Background and Objectives: Despite the importance of breastfeeding, most US women do not meet recommendations for length of any or exclusive breastfeeding. Support in primary care settings is recommended (US Preventive Services Task Force, 2016), but optimal implementation strategies are not established. We evaluated the effect on breastfeeding rates of on-site breastfeeding support within an academic family medicine center with a diverse patient population.
Methods: We conducted a retrospective chart review 10 months before and 10 months following the implementation of integrated breastfeeding support provided by an International Board Certified Lactation Consultant (IBCLC) or MD-IBCLC. Two hundred eighty-one infants were identified, 140 before implementation and 141 after. A research assistant extracted data from the electronic medical record. We performed bivariate and multiple logistic regression analyses using STATA.
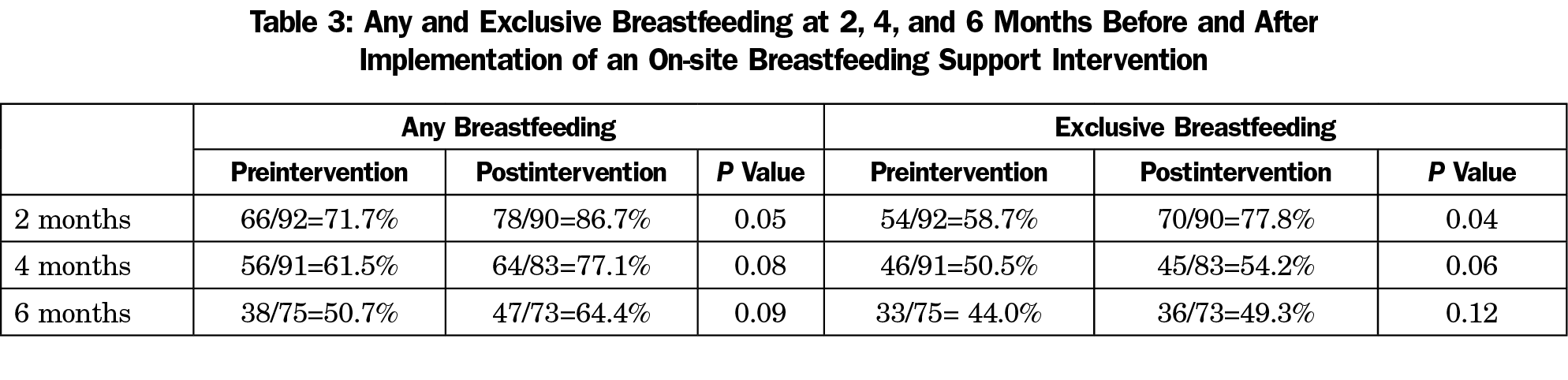
Results: There were no significant demographic differences before and after the intervention. The proportion of infants with any breastfeeding at 2, 4, and 6 months was greater in the postimplementation group (71.7% vs 86.7% at 2 months, P=.05; 61.5% vs 77.1% at 4 months, P=.08; and 50.7% vs 64.4%, P=.09 at 6 months). The proportion of infants exclusively breastfed was also greater in the postimplementation group (58.7% vs 77.8% at 2 months, P=.04; 50.5% vs. 54.2% at 4 months, P=.06; and 44.0% vs 49.3% at 6 months, P=.12).
Conclusions: Providing on-site IBCLC breastfeeding support services within an academic family medicine clinic is associated with significant increases in breastfeeding, supporting the provision of lactation services on-site where mothers and children receive primary care.
The Centers for Disease Control and Prevention incorporates five breastfeeding parameters into their Healthy People 2020 objectives, underscoring the importance of breastfeeding to the health of the American population.1 Although most women initiate breastfeeding, a minority exclusively breastfeed for 6 months as recommended by US medical groups including the American Academy of Family Physicians.2-4 The United States Preventive Services Task Force finds that primary care interventions to support breastfeeding change maternal breastfeeding behaviors and recommends providing such interventions during pregnancy and after childbirth.5 A recent Cochrane review finds the most effective breastfeeding support is “offered as standard by trained personnel during antenatal or postnatal care.”6
We developed a comprehensive, integrated model of breastfeeding support within our family medicine center to improve quality of care for mother-infant dyads. Our objectives were to determine baseline breastfeeding rates and compare them to rates after implementing our new model of care. Our hypothesis was that offering on-site lactation consultations with international board-certified lactation consultants (IBCLCs) would increase the duration of any and exclusive breastfeeding.
