Background and Objectives: The role of training in the declining rate of family physicians’ provision of women’s reproductive health care is unclear. No requirements for abortion training exist, and curricula vary widely. This study assessed the impact of program-level abortion training availability on graduates’ feelings of training adequacy and their postgraduate practice in reproductive health.
Methods: We conducted secondary analysis of graduate survey data from 18 family medicine residency programs in the Northwest categorized by whether or not their program routinely offered abortion training (opt out or elective rotation). We used bivariate analyses and logistic regression to compare groups on preparation for training and current clinical practice of women’s health procedures.
Results: Six of 18 programs included in the study had routinely available abortion training for graduates (N=408). In bivariate analysis, these programs with routine abortion training had significantly more graduates who report feeling prepared to perform abortions (19% vs 10%; P=.01), but no difference in likelihood to provide abortion care postresidency compared to programs without routine abortion training. In adjusted analyses, graduates of programs with routine abortion training were significantly less likely to feel prepared for performing colposcopies (OR=0.45, 95% CI, 0.26-0.78; P<.01) and to actually perform them in practice (OR=0.32, 95% CI, 0.18-0.57; P<.001); all other differences are attenuated.
Conclusions: Program-level abortion training alone is not enough to overcome the systems- and individual-level barriers to increasing the numbers of trained family medicine residency graduates who provide abortion care and other reproductive care in practice. More must be done to create opportunities for family physicians interested in providing full-spectrum care in their postgraduate practices to be able to do so.
Historically, the role of family physicians has included the practice of obstetrics and women’s health care. However, in recent years, the number of family physicians providing maternity care has been on the decline and was down to less than 10% in 2010.1 Reports of provision of other women’s health services are also low; a recent study found only 19.7% of responding family physicians regularly performed intrauterine contraceptive device (IUD) insertions; 11.3% routinely placed/removed contraceptive implants2; and another found that most family physicians offer only expectant management of miscarriage (“watch and wait”) instead of medication and/or procedural management.3 There is uncertainty in how much of this gap in provision is related to training.
The Accreditation Council for Graduate Medical Education (ACGME) does not have specific requirements regarding abortion training. The guidelines state:
Residents must have at least 100 hours (or 1 month) or 125 patient encounters dedicated to the care of women with gynecologic issues, including well-woman care, family planning, contraception, and options counseling for unintended pregnancy.4
Because no specific requirements exist around abortion care, residency programs offer an array of opportunities around abortion training.5,6 Programs may elect to have no training (no procedural training, no formal didactics) on abortion care, have some training (no formal didactics, but procedural training during elective time or formal didactics without available procedural training), have routinely available training (formal didactics and procedural training during elective time), or routinely integrated opt-out training (formal didactic and clinical training, with the option to opt out of procedural training).
Existing literature in family medicine and obstetrics shows that individuals who receive abortion training feel more prepared to perform abortions independently postgraduation.7,8 In addition, individuals with higher procedural numbers are more likely to continue abortion practice postresidency.7,9 These studies have focused on individual training, and thus far no studies have investigated the impact of program-level support of abortion training. Given the demands on family medicine training with a need to cover a wide breadth of clinical content in a just a few years of training, program directors (PDs) benefit from data regarding the impact of their curricula on preparation for practice and actual practice patterns of their program graduates. The aim of this study was to assess the impact of program-level support of abortion care on overall abortion training and postresidency practice.
All family medicine residency programs in Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI) are part of the collaborative Family Medicine Residency Network (FMRN). Historically, every 2 years the FMRN surveyed those who graduated from affiliated programs in the prior 2 years. The survey included questions about graduate demographics, practice characteristics, adequacy of training for various procedures, and current clinical practice of these procedures. At the time of these surveys, there were 18 programs with graduates (ie, excluding new programs) in the FMRN.
This study was a retrospective cohort study, analyzing responses to the 2012 and 2014 surveys, that included graduates from 2010 to 2013. The primary outcomes for this study were graduates’ reported feelings of adequacy of residency training and current clinical practice around pregnancy termination; secondary outcomes included other reproductive health procedures: deliveries, C-section assist, colposcopy, dilation and curettage (D&C), and IUD placement. Missing data for all questions of interest was confirmed to be low, with less than 3% of responses missing on any given question.
