Background and Objectives: To achieve the goal of 300,000 general practitioners by 2020—an increase of 215,200 in a decade—China is utilizing multiple training pathways. To comprehensively illustrate general practitioner training strategies in China, this article introduces and describes these pathways.
Methods: We used descriptive policy analysis. This involved taking an inventory of existing literature and source documents and developing a model to illustrate pathways for training general practice physicians.
Results: The rural doctor pathway represents rural clinicians who had only basic training and practiced multiple years prior to training reforms. The 3+2 pathway to assistant general practitioners requires 3 years of junior college and 2 years of clinical training. The transfer pathway for current physicians requires 1-2 years of training. The 5+3 pathway comprises 5 years of bachelor of science degree training in clinical medicine and 3 years of standardized residency training. Despite the development of advanced degree programs, their use remains limited.
Conclusions: These pathways illustrate significant heterogeneity in training of general practitioners. Training ranges from a 2-year technical degree to a doctorate with research. Emphasis on the 5+3 track shows promise for China’s goals of improved quality and new goal of 500,000 additional general practitioners by 2030.
As the world’s largest country, the policy initiatives devoted to developing family medicine (hereafter termed “general practice” [the closest translation of the Chinese word quánkē yīxué]), in the second decade of the 21st century in China are unprecedented. In 2010, when there were approximately 84,800 general practitioners (GPs),1 the government announced a goal of achieving 300,000, or 2-3 GPs per 10,000 population by 2020.2 Achieving this goal would require an increase of approximately 215,200 GPs in a decade. Efforts to achieve this goal have progressed, as illustrated by data suggesting there were 209,000 in total, or 1.5 GPs per 10,000 population in 2016.2 On January 24, 2018, the Chinese State Council announced a new goal of 700,000 total GPs in China (5 per 10,000 by 2030), an additional increase of 500,000 over a 10-year period.3
In China, a contemporary issue in family medicine literature concerns the rigor and quality needed for educating such a massive increase in GPs. Wu, et al identify significant differences in the educational qualifications of primary care practitioners relative to geographic distribution.4 They report that the percentage of GPs with 3 or more years of clinical training from 2005 to 2013 was at least 20% higher in urban areas than rural areas. Based on 2016 National Health and Family Planning Commission data, only 0.2% of rural doctors in village clinics hold a BS degree in medicine, while 44.3% of GPs in Chinese community health centers hold a BS in medicine.5