Study Setting and Intervention
This study took place in a freestanding family medicine clinic affiliated with an academic medical center. Approximately 170 infants under 2 weeks of age receive care at this site annually. Before the intervention, breastfeeding support was provided primarily by a perinatal nurse coordinator who referred externally for IBCLC services.
The intervention consisted of: (1) IBCLC certification for the perinatal nurse coordinator, who continued to provide breastfeeding support, and (2) on-site lactation consultations with a family physician-IBCLC. Consultations were available if parent or clinician identified breastfeeding or infant growth concerns. Following initial consultation, further support was available through additional appointments, electronic messages, and phone support. Both the perinatal nurse coordinator and physician-IBCLC participated in structured resident and staff didactics and informal consultation with residents and faculty, with the goal of improving breastfeeding support throughout the clinic.
Study Design and Sample
An uncontrolled retrospective pre- and postintervention chart review design was used to evaluate the new model of breastfeeding support. The study period consisted of a 10-month period prior to the intervention, and a 10-month period after implementation. We excluded infants who were not seen in our clinic by 2 weeks of life, a period critical for establishing breastfeeding.
Data Collection
A single research assistant extracted data from the electronic medical record into a Qualtrics chart extraction tool. We specified the exposure variable as intervention status, defined by whether birth date was pre- or postimplementation of the intervention. Clinic billing records identified 281 infants with birth dates in the study period, 140 in the preintervention group and 141 in the postintervention group.
Outcome variables were any breastfeeding and exclusive breastfeeding at 2, 4, and 6 months, which we assessed by reviewing infant feeding as recorded in visit notes for corresponding well-child visits. Infant feeding method was documented as breast milk only, formula only, breast milk and formula, or unable to determine.
