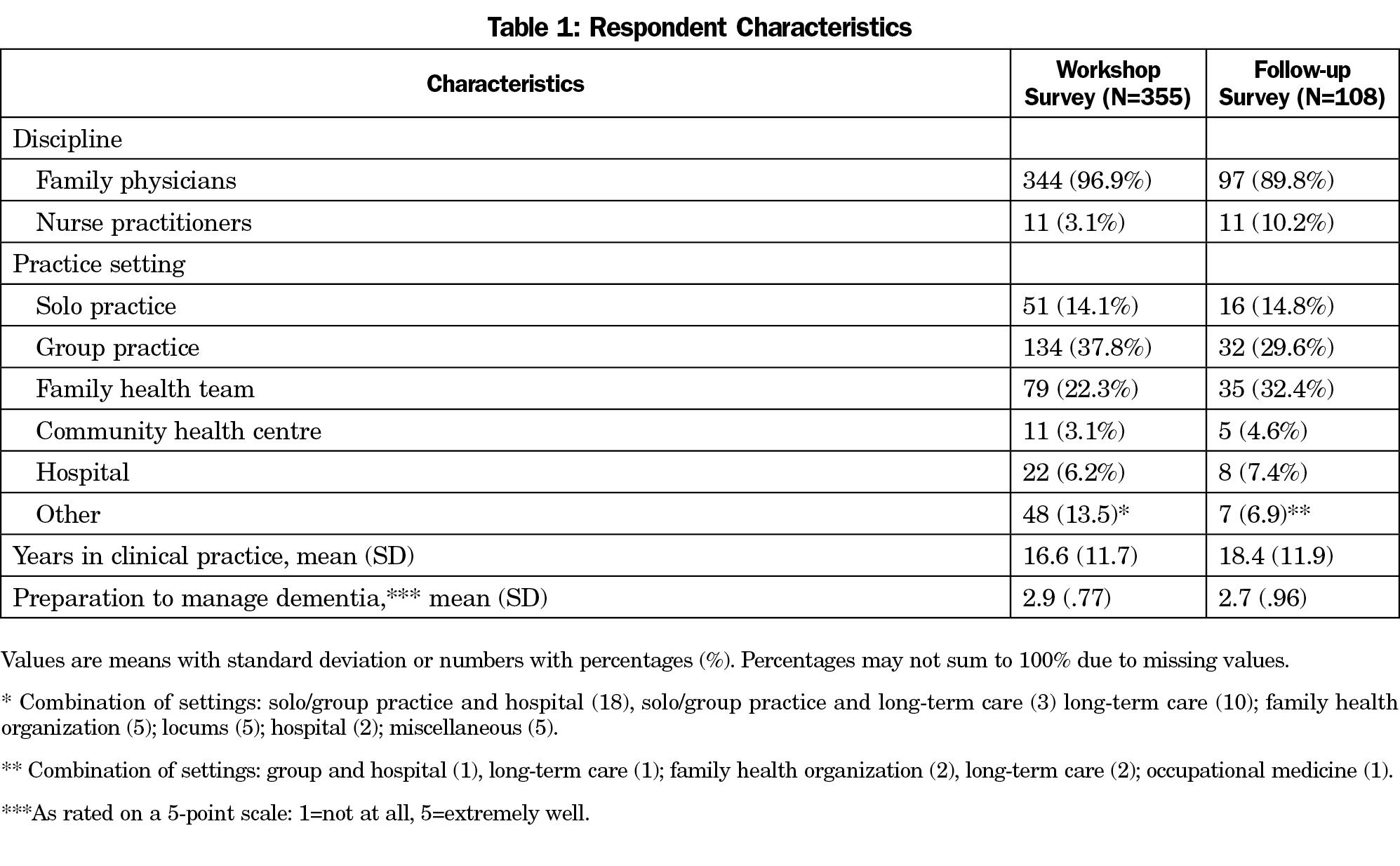
Ninety-one percent (N=355/392) of participants completed a workshop survey and 45% (N=108/242) completed the follow-up survey. The majority of respondents for both surveys were family physicians and were in group practice and had been in practice an average of 17 to 18 years (Table 1). Mean ratings of their preparedness to manage dementia based on formal training were moderately low, as reported in both surveys. There were no significant differences in these respondent characteristics between the two surveys.
