Background and Objectives: Teaching medical students patient-centered approaches to weight loss counseling occurs in myriad ways. We examined lectures and direct faculty observation to see which was associated with better patient-centered care in medical students, measured by both self-perception and independent observer evaluation.
Methods: Third- and fourth-year students attending one medical school were surveyed regarding their education in (1) weight loss and health behavior counseling, (2) obesity stigma, and (3) whether they had experienced direct faculty observation of their weight loss counseling. Several weeks later, the students were observed during a standardized patient encounter for obesity and an obesity-relevant comorbidity. A postencounter survey assessed overall student satisfaction with the encounter and with the care they provided. Independent coders rated their patient-centered communication using a validated measure.
Results: There was no consistent association between any dependent variable and student ratings of adequacy of instruction, nor with instructional content. Direct faculty observation was not associated with overall encounter satisfaction or their overall patient-centeredness. However, experiences with direct faculty observation were significantly and positively associated with students’ perceptions of patient engagement (b=0.1, P=.05), and with independent coders’ ratings of student friendliness (b=0.13, P=.01), responsiveness (b=0.113, P=.03), and lower student anxiety (b=-0.1, P=.01).
Conclusions: Independent observation and self-report of instruction adequacy and content had no consistent association with care quality. However, direct faculty observation predicted improvement in both student self-reports and independent observer ratings of students’ interpersonal quality of care. Further work is needed to define optimal methods of imparting patient-centered care.
More than one-third of US adults meet obesity criteria, which confers significant additional morbidity and mortality risk.1,2 Physicians need to effectively communicate these risks and discuss weight management strategies, yet research shows that bias against patients with obesity3-8 exists and patients who feel judged or stigmatized by providers are less likely to attempt modifying their lifestyle,9 and may avoid or delay seeking care.10 Conversely, positive interactions correlate with improved patient satisfaction and adherence to treatment and outcomes.10-14 To improve patient experiences and outcomes, medical trainees must learn patient-centered approaches to discussing obesity.
To facilitate patient-centered approaches to lifestyle counseling, the medical education community must understand which methods improve patient-centered care. Therefore, we investigated whether direct faculty observation, lectures, or group activities were associated with improved patient-centered care quality in medical students.
Participants
In 2015-2016, we surveyed 150 third- and fourth-year students from one medical school about their obesity and lifestyle counseling education. Several weeks following the survey (mean 8.4, range 3-20), students participated in a standardized patient (SP) scenario with obesity and an obesity-related comorbidity. We administered a survey afterwards evaluating students’ self-perception of their care. The encounter was recorded and independent observers assessed patient-centered communication/behavior using a validated measure.15 Our institutional review board considered this research exempt from review.
Baseline Questionnaire
The initial survey assessed whether the students received adequate instruction regarding weight loss counseling using a 7-point Likert scale, from “strongly disagree” to “strongly agree.” The survey asked students about direct faculty observation with the item “During medical school, faculty members personally observed me providing advice/counseling about weight related behavior changes.” Similarly, the survey asked students whether they had received adequate instruction on providing weight loss counseling or counseling on other behavioral changes, and whether they had lectures, discussions or group activities about obesity stigma or health disparities.
Standardized Patient Scenario
Medical school faculty proficient in SP assessment and obesity management designed the SP encounter to evoke weight-loss discussions. The scenario was portrayed by four male SPs with obesity and severe knee osteoarthrities who desired to avoid future disability. All students initiated a weight-loss discussion.
Four members of the team trained in coding patient-provider communication evaluated the encounters using the Roter Interaction Analysis System (RIAS), a validated tool for measuring patient-centered communication.15-19 RIAS breaks down speech into specific types of utterances (eg, biomedical data gathering, positive rapport building) and calculates a patient-centeredness score. Coders also rated the students’ perceived anger, anxiety, dominance, interest, friendliness, responsiveness, sympathy, hurry, respectfulness, and interactivity on a 7-point scale. Additionally, coders evaluated student behaviors on items like “the doctor displayed an open, receptive and interested posture” and “the doctor greeted the patient warmly.” Items were amalgamated into the patient-centered behavior index. Finally, coders indicated whether they would “recommend this health care provider to my family or friends.”