We identified demographics and medical history from delivery records. The study team selected potentially relevant covariates based on existing literature.
We imported data into STATA version 14 (Stata Corp, College Station, TX) for analysis. We assessed for statistically significant differences in demographic characteristics between pre- and postintervention groups using χ2 tests. We calculated frequency of any breastfeeding and exclusive breastfeeding at 2, 4, and 6 months, with statistically significant differences between pre- and postintervention determined using a P value of ≤.05.
The University of North Carolina’s (UNC) Institutional Review Board determined this study to be exempt.
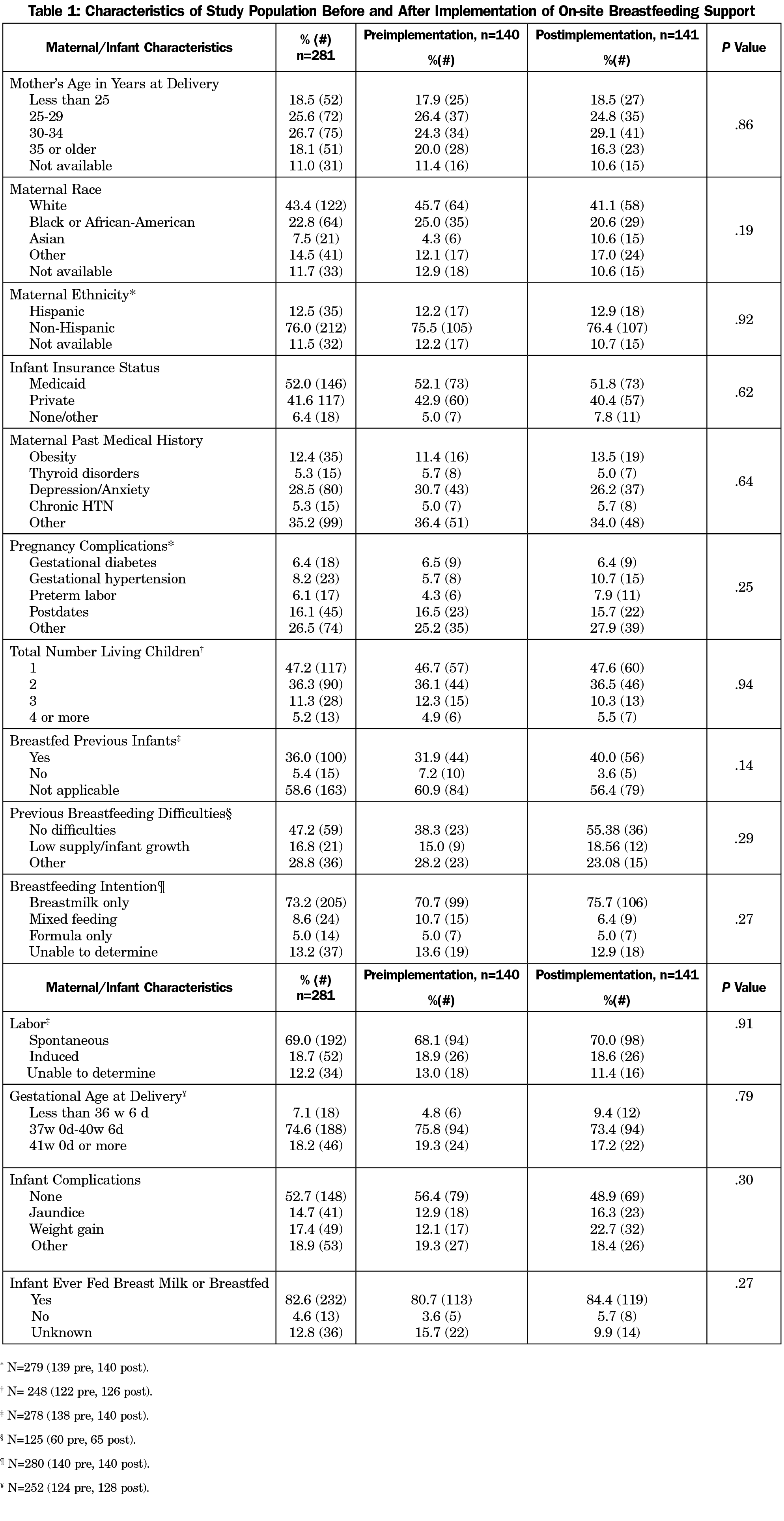
The study sample included 281 mother-infant dyads. More than half of mothers were between ages 25 and 34 years; 43.4% identified as white/non-Hispanic, 22.8% as black/non-Hispanic or African-American, and 12.5% as Hispanic. Fifty-two percent of infants were covered by Medicaid. Demographic, medical history, and other relevant variables were generally similar between the pre- and postintervention groups (Table 1).
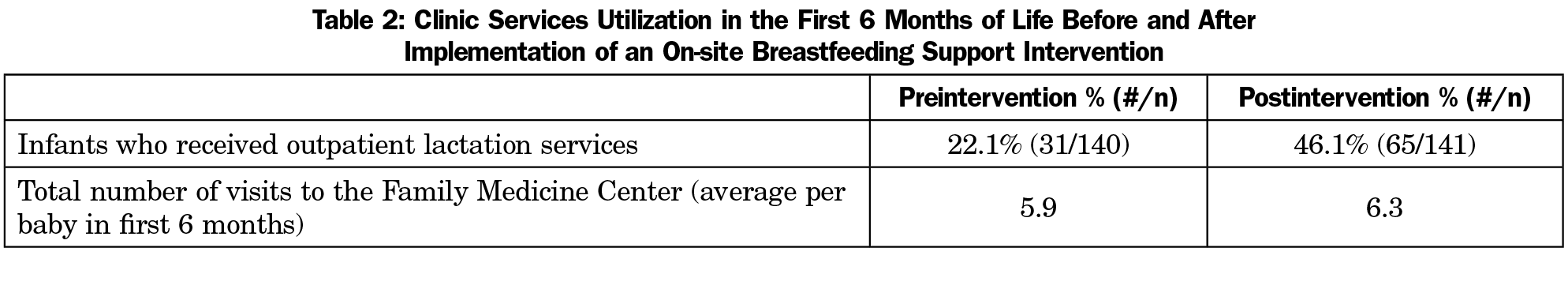
Twenty-two percent of patients in the preintervention group accessed lactation services; this increased to 46% among the postintervention group (Table 2). In the preintervention group, 58.7% were exclusively breastfeeding at 2 months, compared to 77.8% in the postintervention group (P=.045; Table 3). The values at 4 months and 6 months were higher for the postintervention group but not significantly different (50.5% vs 52.2%, P=.062 and 44.0% vs 49.3%, P=.118). For any breastfeeding, the difference between pre- and postintervention groups at 2 months was significantly different (71.7% vs 86.7% at 2 months, P=.05; 61.5% vs 77.1% at 4 months, P=.08; and 50.7% vs 64.4%, P=.09 at 6 months; Table 3).
