The majority of health care in the United States is provided in community settings.1 Since most patients receive health care and most physicians practice outside of academic health centers, effective medical education requires medical students to train in the community with community-based physician preceptors. Recruiting and retaining an adequate number of preceptors is increasingly challenging, especially for family medicine educators.2 In many ways, the community preceptor shortage is emblematic of the larger physician shortage, with many of the same root causes.3 Family physicians are seeing more complicated patients in shorter periods of time with increased demands for documentation and productivity.4 Many clinical faculty report that using an electronic health record is burdensome, resulting in decreased enthusiasm for teaching and decreased teaching time.5 These demands contribute to physician burnout, which leads to early retirement or career change, with a decrease in the clinical and educational workforces.6-8 As medical educators and policy makers seek to respond to the shortage of physicians3 with new medical schools, increasing class sizes, and added programs for advanced-practice clinicians, larger numbers of students need placement with community-based preceptors, leading to competition between and within academic health centers.
Even when motivated to teach, physicians encounter significant barriers to teaching while seeing patients. Having a student is estimated to add 30 to 60 minutes to a typical preceptor’s workday.9-11 Preceptors face challenges with scheduling and may not have enough physical space to comfortably host a student.12 Some physicians report seeing fewer patients when students are present,13 which impacts clinical productivity and potentially compensation. Some physicians