Improved teaching quality has been noted as one of the key issues for advancing general practice as a specialty in China. Based on experience training more than 1,000 general practice trainers and 4,000 GPs from 30 provinces in China through a collaboration between the University of Birmingham and Peking University of Health Sciences, a previous report suggests three priorities for GP training: (1) increasing the number of GP trainers, (2) improving the quality of care in community health centers where GPs typically work, and (3) transitioning to a competency-based rather than knowledge-based curriculum.6
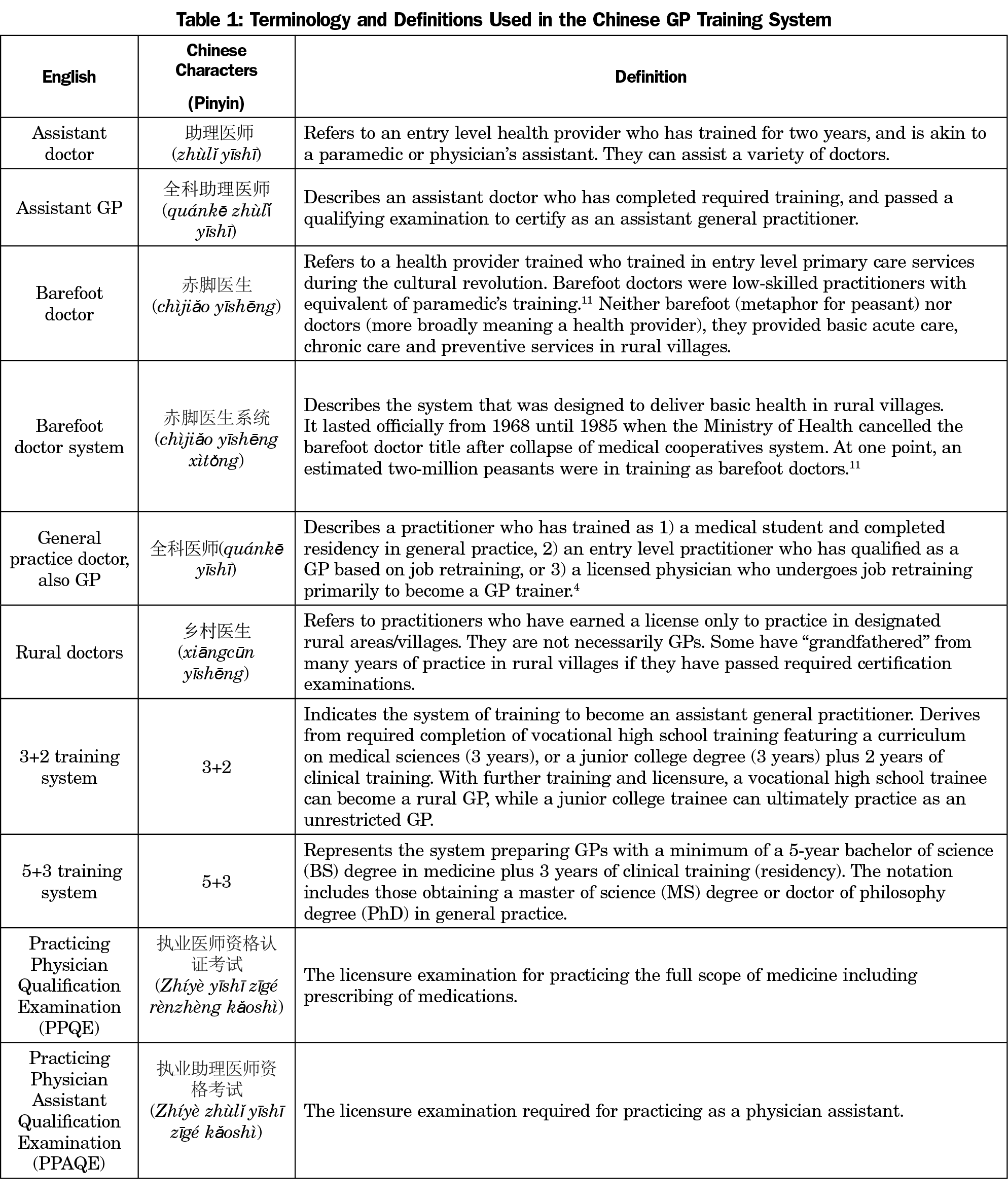
Wu, et al illustrate significant public trepidation with the quality of training.7 They conducted a rigorous mixed-methods study using focus groups and survey methodology in Zhejiang, China, one of the earliest health reform pilot cities implementing general practice. Their qualitative findings illustrate significant distrust of community health services, with the public considering them little more than drug dispensaries, and viewing practitioners as incompetent even for the care of chronic diseases such as hypertension and diabetes. Participants in the study7 pejoratively equated community health services to the system of “barefoot doctors” (chìjiǎo yīshēng), a system of low-skilled practitioners with little more than a paramedic’s training who were deployed during the cultural revolution (Table 1).8-11 Another factor complicating acceptance of general practice can be found in public preferences for hospital care. The Wu, et al survey of 1,248 resondents7 found distrust and lack of confidence in GPs, and patient demand was much higher for hospital-based services than outpatient services. Lack of consistent training of GPs, and training through multiple pathways developed by the government may partly account for lack of public trust and confidence.
Training Pathways to General Practice in China
Wu, et al depict three general practice training pathways: (1) posttransfer training for licensed physicians or assistant doctors to become a GP; (2) general practice training involving a 5-year undergraduate program and 3 years of residency training, and (3) family medicine undergraduate education preparing students for rural practice.4 While a helpful overview, their introduction does not provide full details about the complexity of GP training in China.
In this study, we describe the training pathways to general practice in detail, and how these pathways contribute to fulfilling the aggressive policy of creating access to a GP for the people of China.
