Background and Objectives: Racism’s impact on health has been well documented. Health professional programs are beginning to help learners understand this social determinant of health through curricular integration of education related to racism. Yet educators are hesitant to integrate these concepts into curricula because of lack of expertise or fear associated with learner responses to this potentially sensitive topic. The purpose of this study is to describe the responses of learners to learning sessions on racism as a social determinant of health (SDOH) highlighting structural, personally-mediated, and internalized racism.
Methods: Two separate groups—a family and community medicine (FCM) residency program (N=23) and a community health leadership program (N=14)—participated in lectures and workshops on internalized, personally-mediated, and structural sources of racism, and tours introducing them to the local community’s historical roots of structural racism, including discussions/reflections on racism’s impact on health and health care. Mixed-methods evaluation consisted of learner assessments and reflections on the experiences.
Results: FCM sessions received a positive reception with session averages of 4.15 to 4.75, based on a Likert-type scale (1=did not meet expectations to 5=exceeded expectations). Thematic analysis of community health leadership participant reflections showed thought processing connected to a better understanding of racism. Overall, themes from both programs reflected positive experiences of the sessions.
Conclusions: Our preliminary study findings suggest that educators who encounter internal or external barriers to integrating racism-related concepts into curricula might find that these concepts are well received. This study lays the groundwork for further research into best practices for integration of curriculum on racism as an SDOH for medical schools, residency programs, and other related educational settings.