Postencounter Questionnaire
Postencounter questionnaires measured students’ self-assessment of the visit using a 7-point Likert scale. Students were asked how well they had addressed patient needs, the interactivity of the patient, how satisfied they were with the emotional support and information they had provided, and their overall satisfaction.
Data Analysis
Correlations between coders’ RIAS scores were calculated on 15% of the encounters. We assessed bivariate associations using linear regression, and then used multivariate regression to assess associations adjusted for covariates. Initial survey responses were independent variables. Student demographic characteristics (age, race, marital status, gender, and BMI category), SP, and coder were covariates. Dependent variables consisted of RIAS score and PC Behavior Index score, coder ratings of the student, and postencounter satisfaction measures.
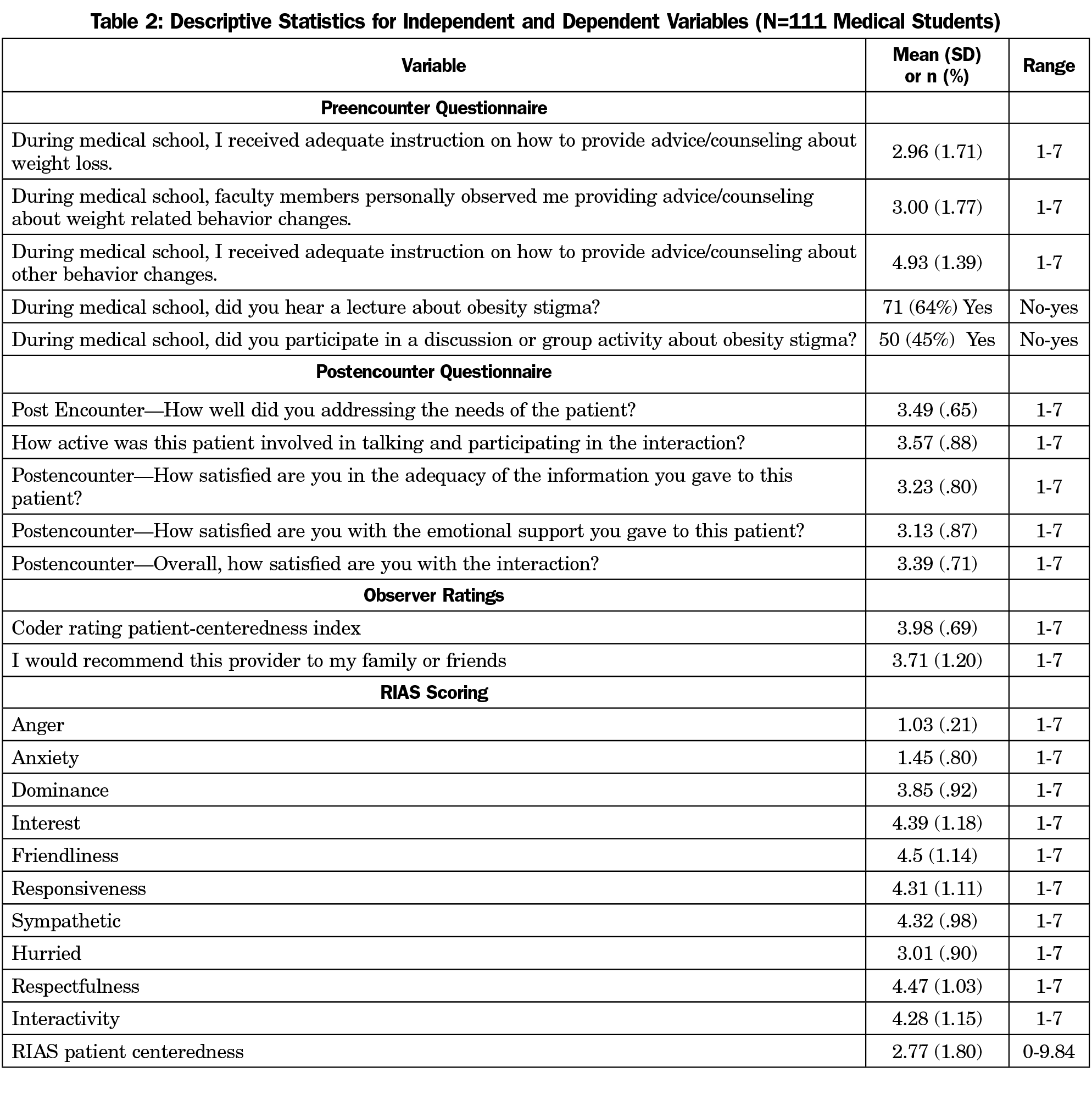
One hundred thirty-six students (91%) completed the survey; 117 (78%) completed the standardized patient visit. We omitted six encounters due to audio issues, leaving 111 (74%) for review. Table 1 includes a summary of the students’ attributes; Table 2 presents distributions of key variables.