We used a descriptive policy analysis approach utilizing three relevant steps as described by Patton and Sawicki12: (1) an inventory phase, (2) a constrained search for alternatives, and (3) preparation of the findings for dissemination. The pathways (ie, outcomes), emphasize the observed policy outcome relative to the importance of teaching GPs. To elucidate the various pathways of training for general practice, in the inventory phase we examined existing literature and searched government and university websites for regulations and policies, and conducted multiple follow-up searches for variations and clarifications. For dissemination, we developed a figure detailing the various pathways, explicated the findings with supporting tables, and interpreted the findings to illustrate how the identified pathways reflect Chinese policy.13
Development of a Comprehensive Overview of the Pathways to General Practice
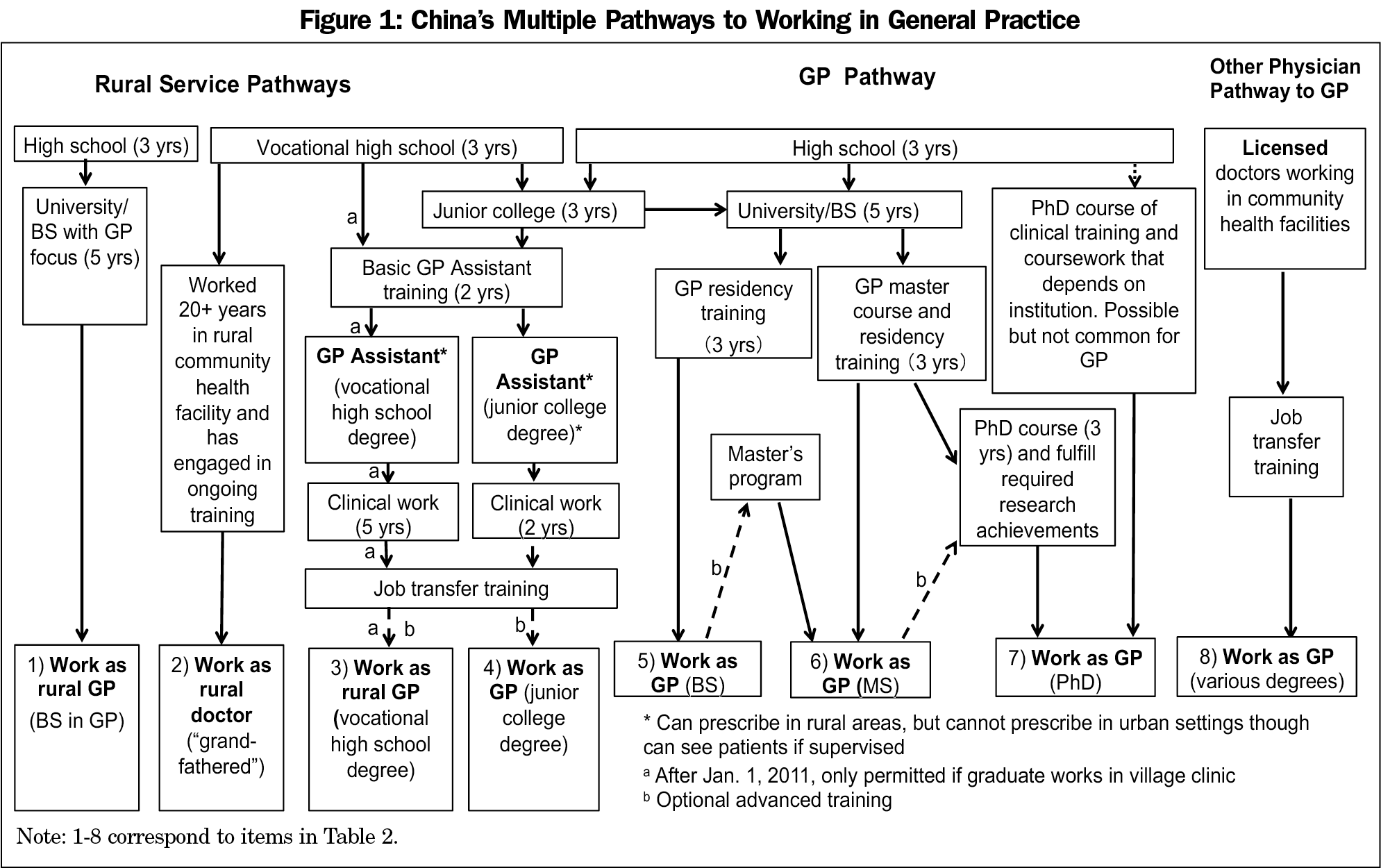
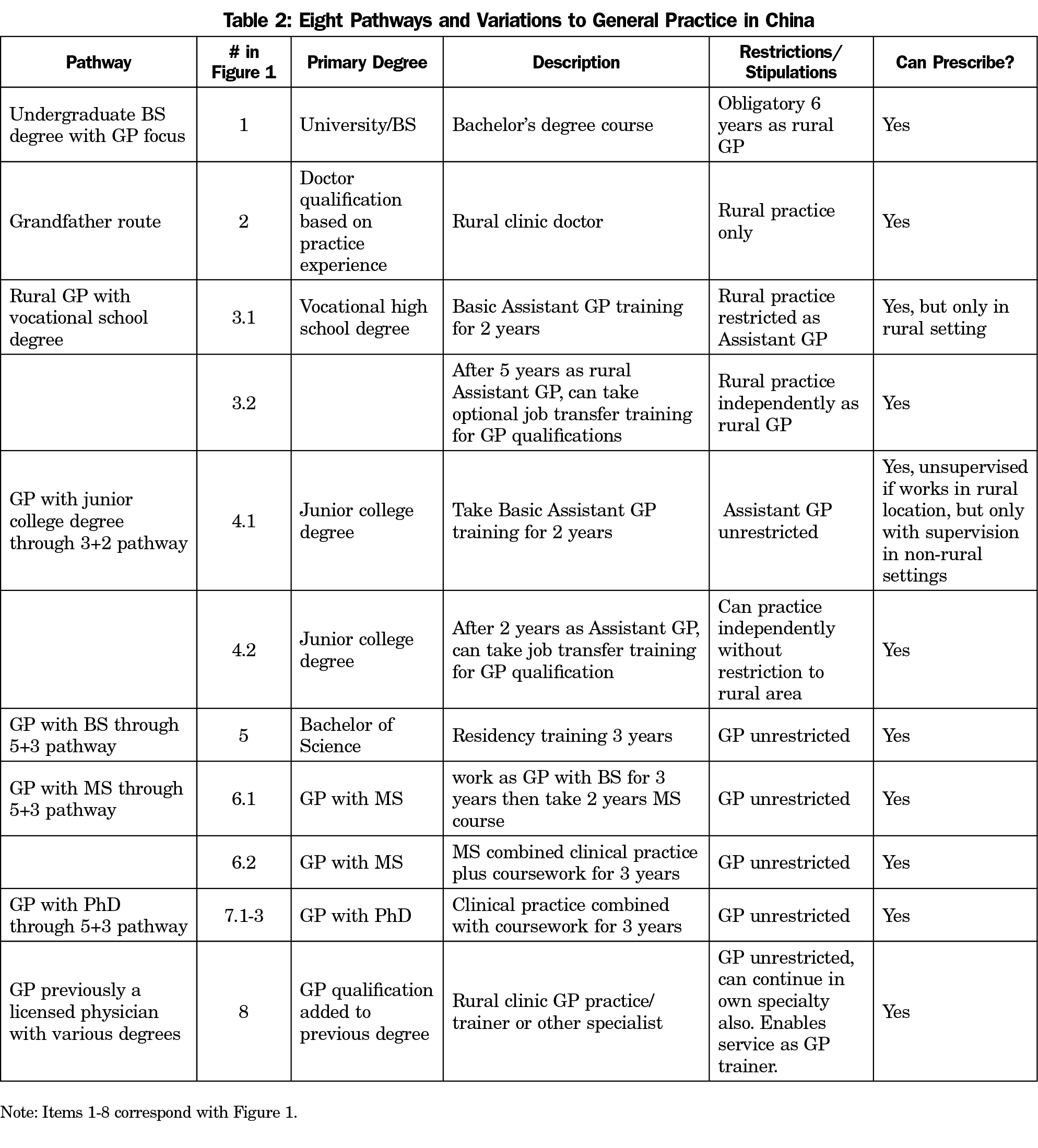
Figure 1 provides a detailed presentation of eight major pathways that historically and currently can be followed to become a GP in China. Table 1 provides definitions of terminology needed for understanding the system.14 Rural doctors can only practice in designated rural areas. They are not necessarily GPs, although they can be. Assistant doctors with training can become assistant GPs, and with further training and certification they can acquire GP status (Table 1). GP status can be attained directly by obtaining a BS in medicine or graduate degree in medicine and completing residency training. Prescribing privileges are separate from certification as an assistant physician.
Pathways to Working in General Practice
Figure 1 is cross-linked with Table 2 to illustrate the multiple pathways to general practice. Although there are many pathways, the training intensity varies dramatically. Becoming a GP does require first completing elementary and middle school. From this common starting point, many pathways emerge.
Terms Used for Describing Generalist Physicians and Assistant Physicians in China
Grasping the Chinese training system requires an understanding of terminology used by the Chinese government (Table 1). A rural GP can refer to both GPs and assistant GPs.15 The system produces assistant GPs (akin to paramedic/physician assistant) under the 3+2 training system, by 3 years of medical sciences curriculum plus 2 years clinical training (Table 1).16-18 The system prepares physician GPs through the 5+3 training system (Table 1); a 5-year bachelor of science degree in medicine plus 3 years of clinical training (residency).16-19
To sit for the medical certification examination, assistant GPs must work 5 years as a clinician after a vocational high school degree, while graduates with a BS in medicine must work as a clinician for 1 year.20 A general practice assistant with a junior college degree who obtains medical certification and completes job transfer training earns the title of GP and the privilege to prescribe anywhere in mainland China.21 A general practice assistant with a vocational high school degree who obtains medical certification earns the privilege to prescribe, but only in rural areas.22