The workshop was well received, with the majority of survey respondents providing ratings of very good (26%) or excellent (66%). Similarly, the majority of respondents agreed (sum of agree and strongly agree ratings) that the workshop information was relevant to their practice (98%).
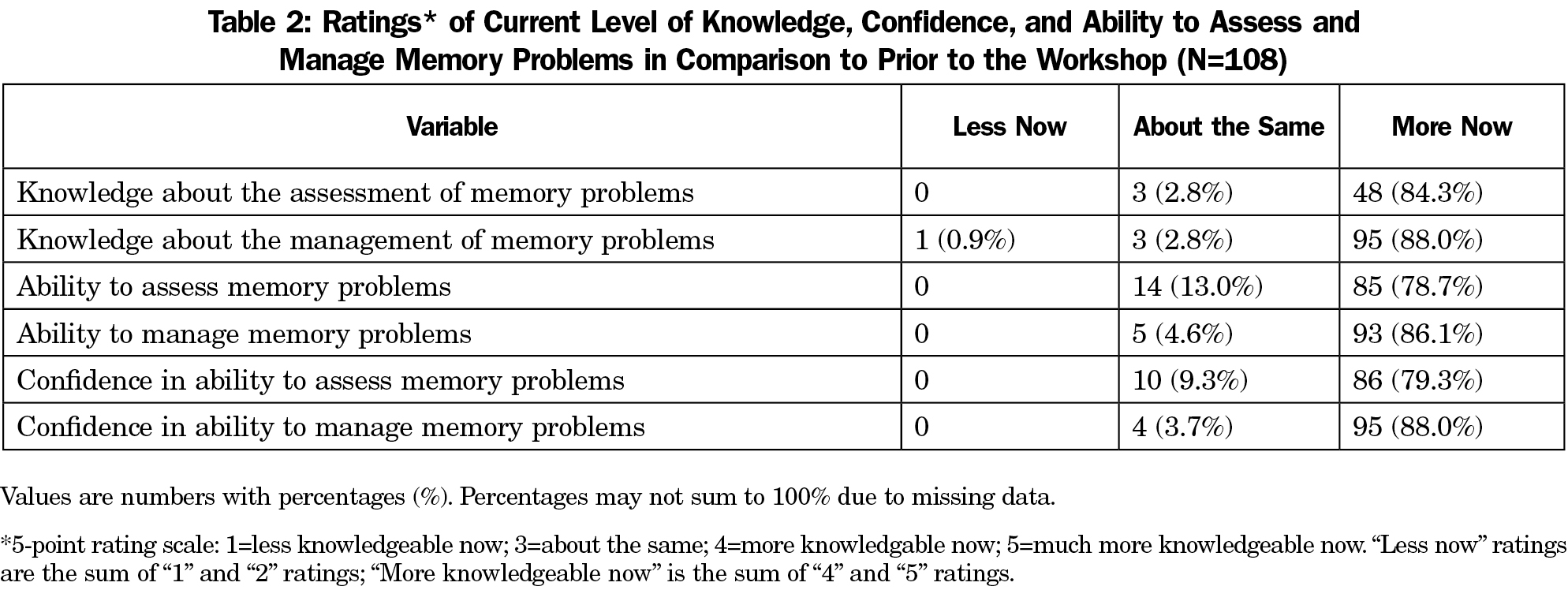
At follow-up the majority of respondents (>79%) reported that as a result of the workshop, they were more knowledgeable, better able, and more confident in their ability to assess and manage memory problems (Table 2).