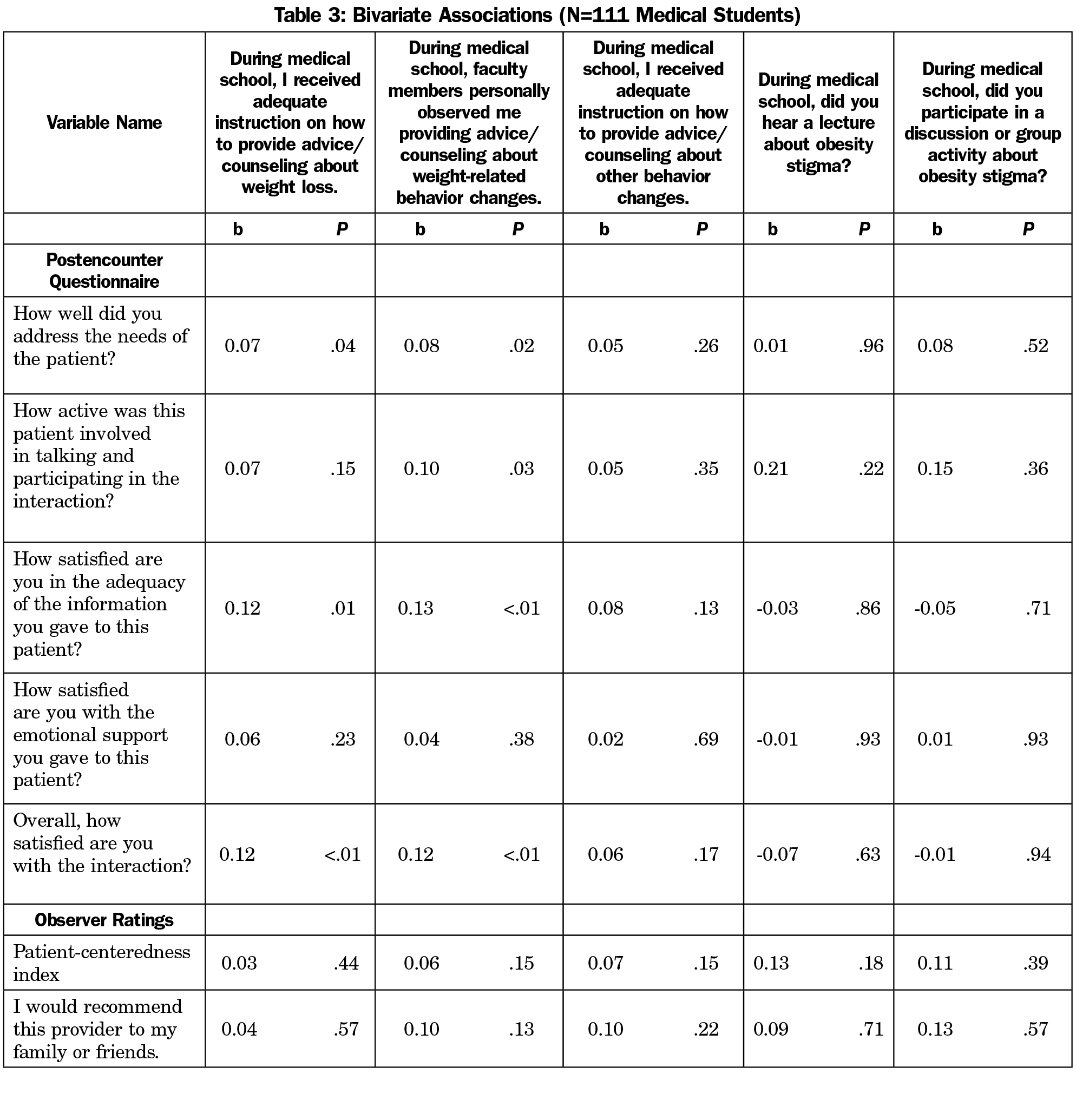
Bivariate analyses (Table 3) revealed positive associations between receiving adequate instruction in weight loss counseling and student satisfaction with addressing the needs of the patient (b=0.07, P=.04), the information they provided (b=0.12, P=.01), and the overall encounter (b=0.12, P=.003). There were positive associations between faculty observation and satisfaction with addressing patient needs (b=0.08, P=.02), patient involvement (b=0.1, P=.03), information given (b=0.12, P=.001), and the overall interaction (b=0.12, P=.002).