Pathway 1: Designated Undergraduate Medical Degree Focused on General Practice and Mandatory Rural Service Pathway
This pathway involves a free university-level medical education for high school graduates who are usually from poor rural backgrounds, and leads to an undergraduate BS degree in medicine.4 After completing the 5-year university medical education program, graduates need to practice in designated rural areas for at least 6 years (or pay a heavy penalty). However, 3 years of clinical (residency) training count towards the required 6 years.4 This 5-year university program for a BS in medicine emphasizes family medicine/general practice.4 According to Chinese regulations,20,21 after working for 1 year after medical school graduation (minimum BS), trainees who obtain the Practicing Physician Qualification Examination (Zhíyè yīshī zīgé rènzhèng kǎoshì) certification can practice medicine and prescribe medications. After completing 6 years of service in designated rural areas, these GPs can work in both rural and urban settings. Wu, et al report this pathway as unsuccessful in promoting student interest in general practice since a majority of students plan careers other than general practice.4
Pathway 2: Grandfathered Rural Doctors
While not Chinese, we use the term “grandfathered” to describe this pathway, as many use this term in English. This historically-rooted pathway describes how practitioners of various backgrounds persist and become certified rural doctors. Some rural practitioners, both those who originally trained as barefoot doctors, and others who completed medical studies before entering rural practice, continue practicing in rural China today.
Designation as a rural doctor14 requires one of three qualifications: (1) higher than vocational high school degree for medicine, (2) worked more than 20 years in a rural health department, or (3) participated in a training program and earned a training certificate.23 These rural doctors can prescribe medicines included in an official list approved for prescription by rural doctors.21 The government instituted a requirement for rural practitioners to pass the examination for a Physician Assistant Medical Certificate in 1999, but many rural doctors could not pass the examination. Requirements for rural practice became stricter with release of the Rural Doctor Practice Regulations issued August 2, 2005 that dictates all rural doctors need to obtain the Practicing Physician Assistant Qualification Examination (Zhíyè zhùlī yīshī zīgé kǎoshì) certificate.23 Since January 1, 2011,15 physicians already working in a rural setting also need to pass the Rural Physician Practice Certificate every 5 years to continue clinical practice.