We categorized graduates by whether or not their program routinely offered elective abortion training. To determine which programs routinely offered abortion training, PDs were asked in December 2014 if any residents since 2005 had received abortion training as part of an elective or regular rotation and whether abortion training was a routine part of didactics. For clarification, we also asked the number of residents receiving abortion training and whether there had been any changes in availability of abortion training since 2005. The authors reviewed blinded responses and considered those who indicated they offered both didactics and hands-on training (elective or routine) to have “abortion training routinely available”; all others were considered to have no routine abortion training.
SPSS 19.0.0 was used for all analyses. We characterized our sample using descriptive statistics. We then compared bivariate associations among graduates in programs with and without elective abortion training for reported adequacy of training and current practice of all primary and secondary outcomes. Graduates who said they felt well or very well prepared for practice were compared to those who said they felt less than well prepared. Those who said they are currently practicing a given procedure were compared against those who reported they were not. Given the wide range of practice patterns and feelings about adequacy of training for all reproductive health procedures among graduates from all programs, no program was an outlier for all variables; as such, all programs were included in the analyses except where indicated.
To determine associations between abortion training during residency and adequacy of training as well as actual postresidency practice, we constructed logistic regression models that controlled for individual and program characteristics. After a stepwise analysis, our final adjustments to the model included graduates’ gender and whether the program had an emphasis on training for rural practice or not. We defined an emphasis on rural practice as having a rural training track or having a program mission that includes preparation for rural practice. For the logistic regression model including graduates’ postresidency practice, we also adjusted for size of the graduates’ practice community using three size categories for population: less than 10,000; 10,000 to 99,000; and suburb, or more than 100,000. For all analyses, we set statistical significance at P<.05.
This study was approved by the University of Washington Institutional Review Board under expedited review.
Program Demographics
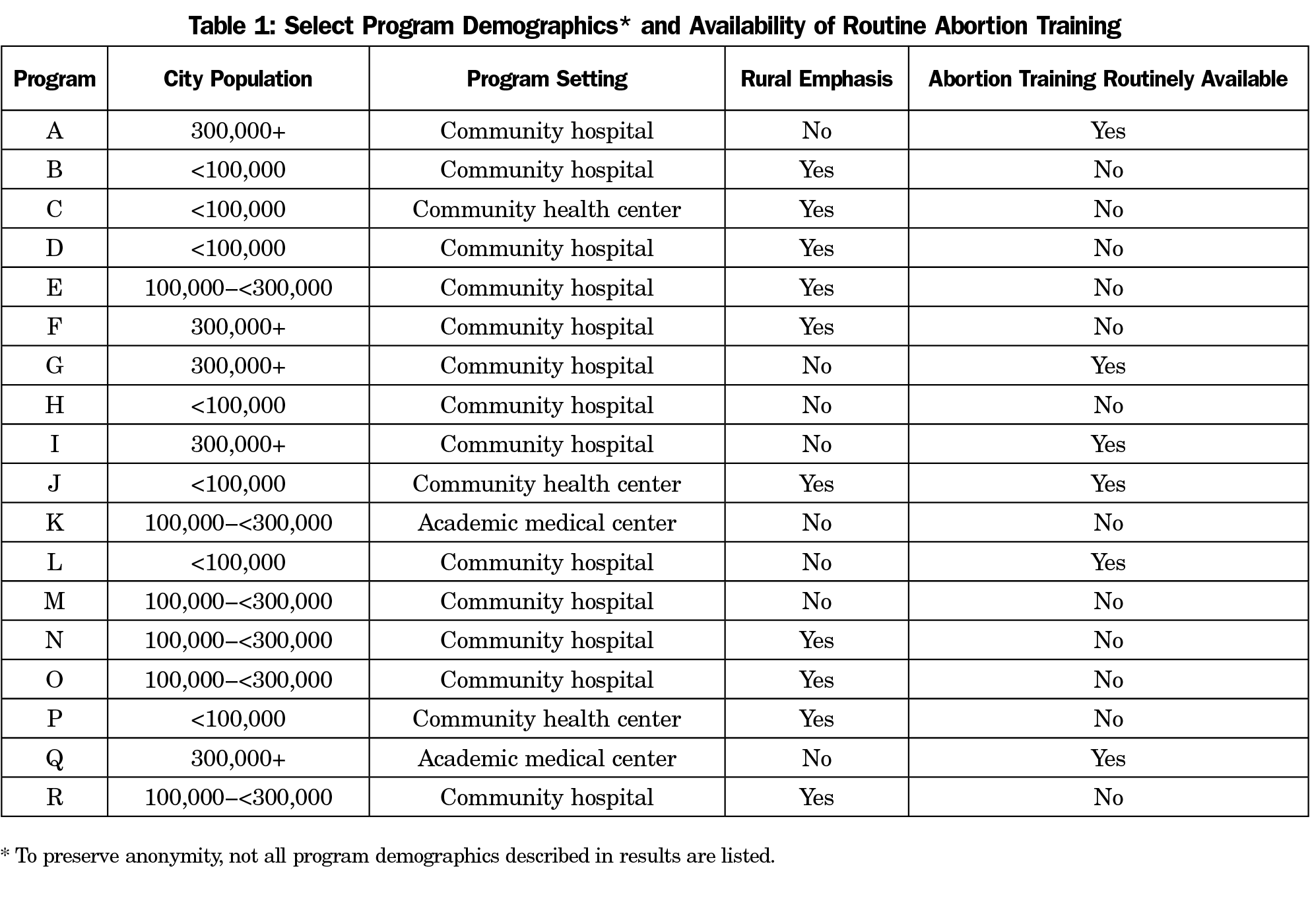
The 18 programs whose graduates were included in the 2012 and 2014 surveys are located in cities with population between 40,000 and 650,000. Programs were located at community hospitals (n=13), community health centers (n=3), and academic medical centers (n=2). The majority (n=11) were the only residency program in their institution, and only two of the seven institutions with other residency programs had an obstetrics and gynecology program. More than half (n=10) were established before 1980. Residency class sizes range from six per year to 16 per year. Ten of the programs had a rural emphasis in their mission; three of these had a rural training track (Table 1).