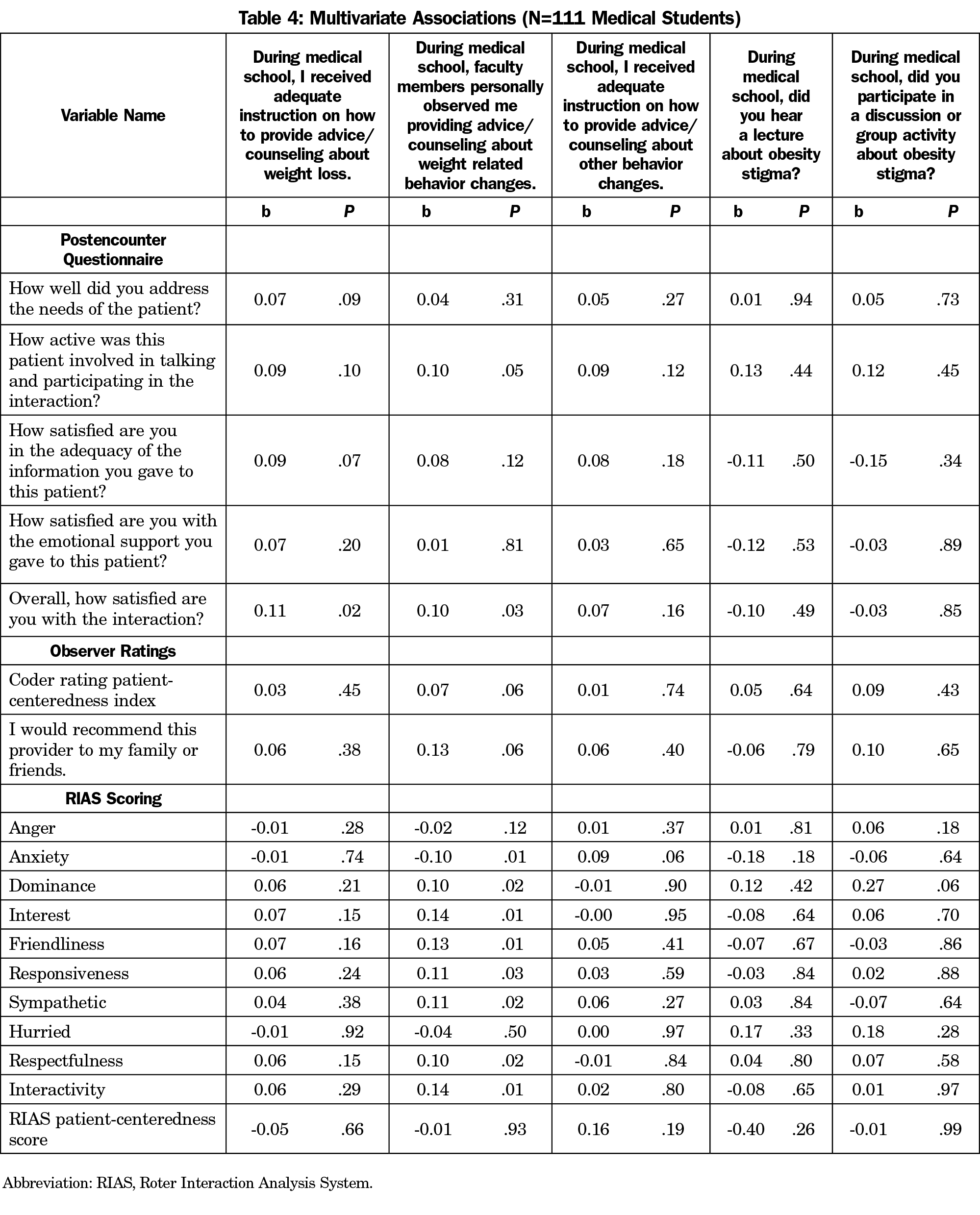
In multivariate analysis (Table 4), receiving adequate instruction about weight loss was associated with students’ overall satisfaction with the interaction (b=0.11, P=.02) but not with other measures. Observation by faculty was associated with lower student anxiety (b=-0.1, P=.01), and higher ratings of students’ interest (b=0.14, P=.01), friendliness (b=0.13, P=.01), sympathy (b=0.11, P=.02), respectfulness (b=0.1, P=.02) and interactivity (b=0.14, P=.01) during the encounter.
Neither hearing lectures about, nor participating in discussions or small groups regarding obesity stigmata was significantly associated with any dependent variable in bivariate or multivariate analysis.
Many studies on direct observation exist; however objective data regarding changes in clinical skills is lacking.20 Moreover, research has focused on direct faculty observation without comparing other forms of teaching patient-centered care. This study uniquely compares different learning styles like small groups and lectures with direct observation. Bivariate analysis (Table 3) of faculty observation demonstrated significant improvement in how the student felt about the encounter though this effect largely disappeared on multivariate analysis (Table 4). Multivariate analysis demonstrated that faculty observation of students’ weight loss counselling was associated with higher coder ratings of student interest, friendliness, sympathy, respectfulness, interactivity, and with lower anxiety ratings. There are three compelling reasons why direct observation by faculty may have a beneficial impact. First, direct observation typically involves some type of feedback, which can contribute to student confidence in subsequent encounters.21 Second, role modeling counseling techniques may provide an example of patient-centered behavior. Third, receiving faculty observation may be connected to more counseling experiences during rotations and improved proficiency at delivering lifestyle counseling. Further studies should elucidate the specific mechanisms by which faculty observation is associated with improved delivery of lifestyle counseling.