Pathway 3: Vocational High School Degree to General Practitioner Assistant and Optionally to Rural General Practitioner (3+2 Designation)
Pathway 3.1: Assistant General Practitioner With Vocational High School Degree in Rural Area (3+2 Designation). According to the Secondary Vocational School Professional Catalogue,24 graduates with a vocational high school degree can only practice in rural settings. For an applicant with a vocational high school medical degree seeking to qualify as a rural GP, regulations stipulate completion of 2 years of basic assistant GP training.25 The training includes 82 weeks of clinical training, 16 weeks of practice in community health facilities, and 2 weeks of theoretical learning.26 According to the Practicing Physician Law20 and Prescription Management Procedures requirements, an applicant needs to pass the Practicing Physician Assistant Qualification Examination and meet facilities management requirements27 to qualify to prescribe medications in a rural setting.21
Pathway 3.2: Rural General Practitioner With a Vocational High School Degree (3+2 Designation). With sufficient training, assistant GPs can practice independently in designated rural areas. After working as an assistant GP in a rural setting for 5 years, passing the Practicing Physician Qualification Examination qualifies one to practice as a rural GP20 who can prescribe from the list of rural practice-approved medications.21
Pathway 4: Junior College Degree to Assistant General Practitioner with Optional Pathway to GP
Pathway 4.1: Assistant GP With Junior College Degree (3+2 Designation). After completing a junior college degree program, an assistant GP can qualify as a rural GP by completing 2 years of basic assistant GP training.25 Passing the Practicing Physician Assistant Qualification Examination earns the privilege to prescribe medications in rural settings.20,21 This pathway resembles the pathway for an assistant GP with vocational high school degree, but a junior college degree graduate who earns these qualifications can practice in rural or urban settings. Chinese regulations permit prescribing privileges for rural general practice, though in urban settings, prescribing medications requires supervision.21
Pathway 4.2: General Practitioner With Junior College Degree (3+2 Designation). According to the Practicing Physician Law20 and Prescription Management Procedures requirements,21 working as an assistant GP in a rural setting for 2 years meets the requirements to take the Practicing Physician Qualification Examination. Passing the examination earns qualification as a GP with the privilege to independently practice and prescribe medications in rural and urban settings.
Pathway 5: General Practitioner With Bachelor of Science degree (5+3)
Becoming a GP with an undergraduate BS degree in medicine represents the main pathway under the 5+3 system. Passing the Practicing Physician Qualification Examination qualifies the GP to independently practice and prescribe medication without restriction on location of practice. Residency training includes 27 months of clinical training at tertiary care hospitals and 6 months of practice in community health facilities.28
Advanced Degrees in General Practice. Under the 5+3 system, GPs can pursue research training for a master of science (MS) or PhD degree in general practice after clinical practice or through combined degree programs. The number of participants choosing these pathways remains very small.
Pathway 6: General Practitioner With Master of Science Degree
Pathway 6.1: General Practitioner With BS in Medicine Works for 3 Years, Then Completes an MS Program. According to the requirements of Peking University Health Science Center, a GP with BS in medicine who works for 3 years can pursue this pathway. The program requirements include theoretical studies and 1 year of clinical training at tertiary care hospitals.
Pathway 6.2: General Practitioner Combined Master of Science Course and Residency Training. In the combined residency and MS degree program, a student with a BS in medicine can complete a combined residency and MS program in three years. The master’s course requires theoretical learning and residency training. Upon completion of requirements, graduates obtain a master’s degree, postgraduate diploma for the residency training, a medical license, and general counseling certificate.
Pathway 7: General Practitioner With a Doctor of Philosophy
Pathway 7.1: General Practitioner With MS Works First, Then Completes PhD Program. A graduate with an MS who works clinically as a GP can return to studies for a doctoral course and earn a PhD in general practice.
Pathway 7.2: General Practitioner With MS Who Completes Doctor of Philosophy Program Directly. A GP with an MS can advance directly into a PhD course that generally takes 3 additional years. At Peking University Health Science Center, the PhD candidate must complete theoretical learning through course work and certain research requirements.29
Pathway 7.3: Combined Degree Program From Undergraduate to Doctor of Philosophy in General Practice. This comprehensive combined degree program involves undergraduate and graduate medical coursework, clinical training, and completion of research requirements. The detailed contents of this pathway depend on the institution.