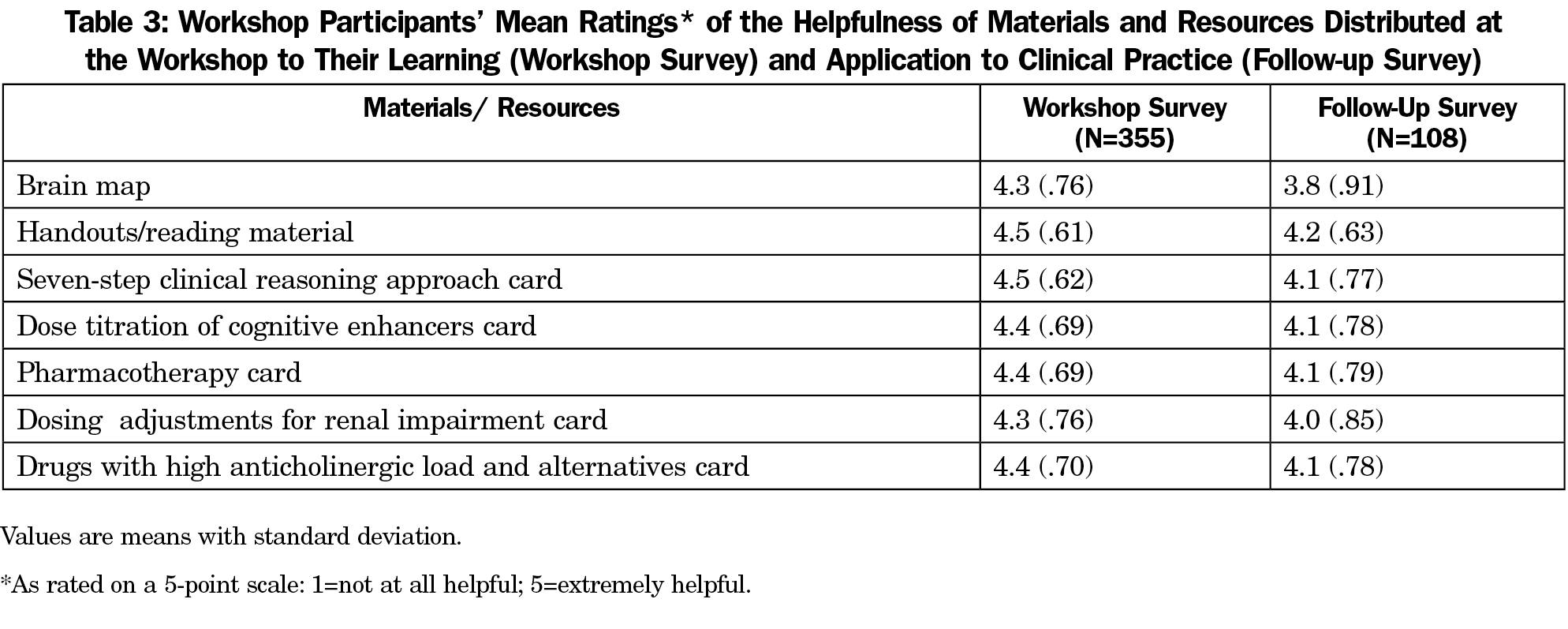
The majority of respondents provided ratings of the clinical reasoning approach and brain map being very or extremely (sum of these two ratings) helpful to their learning for (85% and 93%, respectively) and to application to practice (84% and 66%, respectively). Mean ratings of the helpfulness, or value, of the clinical reasoning approach and brain map reflected that participants found these very useful to their learning (M=4.1 and 3.8, respectively) and to application in practice (M=4.5 and 4.3, respectively; Table 3).