Racism’s impact on health is well documented.1-4 Patients experiencing racism often have disparities in mental health, maternal morbidity and mortality, and cardiovascular treatment.2,3,5,6 Medical schools and residency programs are integrating curriculum on racism as a crucial social determinant of health7-9 but this has been difficult.8,10,11 Educators’ fear of learner reactions is a barrier to facilitating racial dialogue.
This study sought to evaluate learner reactions to teaching about racism as a social determinant of health. Activities were organized by educators interested in teaching about the impact of racism on health. The sessions occurred with postgraduate students and graduate students in two separate programs.
Learner reactions to discussions about racism can inform family medicine (FM) educators who want to implement curricula on the role of racism on health outcomes.12 This is an initial assessment of learners’ responses to sessions drawing heavily on Jones’ “Three Levels of Racism”13 framework. To our knowledge, this is one of the first reports from an effort to contextualize the three levels of racism in a medical education setting.
Setting and Participants
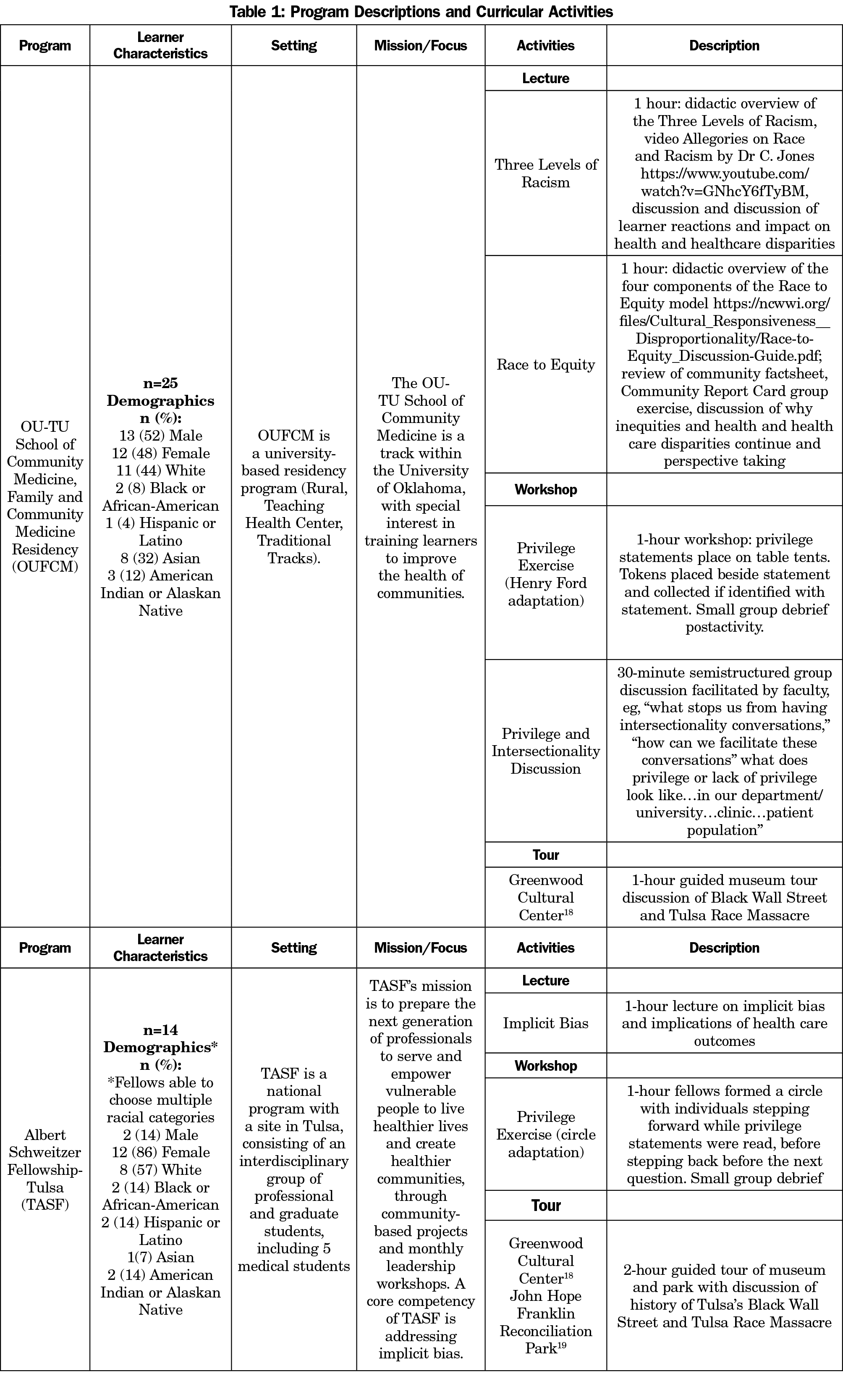
Participants were OU-TU School of Community Medicine University of Oklahoma, Department of Family and Community Medicine (OUFCM) residents, and Tulsa Albert Schweitzer Fellowship (TASF) fellows (Table 1). OUFCM residency sessions occurred during weekly didactic sessions. TASF sessions occurred during monthly leadership meetings. Activities occurred between April 2017 and February 2018. The Institutional Review Boards of the University of Oklahoma Health Sciences Center and University of Tulsa granted this study exempt status.