Pathway 8: Transfer Training Pathway for Community Hospital-Based Physicians to Become General Practitioner Trainers
The transfer training pathway allows licensed doctors working in community health facilities to undergo GP transfer training for 1-2 years.30 The training lasts more than 1 year and includes coursework for more than 1 month, clinic training more than 10 months, and primary practice for more than 1 month as a fellow or intern in a community health center/station. Completing these requirements provides qualification as a GP30 with full privileges to prescribe medications.21 After training, most return to their previous posts and become GP trainers in community health facilities.4 This pathway is needed to prepare other specialists as GP trainers so they can teach in general practice departments. Within general hospitals in China, general pratice departments require staffing by five GPs including a director qualified as a GP.31
Distribution of Rural Practitioners in Village Clinics and Community Health Centers According to Training Level and Location of Practice
To provide a window on the distribution of GPs in China according to the different pathways illustrated in Figure 1, we examined official government data from 2015. In 2015, only 5 years after announcing the aggressive policy to more than triple the size of GPs in a decade, the Chinese government reported there were 188,649 GPs,5 an increase of 103,849 GPs in 5 years. While behind pace for achieving the target of 300,000 GPs in 10 years, the growth was remarkable.
Table 3 presents the distribution in 2015 of rural practitioners including doctors and assistant doctors by their training level and practice in village clinics or community health center in 2015.5 Compared to community health centers practitioners (73,288), practitioners in village clinics (309,923) numbered more than 4.2 times greater. The table suggests some practitioners, presumably those who grandfathered into practicing, did not even complete a high school degree. Vocational high school degree-holding practitioners numbered the greatest among all practitioners, accounting for 51.9%. In contrast, 76% of community health center practitioners had a junior college or college degree. While 1,539 practitioners had an MS degree, they worked exclusively in community health centers. The data convincingly demonstrate higher education levels of practitioners working in community health centers than in village clinics.
This study provides a detailed representation of eight pathways for becoming a GP in China. Training ranges from a 2-year technical degree (with subsequent additional retraining and some restrictions) to a doctorate with research. These findings corroborate and expand upon three pathways described by Wu, et al: (1) the undergraduate medical education for rural practice, here, pathway 1; (2) retraining, here, pathways 2, 3.2, 4.2, and 8; and (3) residency training, here, pathway 5.4 This analysis adds the assistant GP pathways 3.1 and 4.1, and advanced-GP MS and PhD pathways 6.1, 6.2, 7.1, 7.2, and 7.3. The details provided about historical differences and explication of the advanced pathways account for the differences with the Wu, et al description.4 While the described research pathways remain new, they represent pathways critical for general practice’s academic advancement.
This analysis illustrates the variations in the pathways to becoming a GP. These findings suggest significant flexibility for assistant GPs and licensed physicians working in community health centers to pursue training to qualify as GPs. The multiple pathways help expound how the Chinese government has added significant numbers of GPs in a short time since 2010. These pathways further show how aggressively the Chinese government created pathways and training systems for achieving the laudable goal of rapidly increasing the number of GPs.
Transfer training provides an important quick solution for rapidly increasing GP numbers, since retraining requires much less time than training new GPs. Starting at the beginning of the training process requires a minimum of 5 years for a GP assistant (3+2 pathway) and 8 years (5+3 pathway) for a GP. The government actively encourages transfer training of assistant GPs to become GPs, eg, pathways 3.1 to 3.2 and 4.1 to 4.2, and for physicians in rural community health centers to engage in transfer training. For example, the General Practitioner Training and Use of Incentives Policy3 encourages assistant GPs working in rural settings to pursue transfer training.32
The aggressive approach of expansion has led to problems in quality. Public distrust of general practice for care even of common problems7 looms as a significant challenge. The proactive emphasis on the 5+3 model of medical education suggests the next generation of GPs will benefit from better quality training.33 Moreover, the flexibility in training pathways to date suggests that faculty development and professional medical education can be utilized to improve the education of GPs who have completed less intensive training previously.
Implications for the Training of General Practitioners in China
These findings represent critical context for medical educators engaged in expanding general practice training capacity in China. China utilizes multiple pathways that differ from many countries. International educators teaching in China should familiarize themselves with these pathways to frame their teaching. A McKinsey report paints an optimistic picture for achieving success in health care reforms, but identifies as challenges sustainable funding for health care, long-term care and advances in institutional capabilities.34 A focus on training in the community may yield a better understanding of community-based training needs35 and research.
Overcoming Lack of Trust
This analysis illustrating significant heterogeneity in the quality in GP training approaches helps explain in part why GPs face a significant challenge for earning the public’s trust.7,33,36,37 We agree with Wu, et al,7 on the need to build on positive public perceptions about primary care providers’ value as a trusted source for referral, drug dispensing, managing chronic diseases, and providing patient education. Trainees may benefit from discussion on how to advocate their skills as providers of choice for first-contact care to patients.
Future Research
Future research could address even more comprehensively specific competencies and skills of GPs on the different pathways relative to the health needs of the communities served. Changes in medical education and GP curricula will likely continue. Wang, et al report that many leading institutions in China—18 at the time of publication in 2015—were trialing an 8-year medical curriculum.38 It remains to be seen how this will affect GP training, but it could lead to additional training pathways or cessation of current pathways. Comparing measures of morbidity and mortality across pathways of preparation and population densities (rural to urban) could demonstrate the added value of a GP-based training system for a positive impact on health outcomes.