This study shows that in a diverse population served by an academic family medicine practice, integrating on-site comprehensive breastfeeding support services is associated with greater duration of any and exclusive breastfeeding; statistically significant increases were found for both any and exclusive breastfeeding at 2 months.
Our results demonstrate that offering on-site lactation services is associated with increased use of such services. Providing breastfeeding support services in a known location in the context of established care relationships likely contributes to this increased utilization, as well as improved breastfeeding outcomes. Integrated support facilitates a consistent message to mothers that their health care team values and supports their breastfeeding efforts. Colocation and integration may be particularly beneficial in reaching mothers from groups less likely to breastfeed, including African-American mothers, younger mothers, and mothers with infants covered by Medicaid.7
The sample size limits the study, particularly at the 6-month point. Despite the inability to detect statistical significance, the changes in any breastfeeding rates at 4 months (+15.6%) and 6 months (+13.7%) are clinically significant. This study was based at a single, academic family medicine practice, which may limit generalizability. As a retrospective chart review, this study demonstrates association, not causation; however, national breastfeeding indicators have changed much less year to year than the changes we demonstrated.8
Further studies of interest include subgroup analyses in groups less likely to breastfeed, to better understand the potential for this intervention to reduce breastfeeding disparities. Another area of interest is complementary qualitative research to elucidate whether mothers value on-site breastfeeding support services.
Acknowledgments
Financial Support: Dr Sanchez was supported through the Preventive Medicine Residency Program at UNC (HRSA D33HP25771).
Presentations: Data from this report were presented at a poster presentation at Academy of Breastfeeding Medicine, November, 2017, Atlanta GA.
References
- US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health/objectives. Accessed May 20, 2017.
- American Academy of Pediatrics. Breastfeeding and the use of human milk (Policy Statement). Pediatrics. 2012;(129):3. https://doi.org/10.1542/peds.2011-3552
- American Academy of Family Physicians. Breastfeeding (Policy Statement). http://www.aafp.org/about/policies/all/breastfeeding.html. Accessed May 20, 2017.
- American Congress of Obstetricians and Gynecologists. Committee Opinion: Optimizing Support or Breastfeeding as Part of Obstetric Practice. Number 658, February 2016. http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Optimizing-Support-for-Breastfeeding-as-Part-of-Obstetric-Practice. Accessed May 20, 2017.
- United States Preventive Services Task Force; Bibbins-Domingo K, Grossman DC, et al. Primary care interventions to support breastfeeding. JAMA. October 2016; 316(16):1688-1705. https://doi.org/10.1001/jama.2016.14697
- McFadden A, Gavine A, Renfrew MJ, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev. 2017;2(2):CD001141. https://doi.org/10.1002/14651858.CD001141.pub5
- Anstey EH, Chen J, Elam-Evans LD, Perrine CG. Racial and geographic differences in breastfeeding - United States, 2011-2015. MMWR Morb Mortal Wkly Rep. 2017;66(27):723-727. https://doi.org/10.15585/mmwr.mm6627a3
- Centers for Disease Control and Prevention: National Center for Chronic Disease Prevention and Health Promotion: Division of Nutrition, Physical Activity, and Obesity. Breastfeeding Report Card: Progressing Toward National Breastfeeding Goals, United States, 2016. 2016. https://www.cdc.gov/breastfeeding/pdf/2016breastfeedingreportcard.pdf. Accessed May 22, 2019.



There are no comments for this article.