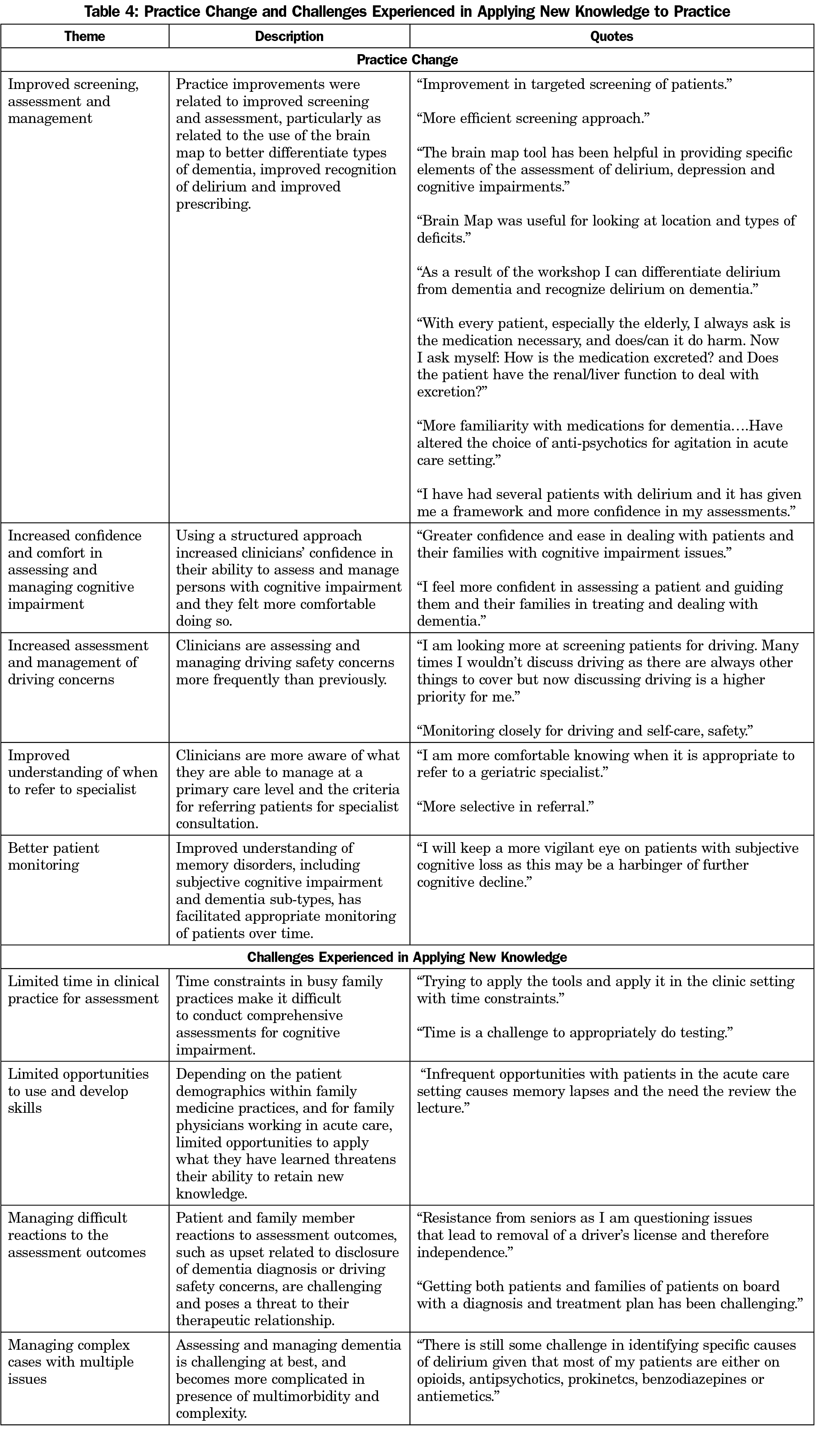
At follow-up, 92.6% (N=100) of survey respondents reported that they had applied what they had learned in the workshop to their clinical practice. Lack of opportunity was identified as a key reason for inability to apply new knowledge to practice. Analysis regarding the ways in which clinical practice changed as a result of this workshop generated eight themes related to practice change: (1) Improved screening and assessment with better use of assessment tools and an improved approach to diagnosis and management; (2) Use of the brain map to better differentiate types of dementia; (3) Improved recognition of delirium and differentiation of dementia and delirium; (4) Improved prescribing with greater consideration given to impact on renal function and anticholinergic load; (5) Increased confidence and comfort in assessing and managing cognitive impairment; (6) Increased assessment and management of driving concerns; (7) Improved understanding of when to refer for specialist consultation; and (8) Better monitoring of patients with memory concerns. In applying new knowledge, respondents reported challenges related to time constraints, limited opportunities to use and develop skills, managing difficult patient reactions to the assessment outcomes, and managing complex cases. Quotes illustrating these themes are presented in Table 4.