express concern that they are not skilled educators and worry about negative interactions with students, including communication difficulties.14 Inadequate academic recognition can cause community-based faculty to feel like second-class citizens, particularly in the realm of promotion.15 Despite these barriers, many community preceptors teach because they believe it is essential to contribute to the future of the medical profession and they enjoy the enthusiasm of students.14,16-18 Having students improves physicians’ lifelong learning, and patients report increased respect for doctors that teach students.4
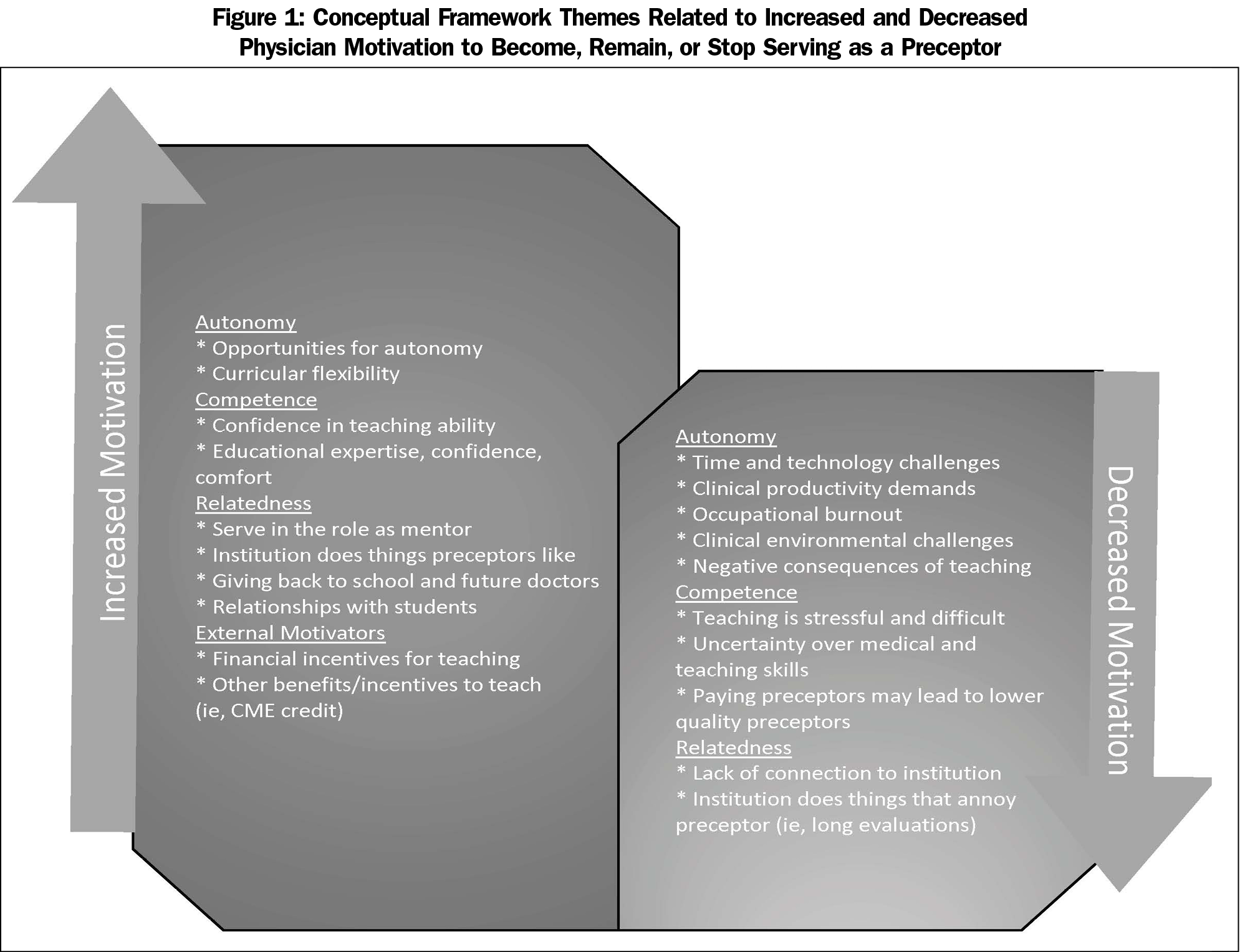
Understanding the motivations of physicians who precept is crucial to ensuring an adequate number of placement opportunities for students. Self-determination theory (SDT) posits that people act in response to a combination of intrinsic and extrinsic motivations.19 While people are intrinsically motivated to engage in activities they find personally interesting, they also respond to external incentives and penalties to complete less interesting tasks. Extrinsic motivation is more effective when it becomes internalized, which is impacted by socialization.19, 20 SDT proposes that autonomy (the opportunity to control one’s actions), competence (the self-perceived ability to perform or complete an act), and relatedness (the sense of affiliation or belonging to a group) are basic psychological needs that must be satisfied to enhance motivation and experience ongoing well-being and integrity.19 While self-determination theory has been used to guide faculty on how to motivate medical students,21,22 it has not been used to evaluate the perspectives of physicians who teach students in community-based settings. Using the framework of SDT, we sought to explore family physicians’ perspectives on serving as a clinical preceptor and explain why family physicians become and remain preceptors, hence our study entitled “Community Preeptor Perspectives on Recruitment and Retention” (CoPPRR).