Intervention
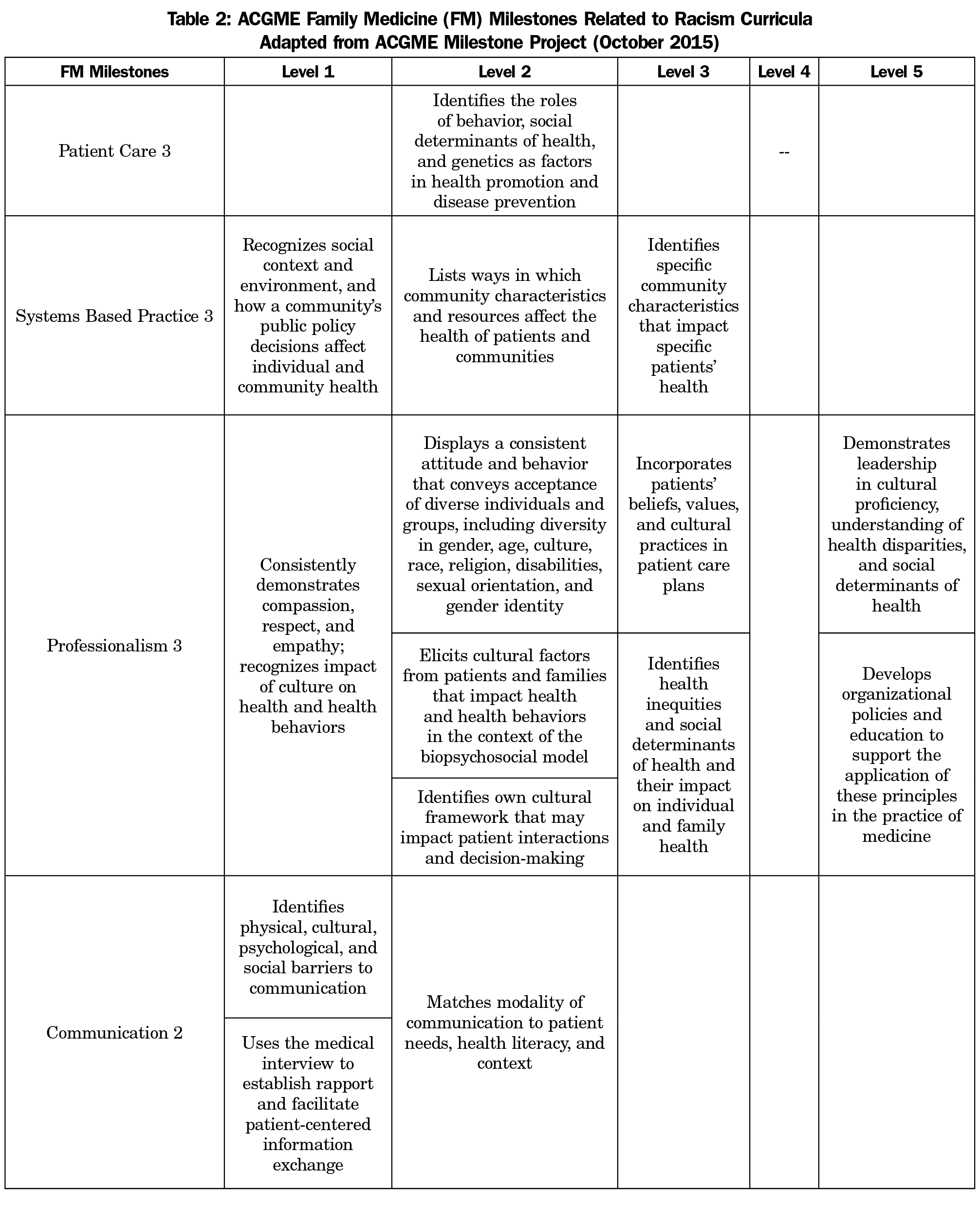
Two OUFCM faculty (a family medicine physician and a behavioral psychologist) and TASF’s director designed and implemented this intervention to enhance learners’ understanding that individual experiences are embedded within a social-cultural context.14-15 Table 1 describes the sessions. Activities were based on the conceptual framework of the “Three Levels of Racism,”13 and drew on the “Toolkit for Teaching About Racism” presented at the 2016 Society of Teachers of Family Medicine (STFM) Annual Spring Conference,16 and the Accreditation Council on Graduate Medical Education (ACGME) Family Medicine Residency Milestones17 related to racism (Table 2).
Educators incorporated tours of the Greenwood Cultural Center (GCC; both groups),18 and John Hope Franklin Reconciliation Park (TASF only).19 Both memorialize the 1921 Tulsa Race Massacre.20 These visits exposed learners to the roots of structural racism within the community. The tours connected a profound historical event to local community health outcomes.
