Background and Objectives: The goal of this study was to investigate the impact of medical students functioning in the role of scribe on students’ learning, medical practice, and preceptor.
Methods: Third-year students from the University of North Dakota School of Medicine and Health Sciences volunteered and were trained to function in the role of scribe. Preceptors also completed training to have students scribe in their practice. The students, preceptors, and staff completed questionnaires assessing perceptions of the impact on the student, the practice, and the provider. We elicited comments and concerns from students, staff, and preceptors.
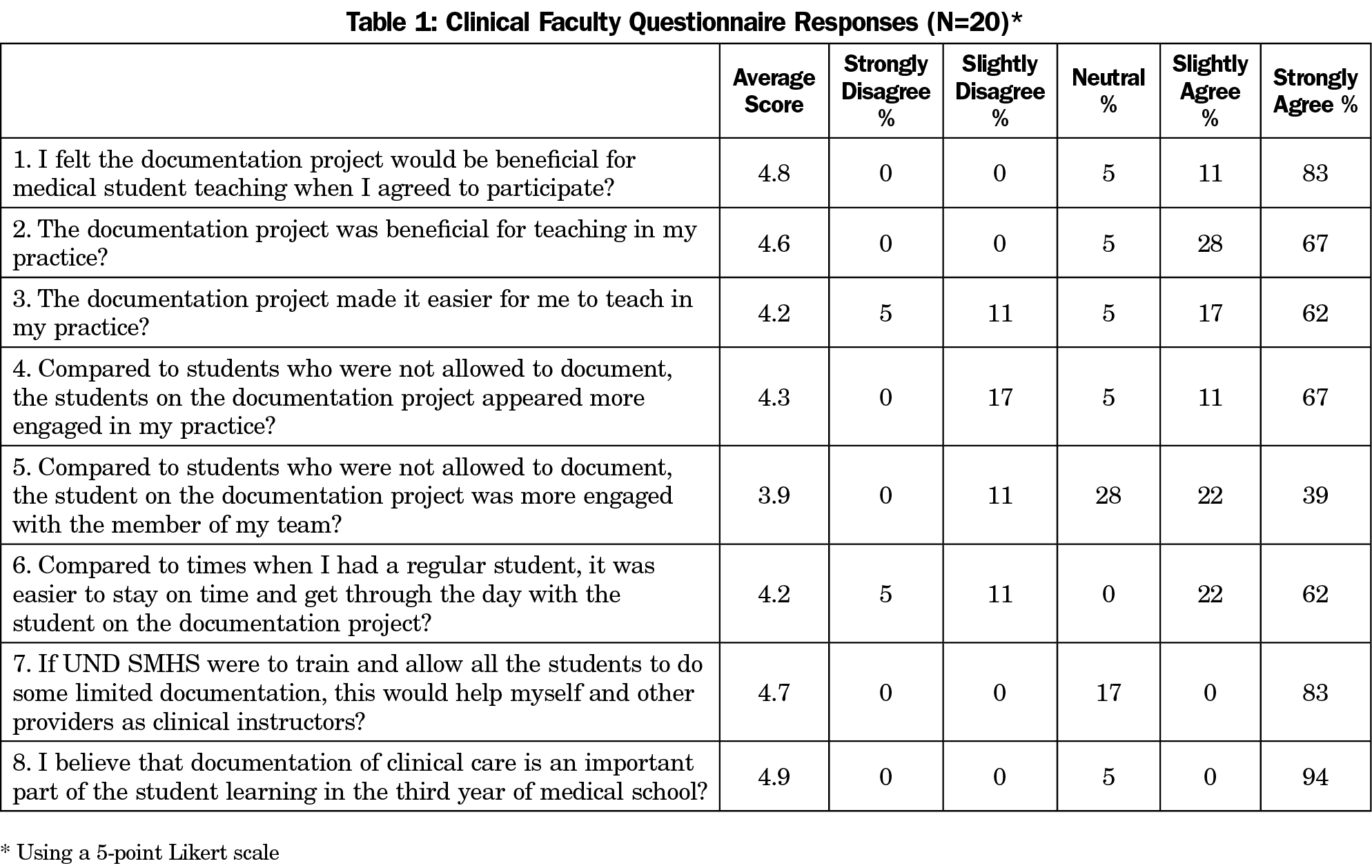
Results: All groups perceived medical students’ scribing as helpful for teaching medical students in the clinical setting, with an average questionnaire score for all groups of 4.7/5. The students reported it was a positive experience. It allowed them to be more engaged, improved the learning environment, and didn’t detract from clinical learning. Staff reported that students were more engaged, and scribing did not impact time management. Preceptors reported that students were more engaged in the practice, and with their team. Preceptors reported it was also easier to teach, and easier to stay on time with medical students scribing. All reported that documentation was important to learn in the third year of medical school, and that students should be trained to function in a limited scribe role.