This study illustrates how the Chinese government engineered multiple policies and pathways for working in general practice. The ambitious policy created considerable variation in the rigor of GP training. Public concern about care quality and trust, and student concern about prestige of the discipline will likely persist if root causes of inconsistent quality remain neglected. We hope this analysis will inform collaborations that will support the government’s goal of 500,000 new GPs, for a net GP workforce of 700,000, or 5 GPs per 10,000 population by 2030.
Acknowledgments
Lilly Pritula provided invaluable support in manuscript preparation.
Financial support: This research was made possible by the generous support of Dr Fetters by (1) the Fulbright Program and was conducted while he served as Distinguished Chair in the Social Sciences at Peking University Health Science Center from September 2016 to January 2017, and (2) University of Birmingham, Teaching Fund for General Practice development in China. The Research Fund for Youth, Institute for Medical Humanities, Peking University provided support for Dr Qi Chen. November 2016.
Presentations: This study was presented at the Michigan Medicine-Peking University Health Science Center Joint Institute for Translational and Clinical Research, Eighth Annual Symposium, October, 2018.
References
- Ge Y, Xu J, Zhou Y, Qian D. History and present situation of development of general practice in China. Chin Gen Pract. 2013;16(7):2201-2203.
- Xinghua Z. The speed of General Practioner Training raise again. (Chinese). Guangming Daily. 2018. http://www.gov.cn/zhengce/2018-01/26/content_5260888.htm. Accessed January 30, 2018.
- General Office of the State Council of the People’s Republic of China. Opinions of the General Office of the State Council on Reforming and Improving General Practitioner Training and Incentive Mechanisms. (Chinese). http://www.gov.cn/zhengce/content/2018-01/24/content_5260073.htm. Accessed January 30, 2018.
- Wu D, Lam TP. At a crossroads: family medicine education in China. Acad Med. 2017;92(2):185-191. https://doi.org/10.1097/ACM.0000000000001512
- National Health and Family Planning Commission. Chinese Yearbook of Health and Family Planning in 2016. Beijing: China Union Medical College Press; 2016.
- Fetters MD, Chi C, Hu L. Hu, and L. Insights on developing general practice education in China. Acad Med. 2017;92(10):1365. https://doi.org/10.1097/ACM.0000000000001886
- Wu D, Lam TP, Lam KF, Zhou XD, Sun KS. Public views towards community health and hospital-based outpatient services and their utilisation in Zhejiang, China: a mixed methods study. BMJ Open. 2017;7(11):e017611. https://doi.org/10.1136/bmjopen-2017-017611
- Revolutionary Health Committee of Hunan Province. A Barefoot Doctor’s Manual. The American Translation of the Official Chinese Paramedical Manual. Philadelphia: Running Press; 1977.
- Sidel VW. The barefoot doctors of the People’s Republic of China. N Engl J Med. 1972;286(24):1292-1300. https://doi.org/10.1056/NEJM197206152862404
- Lampton DM. The politics of medicine in China: the policy process, 1949-1977. Boulder, CO: Westview Press; 1977.
- Zhang D, Unschuld PU. China’s barefoot doctor: past, present, and future. Lancet. 2008;372(9653):1865-1867. https://doi.org/10.1016/S0140-6736(08)61355-0.
- Patton CV, Sawicki DS. Basic methods of policy analysis and planning. 2nd ed. Englewood Cliffs, NJ: Prentice Hall; 1993.
- Dunn, WN. Public Policy Analysis, 5th ed. Boston: Pearson; 2012.
- National Health and Family Planning Commission of the People’s Republic of China. Guiding Opinions of the General Office of the State Council on Further Strengthening the Team Building of Rural Doctors (Chinese). 2011. http://www.nhfpc.gov.cn/fzs/s9660/201107/67df29b85d944ed09ccb745db4875f38.shtml. Accessed July 25, 2018.
- Primary Health Department. Implementation Opinions of the General Office of the State Council on Further Strengthening the Construction of Rural Doctors. (Chinese). 2015. http://www.nhfpc.gov.cn/jws/s3581/201503/02befee5e0234bf1bda7a43ef60aaa9b.shtml. Accessed July 19, 2019.
- National Health Education. Opinions on the establishment of residents’ standardized training program. (Chinese). [Accessed 2018 Feb 4]. Available from: http://www.gov.cn/gzdt/2014-01/17/content_2569096.htm. Accessed February 4, 2018
- Liu Z. Let more “gatekeepers” guard the health of the people. From People’s Political Consultative Conference Newspaper. July 9, 2018.
- Li D. Training doctors for primary care in China: transformation of general practice education. J Family Med Prim Care. 2016;5(1):1-2. https://doi.org/10.4103/2249-4863.184614. – JA.
- Ministry of Education. Opinions of the Ministry of Education on improving the “5+3” Integrated Medical Personnel training. (Chinese). http://www.gov.cn/xinwen/2017-07/04/content_5207871.htm. Accessed Feb 3, 2018.
- National People’s Congress Standing Committee. 2005. The law for People’s Republic of China physician practitioners. (Chinese). http://www.gov.cn/banshi/2005-08/01/content_18970.htm. Accessed February 3, 2018.
- Ministry of Health of the People’s Republic of China. Prescription management methods. (Chinese). 2007. http://www.gov.cn/flfg/2007-03/13/content_549406.htm. Accessed February 3, 2018.