Classroom sessions formed another part of the intervention. Privilege activities16,21 illustrated how race, ethnicity, and other socioeconomic and cultural factors influenced learners’ experiences in everyday life. TASF used the privilege activity from the Toolkit,16 with modification for space (Table 1). OUFCM’s planned privilege session was delayed due to acts of explicit racism affecting residents and their families. Facilitators modified an activity from Henry Ford Health Systems21 to limit vulnerability as compared with the public nature of the Toolkit’s exercise. Privilege statements were privately read. If the resident identified with the statement, they collected a token. Stratification occurred by number of tokens with small group debriefing sessions after the activity.
Data Collection and Analysis
An ex-postassessment of responses to learning sessions was conducted. Quantitative and qualitative surveys were given to OUFCM residents and narrative reactions were completed by TASF fellows. Data from the groups were collected and analyzed in parallel, then triangulated for a final interpretation.
OUFCM. Standard anonymous postdidactic assessments comprised of five questions regarding the quality and value of sessions were administered and written feedback was collected (Table 3). A mean score for all respondents per learning session was available for analysis. Measures of central tendency were calculated. Written comments were collected after the tour of GCC.
TASF. Postsession, fellows (nonanonymous) submitted answers via email to the question “How will you incorporate what you learned during this monthly meeting into your project, studies, and other aspects of your life?” Facilitators applied inductive methods to analyze qualitative data, condensed raw textual data, identified themes, and formed a hypothesis based on those themes.22
Resident assessments of the sessions were positive, with a mean rating above 4 on a 5-point scale (Table 3). Themes derived from the residents’ written feedback (Table 4) suggest increased awareness. Themes and quotes from the TASF fellows fall into the conceptual framework of the Three Levels of Racism (Table 5),13 indicating learners’ increased insight into the connection between race and health. The themes identified were “topic is sensitive,” “will lead to advocacy and education,” “deepened understanding of bias and privilege (critical consciousness),” “challenged assumptions of self, colleagues, patients and client,” and “increased self-awareness (critical self-awareness).”
Prior studies of resident reactions to discussions on racism are limited and learner responses are mixed.23 Our results show a positive learner reaction to addressing racism as a factor in health outcomes in an educational setting. One learner did indicate that there was too much exposure to the topic (Table 4). Future research could explore appropriate spacing and time needed for education around this important topic. OUFCM’s ratings for this session were lower than the median of other didactics. Further research could explore differences in perception of sessions about racism as an SDOH in comparison with traditional biomedical lectures.
This study has several limitations. As a retrospective analysis, there was no pretest conducted and the authors did not have comprehensive data. For example, while the average rating of the OUFCM’s survey was available for analysis, specific results for each question were not. Also, data were not available to calculate a response rate for all sessions, thus precluding an estimate of nonresponse bias. Additionally, the facilitators conducted data analysis, which introduces bias in the interpretation. Furthermore, participants self-selected into community health programs which may increase the positive reception to the sessions. Finally, this study did not permit evaluation of changes in attitude nor effects on behavior of participants.
Resident assessments indicated the modified privilege exercise was well received, suggesting value in modifying activities to needs of individual programs. Our findings suggest educator fear of negative responses should not be a barrier to implementing curricula on racism.
Acknowledgments
The authors thank the Department of Family and Community Medicine, OU-TU School of Community Medicine, University of Oklahoma residents and Tulsa Albert Schweitzer fellows who participated in the activities and shared their experiences. The authors also acknowledge Mayra Salazar, Oklahoma State University MS2; Ekene Ezenwa, OU-TU School of Community Medicine; Ashley Harvey, Oklahoma, State University–Human Development and Family Sciences PhD Candidate; Devin Howell, University of Tulsa MFA candidate; Janet Gaskins, MS; and Samuel Kirzner, MPH, for their contributions to this work.
Disclaimer: The opinions and assertions contained herein are the private views of the authors and should not be construed either as official or as reflecting the views of the University of Oklahoma or the Albert Schweitzer Fellowship.