Conclusions: Allowing students to document in the electronic medical record provides many benefits to students and preceptor practices and should be encouraged and advocated for in medical education.
The introduction of the electronic health record (EHR) has transformed clinical practice over the past few decades, impacting physician workflow in both positive and negative ways.1
EHR use is tied to reimbursement, which pushed adoption rates to 67% by March 2016.3 EHR implementation has proved challenging for physicians, and contributed to physician burnout.4-6 The increased time required for documentation has not been offset by the efficiencies promised with EHR use.7-9 Preceptors comment that this has made it harder to find time to teach. Medical schools are challenged to find physicians willing to be medical student preceptors, and the time required for EHR work further reduces their available teaching time. The use of students as scribes to assist with documentation provides dual benefits. Physician satisfaction with teaching increases and students receive early experience with patient documentation. In practices where providers have scribes, job satisfaction, productivity, and reimbursement all increase.2,4,11,12
The Association of American Medical Colleges (AAMC) recommends that all medical school students gain some EHR competency prior to residency. The Alliance for Clinical Education (ACE) and the Society of Teachers of Family Medicine (STFM) state that learning to document and use the EHR is an essential skill for students.15,16 Physicians comment that they understand the need to have students document in the EHR. Gaining access to the EHR for students has been a challenge medical schools must overcome. The American Medical Association (AMA) and AAMC advocate for increased student access.13,14
The Centers for Medicaid and Medicare Services (CMS) have also changed their stance on student documentation in the EHR.17 EHR access is still limited by some health systems for security or compliance reasons.18 This study investigated a novel method that allows students to document in the EHR. The study looked at students in the scribe role to determine benefits to faculty in the areas of increased productivity and provider satisfaction.2,12,19 Allowing students to act in the scribe role should improve EHR skills and increase engagement. For preceptors, it has the potential to reduce their documentation burden and increase teaching satisfaction.
The Institutional Review Boards of the University of North Dakota and Sanford Health exempted this research proposal. We recruited students from the University of North Dakota School of Medicine and Health Sciences (UND SMHS) from May 2016 to July 2017. When a student was scheduled with a provider and system that allowed scribes, they were asked if they wished to participate. Volunteer students were then trained in the role of scribe. An extra 4 to 6 hours of training was designed to increase EHR skills in the EPIC EHR. First, Sanford Health led training in advanced EPIC use, and proper scribe documentation. Then the students practiced in the EPIC training environment, under the lead physician. They documented clinical visits using case videos for seven different common visits. If the scribed notes met requirements for completeness and accuracy, the students were given a certificate of completion and were scribe-capable. We developed compliant attestation statements indicating the students’ role as scribe. Although the students’ primary role was to learn, they also functioned as documentation scribe on a few patients daily. The learning sequence was as follows: the student entered the room to interview the patient and take an appropriate history and physical; (2) they then presented the patient to the preceptor and discussed the case; (3) they entered the room together; and (4) while the preceptor interviewed and examined the patient, the student entered the visit information into the EHR as scribe. Students, faculty preceptors, and staff (registered nurses, licensed practical nurses, or certified medical assistants who worked with the student) completed surveys at the conclusion of the study to ascertain the impact on the student, the preceptor, and the practice. The survey elicited comments from students, faculty, and staff.
Tables 1-3 summarize item responses by group. Among clinical faculty, 18 returned surveys; among clinical staff; 11 returned surveys; among students, 20 returned surveys. Overall, 49 of 53 participants completed surveys.
All participants reported that documenting would be useful. The faculty and clinical staff reported that documenting was beneficial for teaching and should be learned in the third year of medical school. The students did not think documenting detracted from their student role. Learning to document was beneficial for training, and should be learned in the third year.
Qualitative feedback explained variability. The students’ comments included statements such as “it was a great experience,” “I would recommend for everyone,” and “I learned a lot of things in the EMR, not just note writing but how to navigate it to find information.” The preceptor and staff indicated that the students appeared more engaged. They also clarified answers that fell below 3, such as “Harder at the time since the record gets tied up/hard to flip through the record.”