We determined that six programs had abortion training routinely available for their 2010-2013 graduates, while the other 12 programs were considered to have no routine abortion training.
Respondent Demographics
The 2012 survey had a total of 196 respondents from the classes of 2010 and 2011 (75% response rate) and the 2014 survey had 212 respondents from the classes of 2012 and 2013 (77% response rate). All responding graduates on the 2012 and 2014 FMRN graduate follow-up surveys were included in the sample (n=408).
Respondents were evenly spread between the 4 graduation years; the majority were female (58%). The survey did not include questions on age, race/ethnic background, or other individual demographic characteristics. Graduates had a similar spread of practice settings and organizations (eg, solo practice, family medicine partnership or group, multispecialty group, residency, or university teaching environment), and about 45% spent the majority of their time practicing in an underserved or federally designated setting. There were no differences among graduates from programs with or without routine abortion training for these available variables, though more graduates from programs without routine abortion training were practicing in small communities of fewer than 10,000 people (31% vs 13%, P<.001).
Routinely Available Abortion Training and Postgraduate Women’s Health Practices
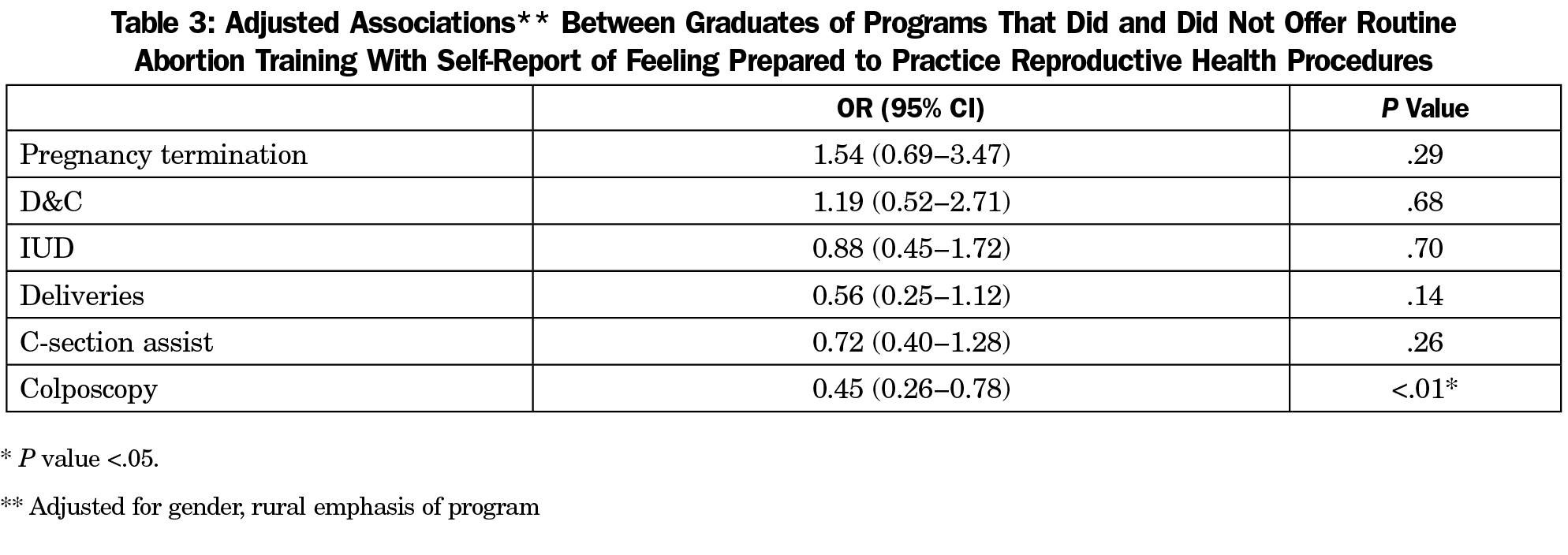
In bivariate analysis, programs with routinely available abortion training have significantly more graduates who report feeling well or very well prepared to perform abortions than programs without routine abortion training (Table 2). However, programs without routine abortion training have significantly more graduates who report feeling well or very well prepared to do colposcopies and to assist on C-sections than programs with routine abortion training. The relationship between programs with routinely available abortion training and graduate feelings of being prepared to perform abortions and assist on C-sections are attenuated in the multivariate regression model. However, in the adjusted model, graduates of programs with routine abortion training have about half the odds of feeling well or very well trained for practicing colposcopies compared to graduates of programs that did not offer routine abortion training (Table 3).
Among programs with routine abortion training, there were two outliers; one program had 82% of respondents reporting feeling well or very well prepared for pregnancy termination while another had only 3% feeling well or very well prepared. Bivariate analysis with the high outlier removed resulted in a loss of significance in this analysis; bivariate analysis with the low outlier removed did not.
Graduates of programs without routine abortion training are significantly more likely to perform D&Cs and colposcopies in postgraduate practice than those who trained in programs with routine abortion training (Table 4). Similar to the analysis of preparation for practice described above, after adjustment in the multivariate logistic model (data not shown), only the significant association for performing colposcopies in practice holds. Graduates of programs with routine abortion training had 68% lower odds of performing colposcopies in their postgraduate practice compared to graduates of programs without routine abortion training (OR=0.32; 95% CI, 0.18-0.57; P<.001).