References
- Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511. https://doi.org/10.1371/journal.pone.0138511
- Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60-e76. https://doi.org/10.2105/AJPH.2015.302903
- Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231-1238. https://doi.org/10.1007/s11606-007-0258-5
- Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979-987. https://doi.org/10.2105/AJPH.2011.300558
- Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7(1):13-30. https://doi.org/10.1023/A:1022537516969
- Smedley BD. The lived experience of race and its health consequences. Am J Public Health. 2012;102(5):933-935. https://doi.org/10.2105/AJPH.2011.300643
- Institute of Medicine. Unequal treatment: confronting racial and ethnic disparities in health care. In: Smedley BD, Stith AY, Nelson AR, eds. Washington, DC: National Academies Press; 2003.
- Sukhera J, Watling C. A framework for integrating implicit bias recognition into health professions education. Acad Med. 2018;93(1):35-40. https://doi.org/10.1097/ACM.0000000000001819
- Karani R, Varpio L, May W, et al. Commentary: racism and bias in health professions education: how educators, faculty developers, and researchers can make a difference. Acad Med. 2017;92(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 56th Annual Research in Medical Education Sessions):S1-s6.
- Sue DW. Race talk: the psychology of racial dialogues. Am Psychol. 2013;68(8):663-672. https://doi.org/10.1037/a0033681
- Acosta D, Ackerman-Barger K. Breaking the silence: time to talk about race and racism. Acad Med. 2017;92(3):285-288. https://doi.org/10.1097/ACM.0000000000001416
- Kirkpatrick D. Great ideas revisited. Train Dev. 1996;50(1):54-59.
- Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health. 2000;90(8):1212-1215. https://doi.org/10.2105/AJPH.90.8.1212
- Institute of Medicine (US) Committee on Assessing Interaction Among Social, Behavioral, and Genetic Factors in Health; Hernandez LM, Blazer DG, eds. Genes, behavior, and the social environment: moving beyond the nature/nurture debate. Washington, DC: National Academies Press; 2006: https://www.nap.edu/catalog/11693/genes-behavior-and-the-social-environment-moving-beyond-the-naturenurture. Accessed October 24, 2018.
- Phelan S, Kinsella EA. Occupational identity: engaging socio-cultural perspectives. J Occup Sci. 2009;16(2):85-91. https://doi.org/10.1080/14427591.2009.9686647
- White-Davis T, Edgoose J, Brown Speights JS, et al. Addressing racism in medical education: an interactive training module. Fam Med. 2018;50(5):364-368. https://doi.org/10.22454/FamMed.2018.875510
- The Accreditation Council for Graduate Medical Education and the American Board of Family Medicine. The Family Medicine Milestone Project. www.acgme.org/portals/0/pdfs/milestones/familymedicinemilestones.pdf. Revised October, 2015. Accessed February 28, 2018.
- Greenwood Cultural Center. http://www.greenwoodculturalcenter.com/. Accessed September 26, 201
- John Hope Franklin Reconciliation Park. https://www.jhfcenter.org/reconciliation-park. Accessed September 26, 2018.
- Staples, B. Unearthing a riot. New York Times Magazine. December 19, 1999. https://www.nytimes.com/1999/12/19/magazine/unearthing-a-riot.html. Accessed September 26, 2018
- Holm AL, Rowe Gorosh M, Brady M, White-Perkins D. Recognizing privilege and bias: an interactive exercise to expand health care providers’ personal awareness. Acad Med. 2017;92(3):360-364. https://doi.org/10.1097/ACM.0000000000001290
- Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):237-246. https://doi.org/10.1177/1098214005283748
- Willen SS, Bullon A, Good MJ. Opening up a huge can of worms: reflections on a “cultural sensitivity” course for psychiatry residents. Harv Rev Psychiatry. 2010;18(4):247-253. https://doi.org/10.3109/10673229.2010.493748






There are no comments for this article.