Background and Objectives: We sought to evaluate whether the University of New Mexico (UNM) Combined Baccalaureate/Medical Degree (BA/MD) program increases the likelihood that students match into family medicine residencies.
Methods: We used binary logistic regression to predict interest and actual residency match in family medicine. We compared BA/MD participants to similar peers (one-to-one match subject design) and all other students for the nine cohorts of medical students who have matriculated into UNM School of Medicine since the inception of the BA/MD program (medical school matriculation years 2009-2017). We also investigated whether BA/MD students were more likely to select family medicine as their specialty choice at the time of matriculation using survey responses.
Results: At the time of matriculation, the differences in identifying family medicine as a first specialty choice between BA/MD, similar peers, and all other students were small and not statistically significant. However, upon graduation, 33% of BA/MD students matched into family medicine compared to 17% of similar peers, a statistically significant difference even after controlling for United States Medical Licensing Examination (USMLE) test scores and several demographic factors.
Conclusions: The University of New Mexico Combined Baccalaureate/Medical Degree students match into family medicine at nearly twice the rate of traditional medical degree students, suggesting that the UNM BA/MD program serves to increase the growth rate of the family medicine workforce.
According to the Association of American Medical Colleges (AAMC), the number of family medicine residency applications from US MD-granting medical schools to Accreditation Council for Graduate Medical Education (ACGME) accredited programs increased by 24% from 2012-2017. However, the number of medical students going into this field is expected to fall short of the projected demand for these services.1 Family medicine physicians uniquely focus on the patient-physician relationship in the context of the family and the community, which may play a critical role in providing care in rural areas.2,3 Students with a rural or an economically disadvantaged background are more likely to want to practice in an underserved area.4-9 Additionally, generating early interest in family medicine may also be a strategy to increase residency choice.10-12 How can medical schools intentionally increase interest in family medicine?
The Combined Baccalaureate/Medical Degree Program (BA/MD) at the University of New Mexico (UNM) is an 8-year program with three specified undergraduate degree options and provisional admission into medical school. The Health, Medicine and Human Values curriculum designed by the program promotes the health and well-being of public and underserved health populations. The program specifically recruits and accepts community-engaged, rural, ethnically and economically diverse students. This study examined the extent to which the program has been successful in producing family medicine residents.