Our study suggests that the availability of residency program-level abortion training is associated with overall higher self-reported preparedness to practice abortion care, but that this is attenuated by whether a program has a rural emphasis. Availability of abortion training at a program level was not associated with higher postresidency provision of abortion care 1 to 2 years postresidency.
Even among the six programs we defined as having routinely available abortion training, there was a wide range in the content of their abortion training programs. Some programs had routine formal didactics and clinical training with an opt-out option for procedural training. Other programs had routine formal didactics with programmatic support for procedural training during elective time, the degree of which can also vary. This is reflected in the results described above regarding the high and low outlier programs among those with routine abortion training. Bivariate analysis with the high program outlier removed resulted in a loss of statistical significance regarding preparedness to practice abortion care, while removal of the low outlier program did not. This suggests that our analysis may be driven by one program’s particularly robust abortion training program. However, it also suggests that program-level adoption of a more supportive abortion training program could further increase residents’ self-reported preparedness to practice abortion care.
Programs with available abortion training had lower graduate-reported training adequacy in C-section assist and colposcopy. We hypothesize that because family physicians in rural areas are likely to be the main providers of maternity care, programs with a rural focus consequently emphasize maternity care skills (eg, performing or assisting C-sections).10-12 This hypothesis is supported by our multivariate analysis, which attenuated differences in C-section practice when we controlled for programs with rural emphasis. The significant differences in preparation for and practice of colposcopy are harder to explain, though may be related to recent clinical guideline changes that impact the need for colposcopy. The volume of colposcopy in a particular program may be related to factors outside of our study, such as patient demographics and access to care. We also hypothesize that because there is limited time in residency, programs with available abortion training trade off clinical teaching time for abortion with other reproductive health procedures, such as C-section training and colposcopy. Similar to abortion care, the ACGME makes no specific requirements regarding C-section training and colposcopy, stating that “residents must document 200 hours (or 2 months) dedicated to participating in deliveries and providing prenatal and postpartum care.”4 Thus, these three reproductive health procedures (abortion, C-section assisting, colposcopy) may occupy the same curricular or elective time. Individual residents and/or programs may emphasize or prioritize particular procedures for a variety of reasons including access to training opportunities, patient demand, health system rules, faculty training, and resident interest. Recognizing that these procedures may compete for the same curricular time can help direct program evaluations to ensure an adequate training balance among these procedures.