This study suggests that a workshop based on a structured clinical reasoning approach to dementia diagnosis and management may be helpful to participants’ learning and application to clinical practice.
In teaching about dementia, it is important to provide a structure or framework that organizes the tasks of assessment and treatment into a manageable role without oversimplification. The cognitive load of learning such a complex domain may seem overwhelming without clear guidance and cognitive schemas.27 The decision tools provided in this workshop may help to influence thought processes by providing a structure to frame and categorize complex aspects of a clinical situation to guide clinical practice.28 This is similar to the concept of scaffolding, a metaphor for providing learning support, such as clinical algorithms, during teaching as one provides a physical scaffold around a building under construction, and which addresses the learning of concepts and metacognitive skills.29,30 Several studies have described the use of instructional scaffolds as structured approaches to facilitate learning.29,31
It is likely that peer teaching also contributed to the effectiveness of this educational opportunity. One possible consequence of specialists teaching family physicians about dementia is the unspoken message that only specialists can effectively manage dementia, leaving physicians more knowledgeable, but hesitant to tackle such a complex topic without referral. The workshop described here was designed by family physicians for family physicians taking into account how family practice functions. Learners may gain more confidence in their ability to apply new knowledge when new strategies, processes, and approaches are shared by teachers working within the same context. The importance of family physicians learning from family physicians is a basic tenet of family medicine curriculum reform, which emphasizes centering education in family medicine with the use of family medicine educators within family medicine settings, so as to be relevant to the learning needs of residents.32
Despite clinicians reporting practice improvements associated with this educational initiative, they nonetheless experienced challenges associated with dementia care, many of which are well documented in the literature.1,3 These challenges may be addressed through the recent development of interprofessional and collaborative care approaches to dementia within the primary care setting.33 The Primary Care Collaborative Memory Clinic model in which family physician-led memory clinics are embedded in group practice settings provides comprehensive assessment and recommendations for management and continuing shared care with the patient’s own primary care physician.34 This care model has demonstrated ability to address several challenges associated with dementia care in primary care practice such as timely access to diagnosis, assessment of driving concerns, and need for interdisciplinary care.35 Such practice setting and system-level initiatives may be complementary to brief CME opportunities, as the one presented here for physicians and other brief programs targeting interprofessional groups,36 which aim to develop skills at an individual clinician level. Together, such programs can build capacity within primary care to effectively deliver person-centered care that meets the needs of an aging population.