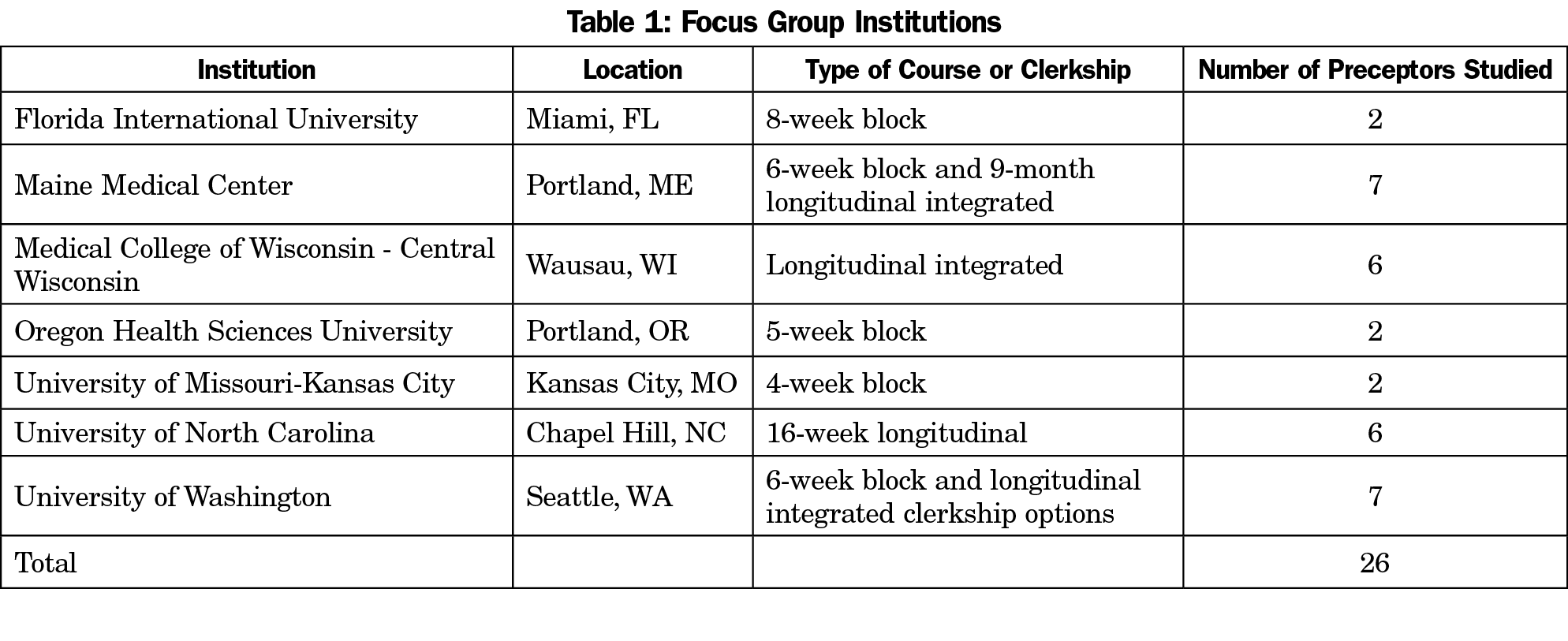
The research team included members of the steering committee for the Society of Teachers of Family Medicine (STFM) Medical Student Education Collaborative (MSEC) with support from the STFM Foundation Project Fund. The University of Washington Institutional Review Board (IRB), with additional review by the IRB at the other participating institutions, reviewed and exempted the study. The research team invited STFM MSEC steering committee members to facilitate focus groups and seven sites were chosen to represent program diversity nationally. We conducted focus groups at seven distinct and geographically diverse academic health centers in the United States (Table 1). Focus group participants were family physicians and preceptors in family medicine courses at the participating medical schools.
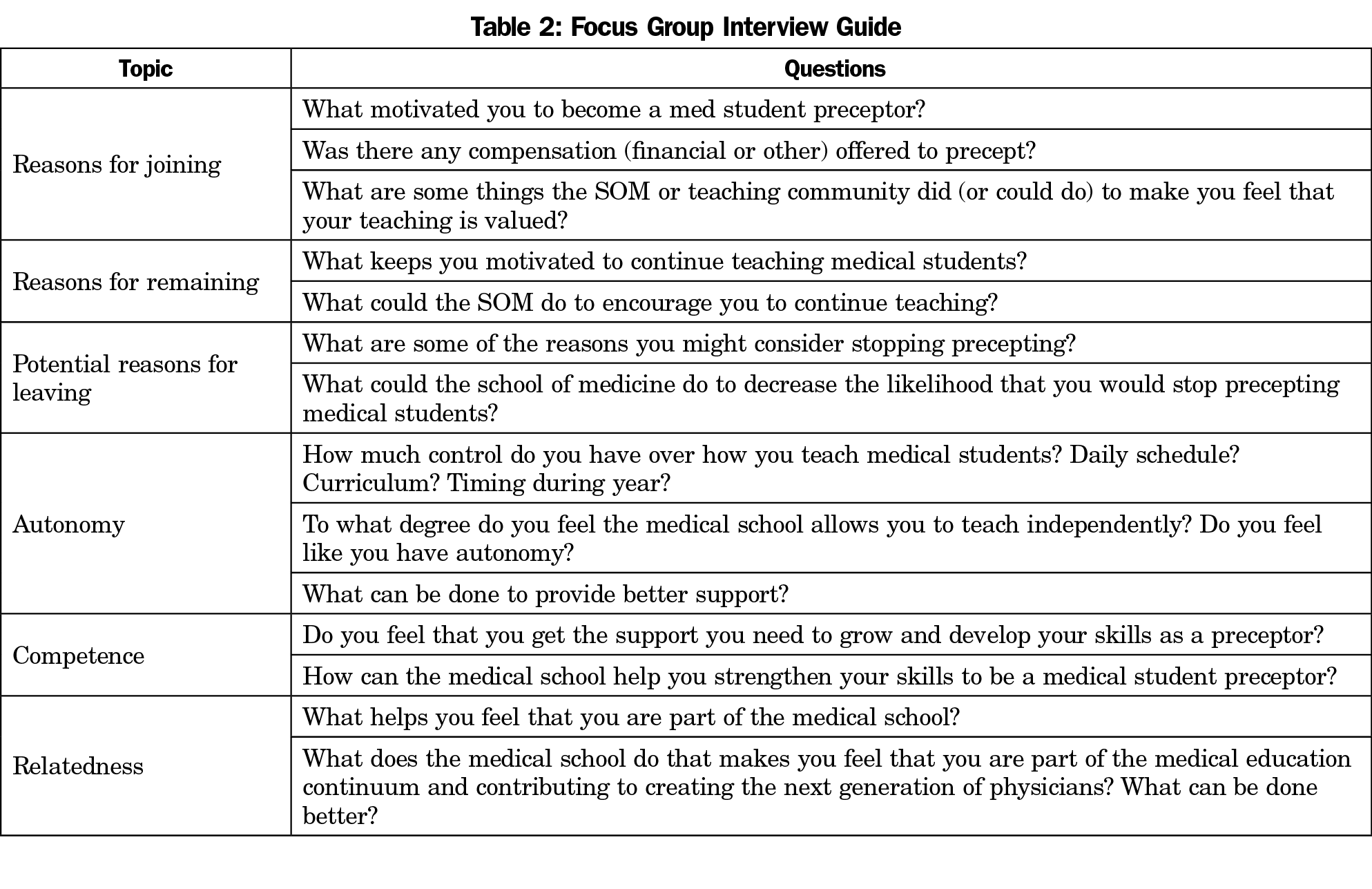
The research team member at each site sent an email invitation to their distribution list of current, former, and potential community preceptors. Recruitment was a challenge, with invitations sent to over 100 family physicians, and only 26 individuals being able to participate. While attempts were made to include family physicians who have chosen not to precept medical students, only current and former preceptors responded to the invitation to participate. Eligible and interested participants provided written informed consent and answered demographic questions. Focus groups occurred in the fall or winter of 2016. Focus groups were conducted by the local research team member using a semistructured interview guide (Table 2) developed