First, the authors sought to understand the program’s impact on interest in family medicine at matriculation to UNM School of Medicine (SOM) among the nine cohorts of students who have enrolled in the medical school to date. Second, we explored the program’s impact on match rates into family medicine among the six cohorts of BA/MD students who have matched to date.
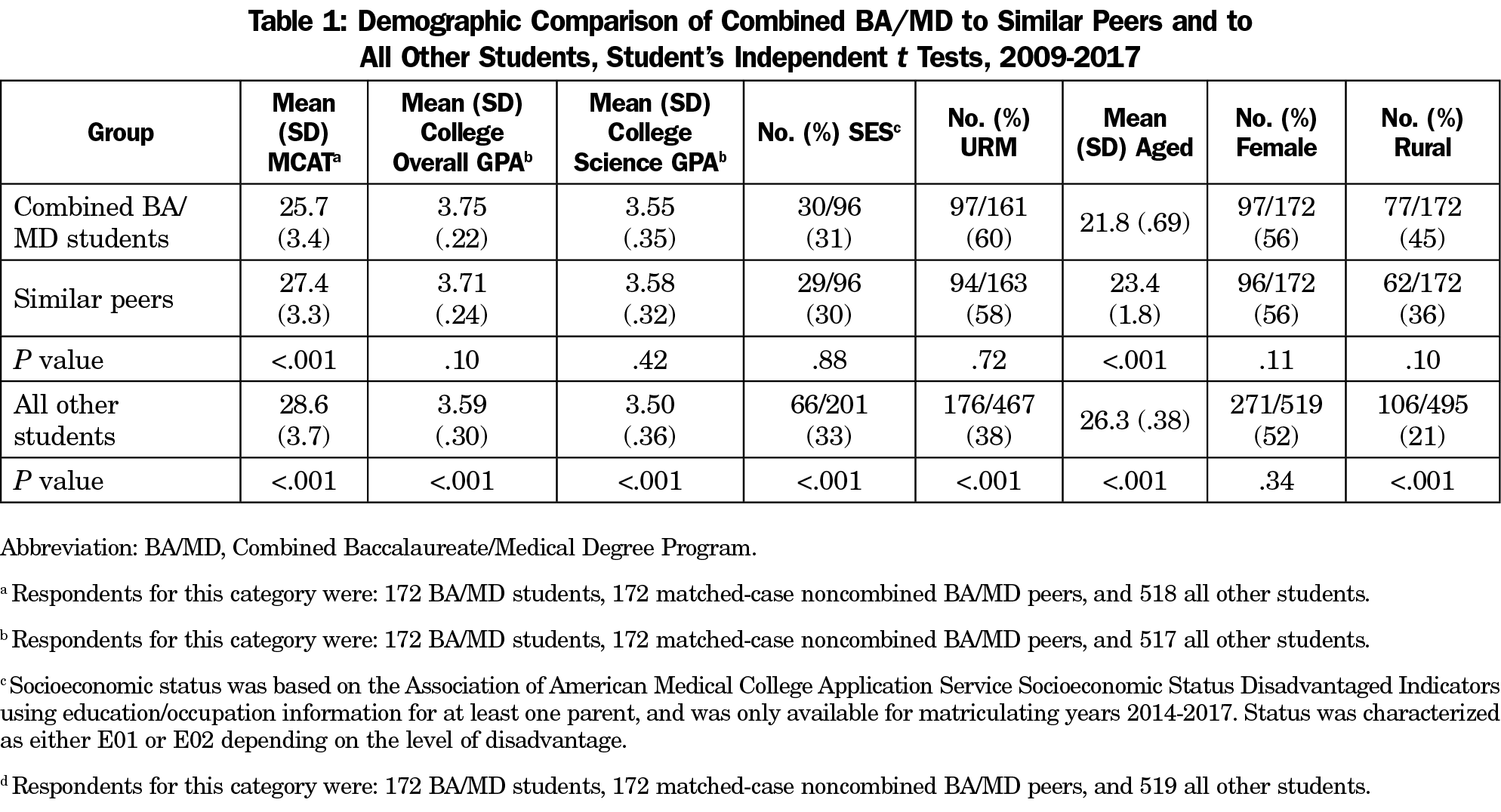
Recognizing that students’ demographic factors (eg, rural, underrepresented in medicine (URM), age, gender, socioeconomic status [SES]) may influence specialty choice, we controlled for such factors using a matched subject design. We hand-matched the 172 BA/MD students (matriculation years 2009-2017) with 172 similar non-BA/MD peers, ensuring the similar peers matriculated in the same year. We emphasized similarity especially in terms of MCAT score, college GPAs (overall and science), status in an underrepresented minority group (Hispanic, Native American/Alaska Native, African-American, or Vietnamese), and age. We also matched students as similarly as possible by gender, rural status, and when available, socioeconomic status.
We compared BA/MD students and their similar peers on interest in family medicine at matriculation to medical school and on matching in a family medicine residency during the fourth year of medical school (2009-2014 matriculants). To measure specialty interest at matriculation, we used the school’s Specialty Interest Survey, completed by all students during orientation. We initially compared both of these outcomes between BA/MD students and their similar peers using Student independent sample t tests. We then analyzed the outcomes using binary logistic regression, controlling for USMLE test outcomes and demographic factors.
The Institutional Review Board at the University of New Mexico Health Sciences Center approved this research.
The level of similarity achieved in our matching process is indicated in Table 1. While statistically equivalent in most respects, the BA/MD students had a statistically significant lower MCAT score than non-BA/MD similar peers (25.7/27.4, P<.001) and were statistically significantly younger (21.8/23.4, P<.001). Table 1 also gives demographic information for all other students in the nine cohorts. BA/MD students and their similar matched peers were dissimilar to all other students in most of the demographic characteristics. Thus, we provide both the bivariate analyses of our two outcomes and the multivariate analyses to further control demographic factors.
