In the United States, over one million people have HIV.1 With a steady incidence and decreasing mortality, prevalence has risen.2 A Health Resources and Services Administration (HRSA) report projected a shortage of 502 full-time equivalent (FTE) HIV clinicians,3 raising concerns about workforce adequacy.4-6
Enumerating the HIV workforce has been difficult, since clinicians are trained across specialties. The HRSA report defined HIV clinicians as those who treat 20 or more HIV patients and found that 55% of HIV clinicians were primary care physicians (PCPs), 37% were infectious disease specialists, and 8% were nurse practitioners (NPs) or physician assistants (PAs).3
With capacity strained and maldistributed, primary care residency programs are critical to filling in the gap.3 Unfortunately, in a survey of family medicine residency program directors (PDs), only 25% felt that the majority of their graduates can provide HIV care and 22% had a formal HIV curriculum.7 In a similar survey of internal medicine residency PDs, about half reported having a formal HIV curriculum.8 In an effort to better understand family physicians’ contributions to the HIV workforce in order to guide training efforts, we identified family physicians providing HIV care and their characteristics.
In a cross-sectional study, we used 2014 Part D Medicare claims data and the 2014 American Medical Association (AMA) Masterfile to identify family medicine HIV clinicians. HIV clinicians were identified by searching the 2014 Medicare Part D Claims Database for prescription claims for HIV-related antiretroviral therapy (ART; appendix A at https://journals.stfm.org/media/2354/egan-appendixa.pdf) and identifying their National Provider Identifier (NPI) numbers. To protect privacy, Part D data only includes those prescribing each drug at least 11 times. Thus, we included physicians prescribing HIV drugs to 11 or more Medicare beneficiaries. Provider type was determined by using NPI designations to group clinicians as PCPs, infectious disease (ID) specialists, NPs/PAs, and other physician specialists. PCPs were further grouped as family medicine (FM), internal medicine (IM), and other (a group that included geriatricians, general practitioners, and pediatricians).
We then linked the PCPs in the study sample with the AMA Masterfile to describe their gender, rurality, years in practice, geographic region, medical degree, and medical school location (United States versus international).
We analyzed the data using Stata 14.0, calculated descriptive statistics, and used χ2 tests to assess the differences between HIV and non-HIV clinicians. Multivariate logistic regressions were performed. We performed regression, restricting it to family physicians matched from the AMA Masterfile. The American Academy of Family Physicians Institutional Review Board deemed our protocol exempt.
Of the 10,049 providers identified as HIV clinicians, 55% were PCPs, 30% were ID, 13.4% were other specialists, and 1% were NPs or PAs. Of the 5,576 PCPs, 66% were IM, 28% were FM, and 7% were other.
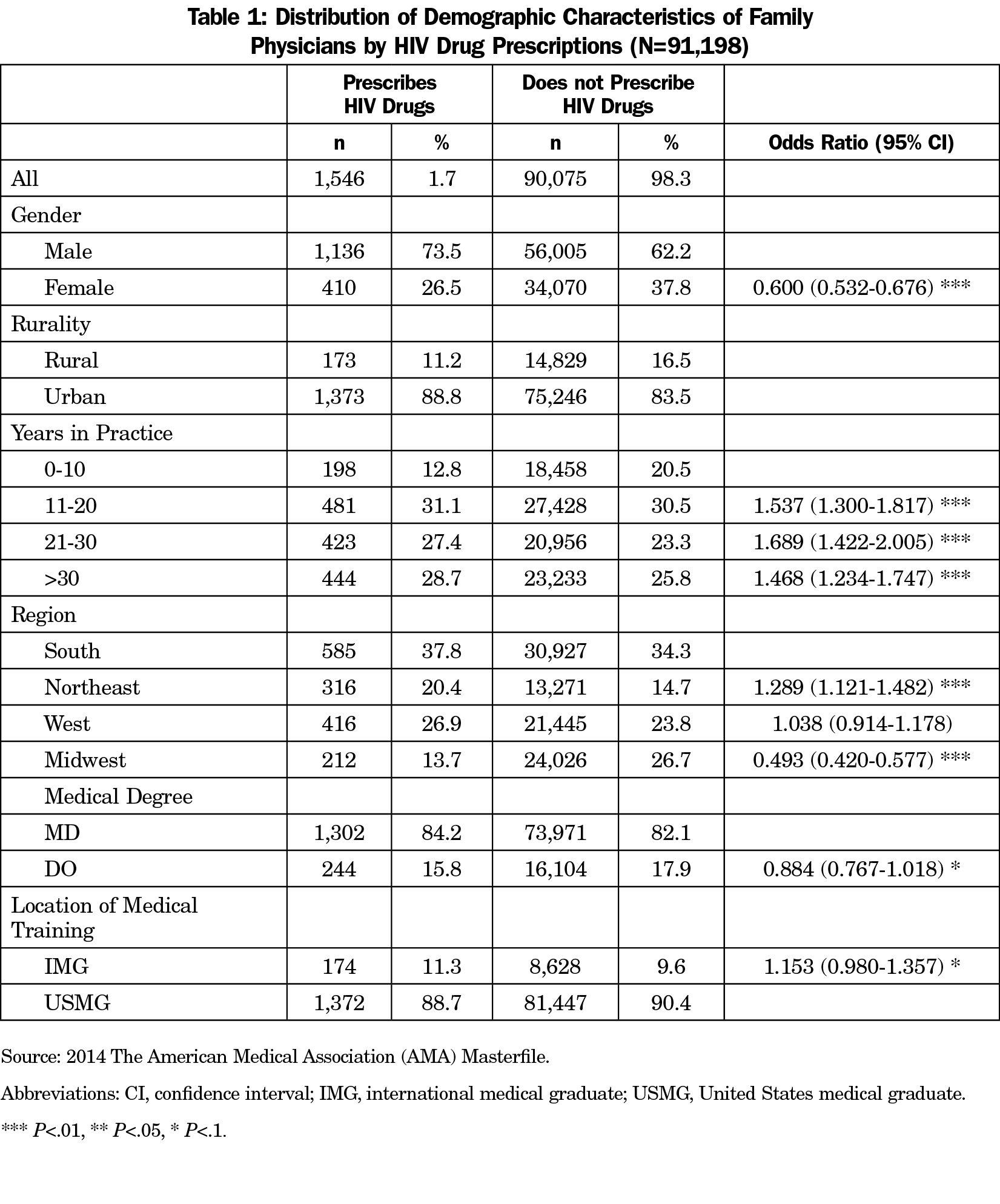
FM HIV clinicians are more likely to be male, practice in urban settings, and have been in practice for more than 10 years compared to family medicine non-HIV prescribers (Table 1).