The EHR is a tool providers use daily. By residency, students need skills to navigate the EHR to appropriately document care. CMS rule changes open the door for students to document in the EHR. Faculty noted students with increased documentation responsibilities are more engaged overall. In addition, decreases in the documentation burden provided by student scribes appeared to make it easier for physicians to teach in their practice. Some clinical staff did not feel it helped with time, and when the findings were discussed with staff, not all teaching time lost in clinic was made up for by documenting. This study included only the Epic EHR, although skills of documenting and using an electronic health record should transfer to other settings and other EHRs. With new CMS rules, this study should serve as an early indicator that students can have a positive impact while acquiring skills to use EHRs. Further research into how the new CMS rules have affected the opportunity for students to learn to document in the EHR would increase knowledge of the rule’s impact.
Acknowledgments
Presentations: STFM Medical Student Education Conference, MSEDI participant, “Getting the Pre-Doc Back into Documentation” Students Acting as Scribe during their Family Medicine Rotation, Anaheim, CA, February 10, 2017.
North Dakota Chapter of the American College of Physicians Annual Meeting 2017; Getting the Predoc Back into Documentation: The Medical Student in the Role of Scribe, Benefits for Faculty and Student, November 22, 2017.
References
- Baumann LA, Baker J, Elshaug AG. The impact of electronic health record systems on clinical documentation times: A systematic review. Health Policy. 2018;122(8):827-836. https://doi.org/10.1016/j.healthpol.2018.05.014
- Shay R. EHR Adoption Rates and Statistics: 2012 - 2017 [Internet]. Practice Fusion. https://www.practicefusion.com/blog/ehr-adoption-rates/. Accessed July 27, 2018.
- Blackwelder R. Practical Approach to Walking in Balance. Dean’s Hour. Grand Forks, ND: University of North Dakota School of Medicine and Health Sciences; 2017.
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. https://doi.org/10.1016/j.mayocp.2015.08.023
- Downing NL, Bates DW, Longhurst CA. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med. 2018 03;169(1):50–1.
- Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12(5):505-516. https://doi.org/10.1197/jamia.M1700
- Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008;77(5):291-304. https://doi.org/10.1016/j.ijmedinf.2007.09.001
- Joukes E, Abu-Hanna A, Cornet R, de Keizer NF. Time Spent on Dedicated Patient Care and Documentation Tasks Before and After the Introduction of a Structured and Standardized Electronic Health Record. Appl Clin Inform. 2018;9(1):46-53. https://doi.org/10.1055/s-0037-1615747
- Bank AJ, Gage RM. Annual impact of scribes on physician productivity and revenue in a cardiology clinic. Clinicoecon Outcomes Res. 2015;7:489-495. https://doi.org/10.2147/CEOR.S89329
- McCormick BJ, Deal A, Borawski KM, et al. Implementation of medical scribes in an academic urology practice: an analysis of productivity, revenue, and satisfaction. World J Urol. 2018;36(10):1691-1697. https://doi.org/10.1007/s00345-018-2293-8
- Heaton HA, Castaneda-Guarderas A, Trotter ER, Erwin PJ, Bellolio MF. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34(10):2018-2028. https://doi.org/10.1016/j.ajem.2016.07.056
- Alliance for Clinical Education. Letter of Support to LCME emphasizing Standard 7.8 Curricular Content - Communication Skills [Internet]. 2015 http://allianceforclinicaleducation.org. Accessed July 27, 2018.
- Society of Teachers of Family Medicine. Preceptor Guidelines Document: Student Use of Electronic Health Records [Internet]. 2014. Available from: https://www.stfm.org. Accessed July 27, 2018.
- Association of American Medical Colleges. Compliance Advisory: Electronic Health Records (EHRs) in Academic Health Centers [Internet]. Association of American Medical Colleges; 2014. https://www.aamc.org/em/aamc/compliance_advisory.pdf. Accessed July 27, 2018.
- American Medical Association. AMA, Regenstrief Institute help increase EHR training in med schools [Internet]. American Medical Association; 2017. https://www.ama-assn.org/press-center/press-releases/ama-regenstrief-institute-help-increase-ehr-training-med-schools. Accessed July 27, 2018.
- Power DV, Byerley JS, Steiner B. Policy Change From the Centers for Medicare and Medicaid Services Provides an Opportunity to Improve Medical Student Education and Recruit Community Preceptors. Acad Med. 2018;93(10):1448-1449. https://doi.org/10.1097/ACM.0000000000002245
- Palabindala V, Pamarthy A, Jonnalagadda NR. Adoption of electronic health records and barriers. J Community Hosp Intern Med Perspect. 2016;6(5):32643. https://doi.org/10.3402/jchimp.v6.32643
- Gidwani R, Nguyen C, Kofoed A, et al. Impact of Scribes on Physician Satisfaction, Patient Satisfaction, and Charting Efficiency: A Randomized Controlled Trial. Ann Fam Med. 2017;15(5):427-433. https://doi.org/10.1370/afm.2122





There are no comments for this article.