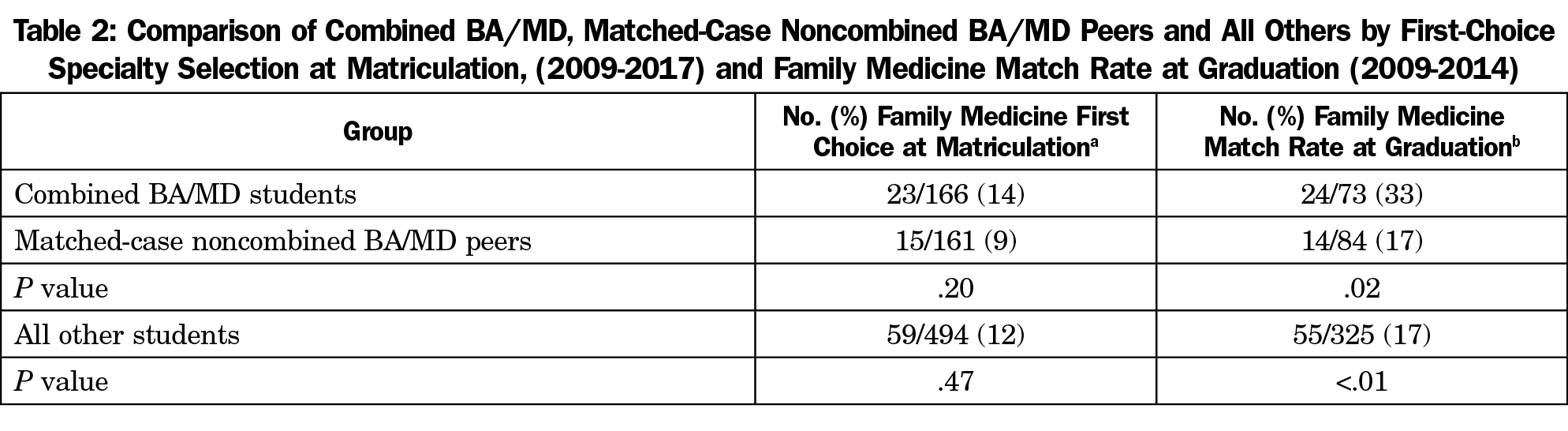
Table 2 shows the initial bivariate analyses. The first column shows that BA/MD students at matriculation (2009-2017 cohorts) chose family medicine as their first specialty choice at a rate of 14% (23/166) in comparison 9% (15/161) of their matched peers and 12% (59/494) of all others, small differences that are not statistically significant. Nevertheless, as seen in the second column, BA/MD students at graduation (2009-2014 cohorts) matched into family medicine at nearly double the rate of their similar peers (33% or 24/73 compared to 17% or 14/84; P<.05) and all others (17% or 55/325; P<.01). Among students who had selected family medicine as their first choice at matriculation, BA/MD students were far more likely to uphold that choice at graduation, and matched at a rate of 67% in comparison to their similar peers (25%) and all others (38%).
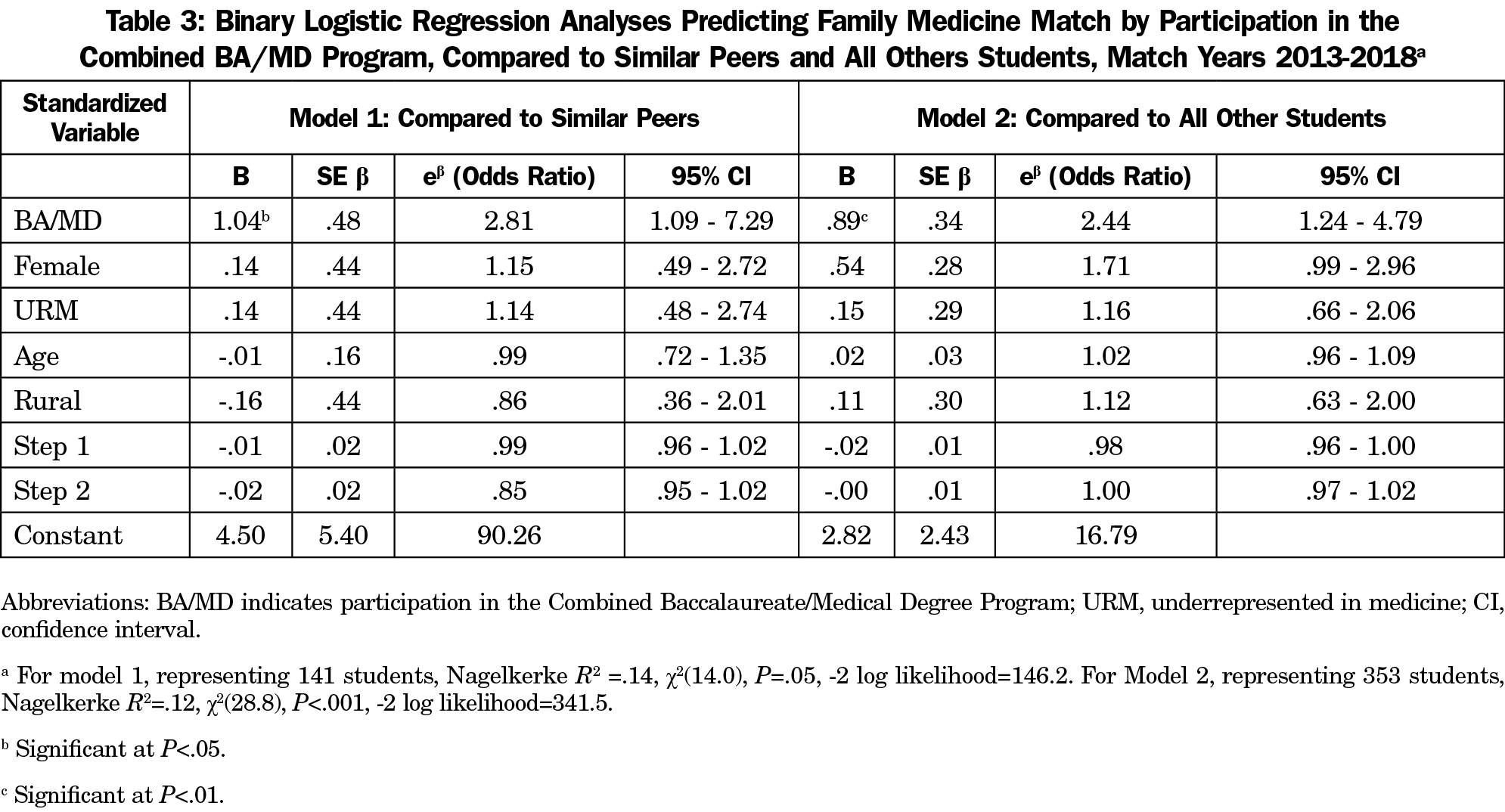
Table 3 demonstrates our analysis of residency match using binary logistic regression to control statistically for demographic factors and academic performance. We predict family medicine match for participation in BA/MD in comparison with similar matched peers (model 1) and all others (model 2). The results indicate that in both models, participating in the UNM BA/MD is a statistically significant predictor for matching in family medicine.
This study’s findings show that UNM BA/MD students match into family medicine at twice the rate of traditional medical degree students, suggesting that the UNM BA/MD program is instrumental in increasing the family medicine workforce. It appears that the UNM BA/MD program enhances interest in and selection of family medicine, as the BA/MD students who selected family medicine at matriculation were more likely to continue with that choice, and those who had not originally selected it at matriculation were more likely to choose it at graduation. Although family medicine was by far the most common primary care specialty selected, pediatrics was next (12%), followed by internal medicine (10%).