Over half of HIV clinicians are in primary care. Our findings should be interpreted within the context of several limitations. For example, we only include Medicare providers and do not distinguish between actively managing and simply refilling medications. Despite these limitations, our specialty distribution mirrors other datasets. HRSA’s study found 55% PCPs and 37% infectious disease specialists.3 Of those credentialed as HIV specialists by the American Academy of HIV Medicine (AAHIV), 50% were PCPs and 29% ID, though the split among PCPs was more even (47% IM, 44% FM) according to written communication with AAHIV staff (June, 2018).
Previous studies have projected a shortage HIV clinicians.3 Similar to the overall HIV clinician workforce,3 this study shows that FM HIV clinicians are more likely to have been in practice for more than 10 years. FM residency programs should work to assist in filling this shortage by educating residents in HIV care. Unfortunately, while 80% of FM PDs reported a need to modify their curriculum to include more HIV clinical training,7 the same number felt that they lacked faculty with appropriate expertise.7 Thus, training will need to be enhanced for both residents and faculty. In addition to teaching prevention, preexposure prophylaxis, and HIV treatment, educators should collaborate with local and national HIV professional groups and practitioners to acquire the needed knowledge base and develop training tools.
Further understanding family medicine’s role is needed to guide future training efforts. As the distribution and needs of HIV patients evolve, family medicine should be prepared to use its experience managing complex patients to fill in gaps.
References
- Hall HI, An Q, Tang T, et al; Centers for Disease Control and Prevention (CDC). Prevalence of Diagnosed and Undiagnosed HIV Infection—united States, 2008-2012. MMWR Morb Mortal Wkly Rep. 2015;64(24):657-662.
- Balderson BH, Grothaus L, Harrison RG, McCoy K, Mahoney C, Catz S. Chronic illness burden and quality of life in an aging HIV population. AIDS Care. 2013;25(4):451-458. https://doi.org/10.1080/09540121.2012.712669
- Gilman B, Bouchery E, Barrett K, et al. HIV clinician workforce study final report. Report submitted to US Department of Health and Human Services, Health Resources and Services Administration, HIV AIDS Bureau. Cambridge, MA: Mathematica Policy Research; May 2013.
- Carmichael JK, Deckard DT, Feinberg J, et al. Averting a crisis in HIV care: a joint statement of the American Academy of HIV Medicine (AAHIVM) and the HIV Medicine Association (HIVMA) on the HIV medical workforce. June 2009. http://www.idsociety.org/Workforce_Policy/. Accessed September 2, 2016.
- The White House. National HIV/AIDS Strategy for The United States: Updated to 2020. 2015. https://files.hiv.gov/s3fs-public/nhas-update.pdf. Accessed September 9, 2016.
- US Department of Health and Human Services Health Resources and Services Administration. Workforce Capacity in HIV. HRSA Care Action Newsletter. April, 2010. https://hab.hrsa.gov/sites/default/files/hab/Publications/careactionnewsletter/april2010.pdf. Accessed September 2, 2016.
- Prasad R, D’Amico F, Wilson SA, et al. Training family medicine residents in HIV primary care: a national survey of program directors. Fam Med. 2014;46(7):527-531.
- Adams J, Chacko K, Guiton G, Aagaard E. Training internal medicine residents in outpatient HIV care: a survey of program directors. J Gen Intern Med. 2010;25(9):977-981. https://doi.org/10.1007/s11606-010-1398-6



There are no comments for this article.