Studies suggest patient-centered care is an important predictor of health care outcomes including patient adherence and care satisfaction.10,22,23 Thus, medical schools are incorporating training in patient-centered care via lectures and small group activities, yet no consistent difference in the effectiveness of independent coder ratings or the postencounter survey was found in either bivariate (Table 3) or multivariate (Table 4) analysis. Although receiving adequate instruction was associated with some positive student measures, the effect disappeared in multivariate analysis. The fact that receiving adequate instruction or discussions regarding weight-loss counseling, weight stigma, and health disparities were not consistently associated was surprising. There may be insufficient variation in the educational experiences at a single medical school to show statistical differences in outcomes. Another possibility is that the teaching modality is less important than nonverbal cues delivered by faculty.24,25 Nonetheless, if confirmed, these results suggest that the current focus on discussions and lectures to promote patient-centered care are insufficient and more education emphasis should be placed on the faculty-student interaction. This may also have educational implications in other areas that would benefit from improved patient-centered care, including chronic pain and chronic disease states.
Limitations
First, the study was conducted at a single medical school. Second, these were standardized patients and scripted encounters, which may not reflect real-world encounters including a greater mix of patient characteristics. Finally, our study relied heavily on student self-reporting. Combining this with objective data regarding topics addressed and time spent in educational modalities would be helpful.
Our study analyzed different teaching modalities and found that direct faculty observation is associated with improved delivery of patient-centered obesity care compared to other teaching methods. Further work should include other schools and instruction styles while evaluating the patient experience to determine optimal educational methods promoting patient-centered care.