Program-level abortion training was not associated with greater postresidency practice of abortion care or other reproductive health procedures. Our study joins a larger body of literature13-16 that indicates that family medicine residents, despite adequate training, are not practicing to their full capacity. In addition, abortion care faces particular barriers to practice that would not be captured in our adjusted analysis. For example, other studies have indicated that individual intent to practice abortion, individual clinical priorities, and individual practice barriers such as insurance or institutional support are important obstacles to abortion provision.8 Additionally, abortion care continues to be highly compartmentalized, with 59% of abortions occurring in specialized abortion clinics.17 Finally, in the WWAMI region, Seattle has a relatively high number of trained abortion providers (family physicians and obstetrician-gynecologists). The Bay Area is an area with similarly high numbers of trained abortion providers, and one study of highly motivated residents completing a year-long abortion curriculum reported that 15% of graduates cited market saturation as a primary reason they were not planning to provide abortion care.18 This may have also been a barrier for the graduates in our study, particularly in the Seattle area.
In all settings, to continue providing abortion care, family medicine physicians trained in abortion care may work for an abortion clinic and miss time from their primary care or other clinical care, thus losing opportunity to practice other obstetric/gynecologic procedures. This may not be feasible shortly after residency; our study looked at graduates 1 to 2 years postresidency and more time may be required for new providers to get traction to offer abortion services, for example after first offering medication abortion or office miscarriage management. Continuing Reproductive Education for Advanced Training Efficacy (CREATE) is a curriculum designed to bridge the gap between clinical training and postresidency abortion practice and has been implemented in the Bay Area, Seattle, and New York City.16,18 Programs like CREATE may be particularly important in rural areas to help support postresidency abortion care.
This study has several limitations. We defined “routinely available abortion training” based on responses from PDs, who may under- or overestimate their program’s extent of abortion training. PDs may not be aware of the full range of training and elective opportunities being accessed by residents. This is exemplified by the fact that 10% of graduates of programs that we classified as not offering routine abortion training reported feeling well or very well prepared in pregnancy termination by their residency program.
The survey asked graduates about both D&Cs and pregnancy termination without defining these terms, which means they could be interpreted differently by different respondents. We found that more FMRN graduates reported practicing D&Cs than terminations, and we suspect that respondents may interpret D&C as a procedure for miscarriage management or elective abortion while interpreting pregnancy termination as elective abortion, though it could be either by medication or uterine aspiration.
The findings of this study may not be generalizable to other regions of the country; the programs in the FMRN have a higher percentage of graduates who perform deliveries and practice maternity care and women’s health procedures than the national averages would suggest.1 More research addressing the different degrees of abortion training as well as the differences in medication and surgical abortion procedures would be beneficial, as would research on other women’s health procedures growing in popularity, such as point-of-care ultrasound. Research in other settings across the country would also be warranted. It would also be useful to consider the implications of not practicing gynecological care earlier in a woman’s reproductive life on later life gynecological care, such as menopause symptom management and vulvar health.
In summary, although there is a clear association between program-level abortion training and preparedness to practice abortion, program-level abortion training alone is not enough to overcome the systems and individual-level barriers facing graduates to provide abortion care postresidency. This finding adds to the growing literature demonstrating that broad training and practice intention does not always translate to a broad scope of practice.13,15,19 Training beyond clinical skills is necessary to allow our graduates to practice the fullest possible spectrum of care.
Acknowledgments
The authors acknowledge the contributions of Lamya Khoury, MD, MPH for her role in critically reviewing the analysis and her work on an early version of this manuscript.
Presentations: Initial findings were presented as part of a University of Washington Family Medicine Residency Network Faculty Development Project and as part of a University of Washington Family Planning Works in Progress session; final results were not presented.