Both in terms of holistic admission processes and curriculum, the program was intentionally designed to provide educational opportunities to diverse students committed to serving rural and underserved communities in New Mexico. In terms of admissions, the program accepts applicants who demonstrate their desire and commitment to medically underserved communities in the state through community and volunteer service. The program admits two-thirds of the entering class from rural areas. A high percentage (62%) of BA/MD students who have been accepted to the program identify as underrepresented in medicine (URM; 41% Hispanic, 13% American Indian/Alaska Native, 4% African American, 4% Vietnamese). Thus, BA/MD students are perhaps more likely to choose family medicine a priori.
The BA/MD program itself may reinforce a humanitarian outlook and positive perception of family medicine. As undergraduates, all BA/MD students complete a 1-month service learning practicum. The practicum occurs during the summer of their second undergraduate year and is completed in a rural and underserved health care setting.13 Additionally, five required courses and two required workshops provide a strong foundation in public health with emphasis on health care issues relevant to the specific circumstances of New Mexico, as well as the national and global context of medicine and health. It seems likely that both admissions and programming factors help explain the fact that BA/MD students select family medicine at nearly twice the rate of similar peers and other students. The fact that BA/MD students had lower MCAT scores than non-BA/MD similar peers could indicate that these students have not been accepted through the regular admissions process, further supporting the argument that some students who would enter the family medicine program are not gaining admission to medical school. Since the data set is relatively small and consists of only six graduating cohorts at a public medical school in the western United States, the generalizability to other institutions may be limited. Nevertheless, we will continue to monitor the program progress over time.