by the research team employing the framework of SDT to probe barriers and facilitators to precepting. Research team members responsible for leading the focus groups conferred by conference call in advance to agree on a common approach to facilitation; no additional formal facilitator training occurred.
Interviews were audio recorded and transcribed by a transcription service with the removal of all personal identifying information. Data were uploaded to and analyzed with Dedoose version 7.0.23 (SocioCultural Research Consultants, Los Angeles, CA).
Study authors (S.M., M.H., P.L., J.P.) reviewed transcripts from institutions other than their own and individually coded key excerpts with themes relevant to SDT. These themes were iteratively refined by group discussion and consensus and further organized into overarching themes, which were themselves further refined to achieve final group consensus on wording and assessed for face validity. These overarching themes were mapped within the conceptual framework of SDT.
A total of 26 community preceptors participated in the focus groups, which ranged in size from two to seven participants (Table 3). Most participants were male (n=19, 73%) with an average age of 46.8 years (SD 11.9). Participants had been precepting for an average of 12 years with a range of 1 to 30 years. While only one preceptor worked in a solo practice, five (19%) were the only preceptor at their location. About one-third of the focus group participants worked with more than one medical school (n=8, 31%) and most worked with other health professions students (n=19, 73%). Of those who had other students, half had multiple students at the same time. Four preceptors (15%) reported a requirement to precept as a condition of employment, and five (19%) reported receiving compensation for precepting.