References
- Tong STC, Makaroff LA, Xierali IM, et al. Proportion of family physicians providing maternity care continues to decline. J Am Board Fam Med. 2012;25(3):270-271. https://doi.org/10.3122/jabfm.2012.03.110256
- Nisen MB, Peterson LE, Cochrane A, Rubin SE. US family physicians’ intrauterine and implantable contraception provision: results from a national survey. Contraception. 2016;93(5):432-437. https://doi.org/10.1016/j.contraception.2016.01.004
- Wallace R, Dehlendorf C, Vittinghoff E, Gold KJ, Dalton VK. Early pregnancy failure management among family physicians. Fam Med. 2013;45(3):173-179. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed11&NEWS=N&AN=23463430
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine. 2018. http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120FamilyMedicine2018.pdf?ver=2018-06-15-112624-307. Accessed June 29, 2018.
- Herbitter C, Greenberg M, Fletcher J, Query C, Dalby J, Gold M. Family planning training in US family medicine residencies. Fam Med. 2011;43(8):574-581.
- Brahmi D, Dehlendorf C, Engel D, Grumbach K, Joffe C, Gold M. A descriptive analysis of abortion training in family medicine residency programs. Fam Med. 2007;39(6):399-403. Accessed May 25, 2018.
- Turk JK, Preskill F, Landy U, Rocca CH, Steinauer JE. Availability and characteristics of abortion training in US ob-gyn residency programs: a national survey. Contraception. 2014;89(4):271-277. https://doi.org/10.1016/j.contraception.2013.12.002
- Goodman S, Shih G, Hawkins M, et al. A long-term evaluation of a required reproductive health training rotation with opt-out provisions for family medicine residents. Fam Med. 2013;45(3):180-186. Accessed May 25, 2018.
- Steinauer JE, Turk JK, Fulton MC, Simonson KH, Landy U. The benefits of family planning training: a 10-year review of the Ryan Residency Training Program. Contraception. 2013;88(2):275-280. https://doi.org/10.1016/j.contraception.2013.02.006
- Coonrod RA, Kelly BF, Ellert W, Loeliger SF, Rodney WM, Deutchman M. Tiered maternity care training in family medicine. Fam Med. 2011;43(9):631-637.
- Tong ST, Makaroff LA, Xierali IM, Puffer JC, Newton WP, Bazemore AW. Family physicians in the maternity care workforce: factors influencing declining trends. Matern Child Health J. 2013;17(9):1576-1581. https://doi.org/10.1007/s10995-012-1159-8
- Young RA. Maternity Care Services Provided by Family Physicians in Rural Hospitals. J Am Board Fam Med. 2017;30(1):71-77. https://doi.org/10.3122/jabfm.2017.01.160072
- Chen FM, Huntington J, Kim S, Phillips WR, Stevens NG. Prepared but not practicing: declining pregnancy care among recent family medicine residency graduates. Fam Med. 2006;38(6):423-426.
- Carek PJ, Diaz V, Dickerson LM, Peterson L, Johnson S. Preparation for practice in family medicine: before and after duty hours. Fam Med. 2012;44(8):539-544.
- Peterson LE, Fang B, Puffer JC, Bazemore AW. Wide Gap between Preparation and Scope of Practice of Early Career Family Physicians. J Am Board Fam Med. 2018;31(2):181-182. https://doi.org/10.3122/jabfm.2018.02.170359
- Shih G, Zhang Y, McNeil S. Continuing reproductive education for advanced training efficacy: a novel collaborative program to support abortion practice and family planning advocacy beyond residency. STFM Education Column. http://www.stfm.org/NewsJournals/EducationColumns/2018JulyEducationColumn. Published 2018. Accessed September 5, 2018.
- Jones RK, Jerman J. Abortion Incidence and Service Availability In the United States, 2014. Perspect Sex Reprod Health. 2017;49(1):17-27. https://doi.org/10.1363/psrh.12015
- Block A, Dehlendorf C, Biggs MA, McNeil S, Goodman S. Postgraduate experiences with an advanced reproductive health and abortion training and leadership program. Fam Med. 2017;49(9):706-713.
- Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of Intended Scope of Practice for Family Medicine Residents With Reported Scope of Practice Among Practicing Family Physicians. JAMA. 2015;314(22):2364-2372. https://doi.org/10.1001/jama.2015.13734




There are no comments for this article.