Acknowledgments
Portions of this project were presented at North American Primary Care Research Groups (NAPCRG) on November 16, 2018, in Chicago, Illinois.
References
- Centers for Disease Control and Prevention. Adult Obesity Facts. https://www.cdc.gov/obesity/data/adult.html. Accessed April 9, 2019.
- Segula D. Complications of obesity in adults: a short review of the literature. Malawi Med J. 2014;26(1):20-24.
- Brown I. Nurses’ attitudes towards adult patients who are obese: literature review. J Adv Nurs. 2006;53(2):221-232. https://doi.org/10.1111/j.1365-2648.2006.03718.x
- Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001;25(8):1246-1252. https://doi.org/10.1038/sj.ijo.0801681
- Latner JD, O’Brien KS, Durso LE, Brinkman LA, MacDonald T. Weighing obesity stigma: the relative strength of different forms of bias. Int J Obes. 2008;32(7):1145-1152. https://doi.org/10.1038/ijo.2008.53
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319-326. https://doi.org/10.1111/obr.12266
- Phelan SM, Dovidio JF, Puhl RM, et al. Implicit and explicit weight bias in a national sample of 4,732 medical students: the medical student CHANGES study. Obesity (Silver Spring). 2014;22(4):1201-1208. https://doi.org/10.1002/oby.20687
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941-964. https://doi.org/10.1038/oby.2008.636 PMID:19165161
- Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity (Silver Spring). 2013;21(10):2146-2152. https://doi.org/10.1002/oby.20384
- Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229-239. https://doi.org/10.3122/jabfm.2011.03.100170
- Epstein RM, Street RL, Jr. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, MD: National Cancer Institute, Publication No. 07-6225; 2007. https://cancercontrol.cancer.gov/brp/docs/pcc_monograph.pdf. Accessed April 9, 2019.
- Bertakis KD, Azari R. Determinants and outcomes of patient-centered care. Patient Educ Couns. 2011;85(1):46-52. https://doi.org/10.1016/j.pec.2010.08.001
- Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796-804.
- Wanzer MB, Booth-Butterfield M, Gruber K. Perceptions of health care providers’ communication: relationships between patient-centered communication and satisfaction. Health Commun. 2004;16(3):363-383. https://doi.org/10.1207/S15327027HC1603_6
- Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46(4):243-251. https://doi.org/10.1016/S0738-3991(02)00012-5
- Beach MC, Saha S, Korthuis PT, et al. Differences in patient-provider communication for Hispanic compared to non-Hispanic white patients in HIV care. J Gen Intern Med. 2010;25(7):682-687. https://doi.org/10.1007/s11606-010-1310-4
- Price EG, Windish DM, Magaziner J, Cooper LA. Assessing validity of standardized patient ratings of medical students’ communication behavior using the Roter interaction analysis system. Patient Educ Couns. 2008;70(1):3-9. https://doi.org/10.1016/j.pec.2007.10.002
- Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979-987. https://doi.org/10.2105/AJPH.2011.300558
- Roter D, Lipkin M Jr, Korsgaard A. Sex differences in patients’ and physicians’ communication during primary care medical visits. Med Care. 1991;29(11):1083-1093. https://doi.org/10.1097/00005650-199111000-00002
- Kogan JR, Holmboe ES, Hauer KE. Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA. 2009;302(12):1316-1326. https://doi.org/10.1001/jama.2009.1365
- Hamburger EK, Cuzzi S, Coddington DA, et al. Observation of resident clinical skills: outcomes of a program of direct observation in the continuity clinic setting. Acad Pediatr. 2011;11(5):394-402. https://doi.org/10.1016/j.acap.2011.02.008
- Bertakis KD, Azari R. Patient-centered care is associated with decreased health care utilization. J Am Board Fam Med. 2011;24(3):229-239. https://doi.org/10.3122/jabfm.2011.03.100170
- Epstein R, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, US Department of Health and Human Services; 2007.
- Phillips SP. Blinded by belonging: revealing the hidden curriculum. Med Educ. 2013;47(2):124-125. https://doi.org/10.1111/medu.12103
- Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med. 1998;73(4):403-407. https://doi.org/10.1097/00001888-199804000-00013




There are no comments for this article.