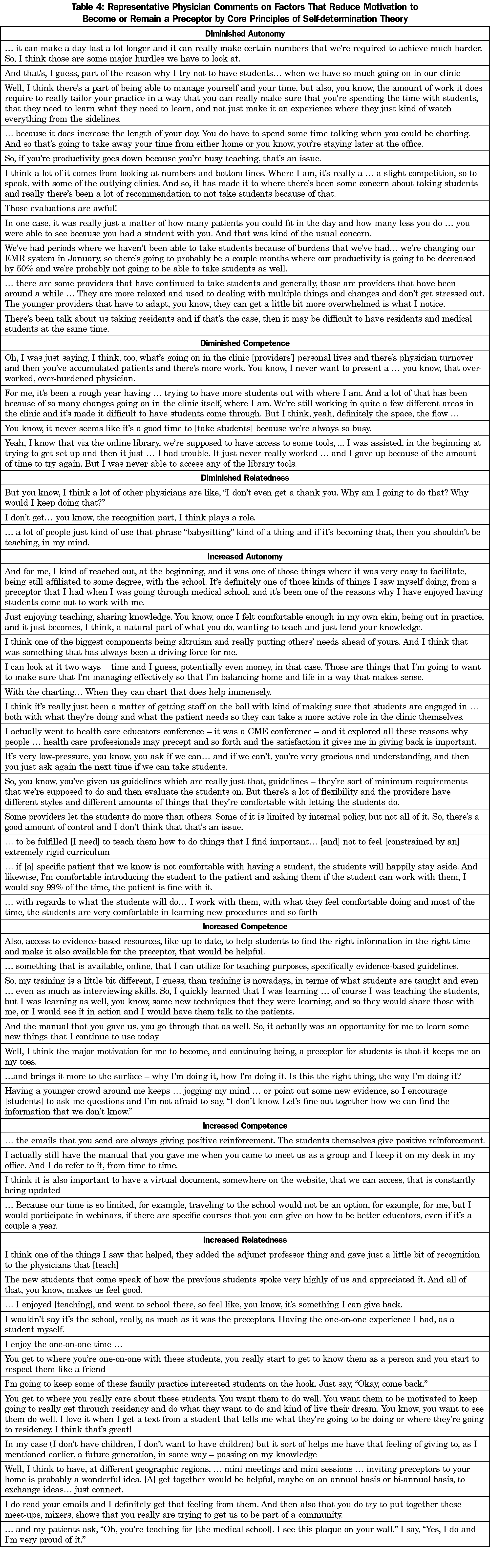
From focus group transcripts, 774 excerpts were coded and grouped into themes based on the SDT conceptual framework of factors that increased and decreased motivation to teach (Figure 1). All identified themes are shown in Figure 1. Participant comments are aligned with SDT themes in Table 4.
One of the core psychological needs according to SDT is autonomy. Preceptors reported a desire for flexibility in the way they interact with students.
So, you know, you’ve given us guidelines which are really just that, guidelines – they’re sort of minimum requirements that we’re supposed to do and then evaluate the students on. But there’s a lot of flexibility and the providers have different styles and different amounts of things that they’re comfortable with letting the students do.
… to be fulfilled [I need] to teach them how to do things that I find important… [and] not to feel [constrained by an] extremely rigid curriculum.
Another core psychological need, according to SDT, is to feel competent. Preceptors reported one of the benefits of precepting is keeping current on medical knowledge.
So, I quickly learned that I was learning … of course I was teaching the students, but I was learning as well, you know, some new techniques that they were learning.
Well, I think the major motivation for me to become, and continuing being, a preceptor for students is that it keeps me on my toes.
In addition to providing quality patient care, preceptors reported that efforts to maintain competency with their teaching skills encouraged them to continue to precept medical students. Their preferred methods of skills development were variable.
I actually still have the [teaching] manual that you gave me when you came to meet us as a group and I keep it on my desk in my office. And I do refer to it, from time to time.
… Because our time is so limited…traveling to the school would not be an option… for me, but I would participate in webinars, if there are specific courses that you can give on how to be better educators, even if it’s a couple a year.
The final core psychological need is relatedness. Precepting allowed physicians to give back to their home institution and mentor students throughout their training. Serving as a preceptor satisfied a personal sense of obligation to give back to the medical profession.