- People’s Republic Ministry of Education. The notice of the Ministry of Education on Printing and Distributing the Professional Catalogue of Secondary Vocational Schools. 2010 Revision.(Chinese). http://old.moe.gov.cn//publicfiles/business/htmlfiles/moe/moe_722/201005/xxgk_87384.html. Accesssed July 19, 2018.
- State Council State Department of People’s Republic of China. 2005. Rural doctor practice regulations. (Chinese). http://www.gov.cn/banshi/2005-08/02/content_19251.htm. Accessed February 3, 2018
- People’s Republic Ministry of Education. Professional Catalogue of Secondary Vocational Schools. Revised in 2010. (Chinese). http://old.moe.gov.cn//publicfiles/business/htmlfiles/moe/moe_722/201005/xxgk_87384.html. Accessed July 19, 2018.
- National Health and Family Planning Commission, National Development and Reform Commission, Ministry of Education, Ministry of Finance, Ministry of Human Resources and Social Security, Administration of Traditional Chinese Medicine, 2016. Notice on printing and distributing the Assistant General Practitioners’ Training and Implementation Opinion (Trial Implementation). (Chinese). http://www.nhfpc.gov.cn/qjjys/s3593/201606/ac7465a778f24fcd9a47f7cec54a3974.shtml. Accessed February 3, 2018.
- Ministry of Health of the People’s Republic of China. Notice of the Ministry of Health on Printing and Distributing the Standards for Assistant General Practitioners Training (Trial). 2012. (Chinese). http://www.nhfpc.gov.cn/qjjys/s3593/201209/6f495e57aaaa4f1886fffff15de2e71f.shtml. Accessed July 28, 2018.
- Ministry of Health of the People’s Republic of China. Order of the Ministry of Health No. 53. (Chinese). http://www.gov.cn/flfg/2007-03/13/content_549406.htm. Accessed July 25, 2018.
- National Defense Office Science and Education of People’s Republic of China. 2014 Resident Standardized Training Contents and Standards (Trial). Issued August 26, 2014. (Chinese). http://www.nhfpc.gov.cn/ewebeditor/uploadfile/2014/08/20140825155108969.PDF. Accessed July 19, 2018.
- Graduate School Health Science Center of Peking University. Peking University School of Medicine graduate with the same level of academic personnel to apply for a doctorate or master’s degree. (Chinese). http://gratest.bjmu.edu.cn/website/xwtdxl/ff808081512eda2e0151336cf8b90004.htm. Accessed February 4, 2018.
- General Office of the Ministry of Health. Opinions of the General Office of the State Council on Reforming and Improving General Practitioner Training and Incentive Mechanisms (Chinese). 2011. http://www.gov.cn/gzdt/2011-01/11/content_1782252.htm. Accessed February 3, 2018.
- National Defense Office Science and Education of People’s Republic of China. 2018. Notice on Printing and Distributing the Standards for the Establishment of the Standardized Training Base for Residents (Chinese). 2018. http://www.nhfpc.gov.cn/qjjys/s3593/201809/951a65647c41459b858ccf1c26fc1acb.shtml. Accessed October 5, 2018.
- Ministry of Health. Notice of the General Office of the Ministry of Health on Printing and Distributing the Outline of the Training of General Practitioners in Primary Health Care Institutions (Chinese). 2011. http://www.moh.gov.cn/qjjys/s3593/201101/cc492eb3eda04fe0909a0b0b61acbc36.shtml. Accessed July 19, 2018.
- Wu D, Lam TP. Underuse of Primary Care in China: The Scale, Causes, and Solutions. J Am Board Fam Med. 2016;29(2):240-247. https://doi.org/10.3122/jabfm.2016.02.150159
- Süssmuth-Cyckerhoff C, Wang J. China’s health care reforms. Health International. No.10, 2010. https://www.mckinsey.com/~/media/mckinsey/dotcom/client_service/healthcare%20systems%20and%20services/health%20international/hi10_china_healthcare_reform.ashx. Accessed July 29, 2018.
- Kidd M. From the president: China and the rise of the family doctor. Wonca Global Family Doctor. April, 2014. http://www.wonca.net/News/FromthePresidentChinaandtheriseofthefamilydoctor.aspx. Accessed July 29, 2018.
- Wu D, Lam TP, Lam KF, Zhou XD, Sun KS. Health reforms in china: the public’s choices for first-contact care in urban areas. Fam Pract. 2017;34(2):194-200. https://doi.org/10.1093/fampra/cmw133
- Wee SL. China’s health care crisis: lines before dawn, violence and ‘no trust.’ New York Times. September 30, 2018. https://www.nytimes.com/2018/09/30/business/china-health-care-doctors.html?smprod=nytcore-ipad&smid=nytcore-ipad-share. Accessed October 3, 2018.
- Wang Z, Yin Z, Wei Y, Liu F, Yang J. The expansion of 8-year medical training programs in China: a status report. Med Educ Online. 2015;20:10.3402/meo.v20.25890.



There are no comments for this article.