Limitations
There are several limitations to this study. The measurement of outcomes and impacts in this evaluation study were primarily based on self-report. Although there is no objective data to support reports of practice change in this study, self-reported self-efficacy and confidence have been associated with practice behaviors,25 suggesting that the changes to confidence and abilities reported in this study potentially did impact behavior. This is supported by the responses to the 3-month follow-up survey listing numerous specific changes to practice behavior attributed to the workshop. Self-assessment methods have been used effectively in several studies to examine learners’ evaluations of the impacts associated with medical education37-39 and to evaluate program effectiveness and quality.40 Using perceived change methodology in the follow-up survey may have introduced a response bias reflecting what is expected with overestimations of practice changes.41 More objective measures of practice change would be ideal (eg, chart audits), however for pragmatic reasons this was not possible. The response rate for the follow-up survey was low (45%), likely due to this initiative being limited to the one workshop 3 months prior; however, those who completed the survey were demographically similar to the entire sample. It is possible that those who did not respond to the follow-up survey may have had differing experiences. A recent study, using a similar methodology to assess the impact of an interprofessional half-day dementia workshop also experienced a low response rate to a 3-month post-training survey; this corroborates the difficulties associated with acquiring ample follow-up responses for brief training initiatives.36 An additional limitation is that the individuals who participated in this workshop were self-selected and thus highly motivated to complete the training. This selection bias may limit the generalizability of these findings. Future studies could explore the value of this structured approach in family medicine residency programs.
This paper adds to a growing body of research on strategies to improve dementia care with effective CME interventions. A 3-hour workshop focused on an organized approach to cognitive impairment, using didactic presentations, case-based discussion, and laminated pocket cards of the “brain map” and clinical reasoning model was effective in improving participants’ confidence to assess and manage patients with cognitive impairment, with self-reported improvements to dementia assessment and management. Nonetheless, clinicians continued to experience challenges in providing dementia care, highlighting the complexity of this condition and need for multiple strategies for capacity building in primary care.
Acknowledgments
The authors are grateful to study participants, whose participation in these dementia workshops reflect their commitment to improving care for older adults with memory concerns.
Financial Support: This study was supported by the Canadian Institutes of Health Research Knowledge Translation Supplement Grant.
Presentation (preliminary data): Lee L, Hillier LM, Weston WW. Improving dementia assessment: effect of a structured approach and “brain map” tool. Family Medicine Forum, Vancouver, BC, November 7-9, 2013.
References
- Aminzadeh F, Molnar FJ, Dalziel WB, Ayotte D. A review of barriers and enablers to diagnosis and management of persons with dementia in primary care. Can Geriatr J. 2012;15(3):85-94.
https://doi.org/10.5770/cgj.15.42.
- Pimlott NJ, Persaud M, Drummond N, et al. Family physicians and dementia in Canada: Part 2. Understanding the challenges of dementia care. Can Fam Physician. 2009;55(5):508-9.e1, 7.
- Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23(4):306-314.
https://doi.org/10.1097/WAD.0b013e3181a6bebc.
- Lang L, Clifford A, Wei L, et al. Prevalence and determinants of undetected dementia in the community: a systematic literature review and a meta-analysis. BMJ Open. 2017;7(2):e011146.
https://doi.org/10.1136/bmjopen-2016-011146.
- Smetanin P, Kobak P, Briante C, et al. Rising Tide: The Impact of Dementia in Canada in 2008 to 2038. Toronto, ON: Risk Analytica; 2009, Available at http://www.alzheimer.ca/~/media/Files/national/Advocacy/ASC_Rising_Tide_Full_Report_e.pdf. Accessed April 6, 2017.
- Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187-194.
https://doi.org/10.1111/j.1532-5415.2004.52054.x.
- Leifer BP. Early diagnosis of Alzheimer’s disease: clinical and economic benefits. J Am Geriatr Soc. 2003;51(5)(Suppl Dementia):S281-S288.
https://doi.org/10.1046/j.1532-5415.5153.x.
- Canadian Institute for Health Information. Analysis in brief: alternative level of care in Canada. 2009. Ottawa, ON: Canadian Insititute for Health Information. https://secure.cihi.ca/free_products/ALC_AIB_FINAL.pdf. Accessed April 6, 2017.
- Pimlott NJG, Siegel K, Persaud M, et al. Management of dementia by family physicians in academic settings. Can Fam Physician. 2006;52(9):1108-1109.
- Hogan DB, Borrie M, Basran JFS, et al. Specialist physicians in geriatrics-report of the canadian geriatrics society physician resource work group. Can Geriatr J. 2012;15(3):68-79.
https://doi.org/10.5770/cgj.15.41.