… I enjoyed [teaching], and went to school there, so feel like, you know, it’s something I can give back.
In my case, I don’t have children, I don’t want to have children, but it sort of helps me have that feeling of giving to, as I mentioned earlier, a future generation, in some way – passing on my knowledge.
You get to where you really care about these students…I love it when I get a text from a student that tells me what they’re going to be doing or where they’re going to residency. I think that’s great!
Preceptors also valued concrete (extrinsic) rewards for teaching, including academic titles, certificates, and continuing medical education (CME) credit given for teaching,
…having a card from [the medical school] saying that I’m a professor… And I keep that in my wallet, but I don’t think I’ve ever shown a single person, but that actually helps sort of somehow having a card, with your title on it, means something.
Focus group participants were asked for reasons why they have stopped precepting, or reasons other community preceptors may choose not to precept. They identified concerns that teaching takes time away from other personal and professional obligations (which results in diminished autonomy).
… because it does increase the length of your day. You do have to spend some time talking when you could be charting … and you’re staying later at the office.
…if your productivity goes down because you’re busy teaching, that’s an issue.
Physicians reported factors that result in them questioning their competence as a community preceptor, often due to their environment. These situations have led them to stop precepting for a period of time or for some, altogether.
There’s physician turnover and then you’ve accumulated patients and there’s more work. You know, I never want to present a … you know, that over-worked, over-burdened physician.
We’ve had periods where we haven’t been able to take students because of burdens that we’ve had… we’re changing our EMR system in January, so there’s going to probably be a couple months where our productivity is going to be decreased by 50% and we’re probably not going to be able to take students as well.
For me, it’s been a rough year… trying to have more students out with where I am… We’re still working in quite a few different areas in the clinic and it’s made it difficult to have students come through.
Academic health centers themselves may contribute to a preceptor’s diminished sense of proficiency. Some preceptors reported struggling with using an institution’s educational technology, lacking awareness of the learning objectives for the clinical experience, or lacking perspective on how their teaching fits into the overall medical school curriculum.
I know that via the online library, we’re supposed to have access to some tools, ... I was assisted, in the beginning at trying to get set up and then it just … I had trouble. It just never really worked … and I gave up because of the amount of time to try again. But I was never able to access any of the library tools.
I’m still not 100% sure what the new curriculum is and were there really any major changes …and if we’re supposed to be teaching them to a certain goal, I’m not sure really what my part is in this new curriculum.
Participants also expressed that a lack of a relationship with students results in a decreased desire to continue to precept.
But you know, I think a lot of other physicians are like, “I don’t even get a thank you. Why am I going to do that? Why would I keep doing that?”
… a lot of people just kind of use that phrase “babysitting” kind of a thing and if it’s becoming that, then you shouldn’t be teaching, in my mind.
Family physicians are motivated to serve as community preceptors for a variety of reasons. Our results suggest relating efforts to recruit and retain preceptors to the concepts of SDT, namely autonomy, competency, and relatedness, has potential to strengthen preceptor networks. Institutions may enhance preceptor autonomy by including community faculty and preceptors in the development of course goals and objectives, by providing flexibility on when, how, and where preceptors teach, and by seeking regular feedback on clerkship structure and curriculum. Institutions may enhance preceptor competency through informed general and targeted faculty development efforts, provision of CME activities, and through formal recognition of excellence in teaching through awards, wall plaques, teaching pins, student thank-you notes, or other mechanisms. Institutions may enhance relatedness in several ways, including: (1) regular communications including academic detailing meetings, newsletters, and timely and relevant email messages; (2) provision of community faculty and preceptors with branded promotional materials, such as coffee mugs, clothing, pens or other similar items; (3) inclusion in campus activities, such as the white coat ceremony, match day and graduation activities, or student research presentation events.