Acknowledgments
The authors thank the UNM College of Arts and Sciences BA/MD Program faculty and staff for designing and implementing an exceptional undergraduate experience that responds to the health care needs of New Mexico.
Financial Support: This effort was partially funded by the University of New Mexico School of Medicine.
Prior Presentations: BA/MD match rates were presented at the UNM SOM Committee on Admissions annual retreat on April 19, 2018 in Albuquerque, New Mexico.
References
- Association of American Medical Colleges. Report on Residents. Table C3: Residency Applicants to ACGME-Accredited Programs by Specialty and Medical School Type, 2017-2018. https://www.aamc.org/download/321562/data/2013factstablec3.pdf. Accessed July 25, 2019.
- Kelly C, Roett MA, McCrory K, et al; Family Medicine for America’s Health Collaborative. A shared aim for student choice of family Medicine: an update from ADFM and family medicine for America’s health. Ann Fam Med. 2018;16(1):90-91. https://doi.org/10.1370/afm.2191
- Rabinowitz HK, Diamond JJ, Markham FW, Wortman JR. Medical school programs to increase the rural physician supply: a systematic review and projected impact of widespread replication. Acad Med. 2008;83(3):235-243. https://doi.org/10.1097/ACM.0b013e318163789b
- Talib Z, Jewers MM, Strasser JH, et al. Primary care residents in teaching health centers: their intentions to practice in underserved settings after residency training. Acad Med. 2018;93(1):98-103. https://doi.org/10.1097/ACM.0000000000001889
- Goodfellow A, Ulloa JG, Dowling PT, et al. Predictors of primary care physician practice location in underserved urban or rural areas in the United States: A systematic literature review. Acad Med. 2016;91(9):1313-1321. https://doi.org/10.1097/ACM.0000000000001203
- Kost A, Cawse-Lucas J, Evans DV, Overstreet F, Andrilla CHA, Dobie S. Medical student participation in family medicine department extracurricular experiences and choosing to become a family physician. Fam Med. 2015;47(10):763-769.
- Talamantes E, Hernandez AM, Gonzalez R, et al. Interest in family medicine among US medical students and its association with a community college academic pathway. Fam Med. 2017;49(10):759-764.
- Pretorius RW, Milling DA, McGuigan D. Influence of a rural background on a medical student’s decision to specialize in family medicine. Rural Remote Health. 2008;8(3):928.
- Pacheco M, Weiss D, Vaillant K, et al. The impact on rural New Mexico of a family medicine residency. Acad Med. 2005;80(8):739-744. https://doi.org/10.1097/00001888-200508000-00007
- Kost A, Cantone RE, Schneider B, Sairenji T, Palmer R. Validation and Comparison of a Brief Instrument vs a Single-Item Screen to Predict Entry to Family Medicine at Matriculation to Medical School. Fam Med. 2018;50(9):672-678. https://doi.org/10.22454/FamMed.2018.258795
- Talamantes E, Jerant A, Henderson MC, et al. Community college pathways to medical school and family medicine residency training. Ann Fam Med. 2018;16(4):302-307. https://doi.org/10.1370/afm.2270
- Senf JH, Campos-Outcalt D, Kutob R. Factors related to the choice of family medicine: a reassessment and literature review. J Am Board Fam Pract. 2003;16(6):502-512. https://doi.org/10.3122/jabfm.16.6.502
- Clithero A, Sapien R, Kitzes J, et al. Unique premedical education experience in public health and equity: Combined BA/MD summer practicum. Creative Ed. 2013;4, 165-170. http://doi.org/10.4236/ce.2013.47A2021
- Rosenthal TC, McGuigan MH, Anderson G. Rural residency tracks in family practice: graduate outcomes. Fam Med. 2000;32(3):174-177.
- Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA. 1999;281(3):255-260. https://doi.org/10.1001/jama.281.3.255



There are no comments for this article.