- Massoud F, Lysy P, Bergman H. Care of dementia in Canada: a collaborative care approach with a central role for the primary care physician. J Nutr Health Aging. 2010;14(2):105-106.
https://doi.org/10.1007/s12603-010-0020-2.
- Prins A, Hemke F, Pols J, Moll van Charante EP. Diagnosing dementia in Dutch general practice: a qualitative study of GPs’ practices and views. Br J Gen Pract. 2016;66(647):e416-e422.
https://doi.org/10.3399/bjgp16X685237.
- Dubois B, Padovani A, Scheltens P, Rossi A, Dell’Agnello G. Timely Diagnosis for Alzheimer’s Disease: A Literature Review on Benefits and Challenges. J Alzheimers Dis. 2016;49(3):617-631.
https://doi.org/10.3233/JAD-150692.
- Cahill S, Clark M, Walsh C, O’Connell H, Lawlor B. Dementia in primary care: the first survey of Irish general practitioners. Int J Geriatr Psychiatry. 2006;21(4):319-324.
https://doi.org/10.1002/gps.1464.
- Turner S, Iliffe S, Downs M, et al. General practitioners’ knowledge, confidence and attitudes in the diagnosis and management of dementia. Age Ageing. 2004;33(5):461-467.
https://doi.org/10.1093/ageing/afh140.
- Moore A, Patterson C, Lee L, Vedel I, Bergman H; Canadian Consensus Conference on the Diagnosis and Treatment of Dementia. Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia: recommendations for family physicians. Can Fam Physician. 2014;60(5):433-438.
- Lee L, Weston WW, Hillier LM. Developing memory clinics in primary care: an evidence-based interprofessional program of continuing professional development. J Contin Educ Health Prof. 2013;33(1):24-32.
https://doi.org/10.1002/chp.21163.
- Lee L, Weston WW, Heckman G, Gagnon M, Lee FJ, Sloka S. Structured approach to patients with memory difficulties in family practice. Can Fam Physician. 2013;59(3):249-254.
- Lee L, Weston W, Heckman G, et al. A structured approach to the patient with memory difficulties in family practice. Supplemental Data File: The Centre for Family Medicine Memory Clinic Brain Map. Can Fam Physician. 2013;59(3):249-254. http://www.cfp.ca/content/59/3/249/tab-supplemental. Accessed April 6, 2017.
- Ambrose SA, Bridges MW, DiPietro M, et al. How learning works - 7 research-based principles for smart teaching. San Francisco: Jossey-Bass; 2010.
- Parry SW, Frearson R, Steen N, Newton JL, Tryambake P, Kenny RA. Evidence-based algorithms and the management of falls and syncope presenting to acute medical services. Clin Med (Lond). 2008;8(2):157-162.
https://doi.org/10.7861/clinmedicine.8-2-157.
- Thomas DC, Johnston B, Dunn K, et al. Continuing medical education, continuing professional development, and knowledge translation: improving care of older patients by practicing physicians. J Am Geriatr Soc. 2006;54(10):1610-1618.
https://doi.org/10.1111/j.1532-5415.2006.00879.x.
- Kirkpatrick DL, Kirkpatrick JD. Evaluating Training Programs. 3rd ed. San Francisco: Berrett-Koehler; 2006.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191-215.
https://doi.org/10.1037/0033-295X.84.2.191.
- Bandura A. Self-efficacy - The Exercise of Control. New York: W.H. Freeman and Company; 1997.
- Cavanagh S. Content analysis: concepts, methods and applications. Nurse Res. 1997;4(3):5-16.
- Kirschner PA. Cognitive load theory: implications of cognitive load theory on the design of learning. Learn Instr. 2002;12(1):1-10.
https://doi.org/10.1016/S0959-4752(01)00014-7.