Our analysis aligns with previous studies showing that preceptors teach because of a strong internal motivation.23-25 While less effective than intrinsic motivation, external factors such as a clinical faculty appointment and academic promotion should not be taken lightly.26,27 SDT suggests, and our study supports, that financial incentives are perhaps the least successful tool to encourage community family physicians to teach,14,16,24 which may be reassuring to the many schools that are not paying community preceptors.28 Preceptors in our focus groups reported that they want their time and energy to be acknowledged and appreciated, a strategy successfully used at some institutions.26 Our analysis supports the findings of others that preceptors want to know they will receive adequate faculty development for precepting,12,25 followed by regular, succinct, and accurate communication and feedback from the institution.24,25
Our findings aligned with previous studies suggesting that SDT can function as a useful framework to organize preceptor recruitment and retention efforts by enhancing motivation to teach. Medical educators and policy makers seeking to recruit community preceptors can highlight the intrinsic motivators for teaching: the joy of seeing a student learn, the value in passing on medical knowledge, and the opportunity to shape the lives of future physicians. Focusing on this meaningful work can prevent burnout, and teaching may be one way for physicians to find personal meaning in their professional work.29-32
Highlighting another aspect of SDT, preceptors need to see how their efforts fit into the overall medical education effort. Some preceptors reported a sense of pride in being connected with a medical school, either because they themselves trained there or because they identified with the values of the school, highlighting the internalization of these extrinsic motivators. Strategies to tighten this connection, such as adjunct faculty appointments, certificates of recognition, positive student feedback, and physical reminders of this affiliation (eg, a coffee mug or patch for a lab coat), are important extrinsic motivators for some community preceptors in our study. They value thank you notes from students and updates on where students match for residency or end up practicing. Another option for building on relatedness may be to lengthen weeks spent with preceptors through longer block or longitudinal rotations.
Having medical students in a community practice environment may help physicians maintain a sense of clinical competency, another optimizer of the core psychological needs described by SDT. Medical schools can promote this benefit by providing access to resources that community physicians can use to optimize patient care and medical student education. Medical educators and policy makers should also highlight extrinsic benefits of teaching, such as CME credit.
Preceptors need to feel autonomous and competent to maintain intrinsic motivation. Attacks on autonomy and competence, such as a strictly regimented plan for clinical teaching or a lack of regular specific feedback, can diminish intrinsic motivation In our study, preceptors reported that medical schools may diminish their autonomy by placing excessive structure around clinical teaching encounters (eg, multiple checklists). While clerkship directors attempt to standardize educational experiences to ensure graduation of competent physicians and attainment of accreditation requirements,33-35 community preceptors desired flexibility to adjust learning opportunities to the patients at hand. Balancing these competing priorities is necessary to avoid diminishing intrinsic motivation for community preceptors.
Individual institutions may not be able to have a meaningful impact on some elements of the practice environment that make precepting medical students difficult. Participants in our study reported that the advent of the electronic health record and increasing documentation demands have made continuing to precept students difficult. Fortunately, Medicare now recognizes the documentation by medical students as acceptable for billing—highlighting another need for preceptor engagement and faculty development.36
Our study has several key limitations. Some sites had difficulty with convening focus groups, evidenced by three focus groups consisting of just two preceptors, also attesting to preceptor time challenges. We interviewed only family physicians who were community preceptors and agreed to participate in this study. We did not specifically recruit participants to understand the perspectives of those who had been preceptors but had since stopped teaching. Additionally, the perspectives of nonresponders are not known; we had a high nonresponse rate. We did not capture the views of physicians or other clinicians who have never taught. It is also unclear how these results would generalize to other communities of educators, such as advanced practice clinician educators or physicians in other specialties. Finally, this study did not seek to develop a hierarchy of strategies to recruit and retain preceptors, but rather to explore from community-based preceptors within the framework of SDT the challenges and frustrations of balancing a busy clinical practice with educating future physicians and other health professionals.
Future studies should determine if SDT applies to other groups of community preceptors. Surveys of community preceptors may guide medical educators and policy makers on where to focus their efforts as well as where to allocate limited financial and human resources. Local, state, and national organizations seeking to encourage community preceptors may use this framework to assess the effectiveness of their interventions. Further validation and strengthening of the community-preceptor workforce is in alignment with desires and demands to increase the primary care physician (and other clinician) workforce to meet the needs of a growing, aging, and diversifying US population.




There are no comments for this article.