- Neistadt ME. Teaching clinical reasoning as a thinking frame. Am J Occup Ther. 1998;52(3):221-229.
https://doi.org/10.5014/ajot.52.3.221.
- Dawn S, Dominguez KD, Troutman WG, Bond R, Cone C. Instructional scaffolding to improve students’ skills in evaluating clinical literature. Am J Pharm Educ. 2011;75(4):62. https://doi.org/10.5688/ajpe75462.
- Fisher D, Frey N. Scaffolds for learning. In: Fisher D, Frey N, eds. Guided instruction: How to develop confident and successful learners. Alexandria, VA: ASCD Publishers; 2010.
- Ivanoff CS, Hottel TL. A four-tier problem-solving scaffold to teach pain management in dental school. J Dent Educ. 2013;77(6):723-731.
- Tannenbaum D, Kerr J, Konkin J, et al. Triple C competency-based curriculum. Report of the Working Group on Postgraduate Curriculum Review - Part 1. Mississauga, ON: College of Family Physicians of Canada; 2011.
- Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148-2157.
https://doi.org/10.1001/jama.295.18.2148.
- Lee L, Hillier LM, Heckman G, et al. Primary Care-Based Memory Clinics: Expanding Capacity for Dementia Care. Can J Aging. 2014;33(3):307-319.
https://doi.org/10.1017/S0714980814000233.
- Lee L, Hillier LM. Family physicians’ perspectives on memory clinics in primary care. Neurodegener Dis Manag. 2016;6(6):467-478. https://doi.org/10.2217/nmt-2016-0031.
- Tan ZS, Damron-Rodriguez J, Cadogan M, et al. Team-based interprofessional competency training for dementia screening and management. J Am Geriatr Soc. 2017;65(1):207-211. https://doi.org/10.1111/jgs.14540.
- Bradley KE, Andolsek KM. A pilot study of orthopaedic resident self-assessment using a milestones’ survey just prior to milestones implementation. Int J Med Educ. 2016;7:11-18. https://doi.org/10.5116/ijme.5682.6dfd.
- Mandel LS, Goff BA, Lentz GM. Self-assessment of resident surgical skills: is it feasible? Am J Obstet Gynecol. 2005;193(5):1817-1822.
https://doi.org/10.1016/j.ajog.2005.07.080.
- Gow KW. Self-evaluation: how well do surgery residents judge performance on a rotation? Am J Surg. 2013;205(5):557-562.
https://doi.org/10.1016/j.amjsurg.2013.01.010.
- Peterson LN, Rusticus SA, Wilson DA, Eva KW, Lovato CY. Readiness for Residency: A Survey to Evaluate Undergraduate Medical Education Programs. Acad Med. 2015;90(11)(suppl):S36-S42.
https://doi.org/10.1097/ACM.0000000000000903.
- Lam T, Bengo P. A comparison of three retrospective self-reporting methods of measuring change in instructional practice. Am J Eval. 2003;24(1):65-80.
https://doi.org/10.1177/109821400302400106.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
https://doi.org/10.7326/0003-4819-113-12-941.
- Gauthier S, Patterson C, Chertkow H, et al. Recommendations on the 4th Canadian Consensus Conference on the diagnosis and treatment of Dementia (CCCDTD4). Can Geriatr J. 2012;15(4):120-126.
- Chertkow H, Bergman H, Schipper HM, et al. Assessment of suspected dementia. Can J Neurol Sci. 2001;28(S1)(suppl 1):S28-S41.
https://doi.org/10.1017/S0317167100001189.
- Chow T. Structural neuroimaging in the diagnosis of dementia. Alzheimers Dement. 2007;3(4):333-335.
https://doi.org/10.1016/j.jalz.2007.07.016.
- Garcia A. Cobalamin and homocysteine in older adults: do we need to test for serum levels in the work-up of dementia? Alzheimers Dement. 2007;3(4):318-324.
https://doi.org/10.1016/j.jalz.2007.07.003.



There are no comments for this article.