Despite existing guidelines that recommend regular reproductive and sexual health counseling for adolescents, studies show that providers infrequently discuss sexual health with patients due to lack of comfort, time, and training, beginning in medical school.1-11 The absence of standardized sexual health curricula in US medical schools results in variable and often inadequate curricula.12-13 Programs promoting medical students as sexual health educators have demonstrated improved adolescents’ and medical students’ sexual health knowledge and changes in medical student attitudes toward sexual health issues.14-17 In one study, participation in a peer-led sexual health education project improved medical students’ confidence in discussing four sexual health topics with patients of all age groups.18 Our study aimed to measure the impact of teaching in Sex Ed by Brown Med, a preclinical elective for medical students at The Warren Alpert Medical School of Brown University (AMS), on confidence in discussing sexual health topics and using nine advanced interviewing skills.
BRIEF REPORTS
Impact of Teaching Sexual Health Education on Medical Students
Sarah J. F. Bourne, BA | Charlotte M. Lee, BA | Elizabeth Taliaferro, BA | Angela Y. Zhang, BA | Natasha F. Dalomba, BA | Constance Panton, BA | Mary B. Roberts, MS | Susanna Magee, MD, MPH
Fam Med. 2020;52(7):518-522.
DOI: 10.22454/FamMed.2020.939791
Background and Objectives: Physician discomfort, embarrassment, and perceived lack of time and/or training all play a role in preventing physicians from discussing sexual health with patients. Past research shows this discomfort begins in medical school. We aimed to determine whether teaching sexual health education increases medical students’ self-efficacy in discussing sexual health topics with adolescents.
Methods: We emailed a retrospective pre/postsurvey to all medical students who taught sexual health education in a local middle school through Sex Ed by Brown Med (N=61).
Results: Participation in Sex Ed by Brown Med improves self-efficacy in discussing nine sexual health topics and in performing nine advanced interviewing skills relevant to sexual health in a retrospective analysis using self-reported data.
Conclusions: Programs similar to Sex Ed by Brown Med may be useful in improving medical students’ ability to adequately care for their patients’ sexual health by making future clinicians more comfortable when discussing the important topic of sexuality, and concurrently providing evidence-based comprehensive sexual health education to middle school students. Further research is needed to determine the impact of our program (and similar programs) before disseminating this model of sexual education.
About the Program
Sex Ed by Brown Med, a program designed to train medical students to teach sexual health education to 7th graders, began in 2014 after a physician and medical student approached a local middle school principal about the need for better sexual health education. Now, a memorandum of agreement exists with the school district and the medical students work directly with school leaders to schedule lessons. The program trains 30 to 35 self-selected volunteer medical students (20%-25% of the class) to teach a 12-lesson sexual health education program.19
Standard sexual health counseling curriculum at AMS includes approximately 5 hours of training for medical students. Our program adds 20-30 hours of training through service learning, including 1-hour sessions prior to each lesson and hours spent teaching each lesson.20 The 1-hour sessions prepare medical students for the upcoming lesson and teach skills such as using inclusive language and asking and answering uncomfortable questions; while sessions are geared toward preparing volunteers for the classroom, we hypothesize that these advanced interviewing skills are translatable to clinical settings. Our program has been shown to increase the 7th grade students’ knowledge of sexual health topics, but the impact on medical student participants has never been measured.19
Data Collection
In October 2018, we sent a voluntary, retrospective pre/postsurvey with follow up emails to all former participants in Sex Ed by Brown Med (N=114). We selected a retrospective pre/postsurvey given their validation in educational interventions: once respondents have knowledge about a subject, they are more likely to accurately assess their degree of change and less likely to overestimate their knowledge compared to traditional pretest-posttest studies.21-24 To be eligible, respondents must have taught at least one lesson and could not be teaching with the program at the time of the survey. Question types included multiple choice and Likert scale. Surveys were anonymous and participants were informed that their responses would be used for research purposes. Participation was not linked to a course grade. We entered survey participants into a raffle for a chance to win a Sex Ed by Brown Med logo mug. The manager of the Institutional Review Board at Brown University approved the study as exempt under policies surrounding quality improvement research.
Analysis
We calculated frequencies and percentages for all variables, and we used Wilcoxon signed rank tests to examine change in self-efficacy for advanced interviewing skills and ability to discuss sexual health topics before and after participation in the program. We calculated change in self-efficacy scores to examine differential changes by selected demographic and program participation variables. We used nonparametric tests to statistically detect the differential change by the selected variables. We set significance at P≤.05, and conducted all analyses using IBM SPSS Statistics version 23.
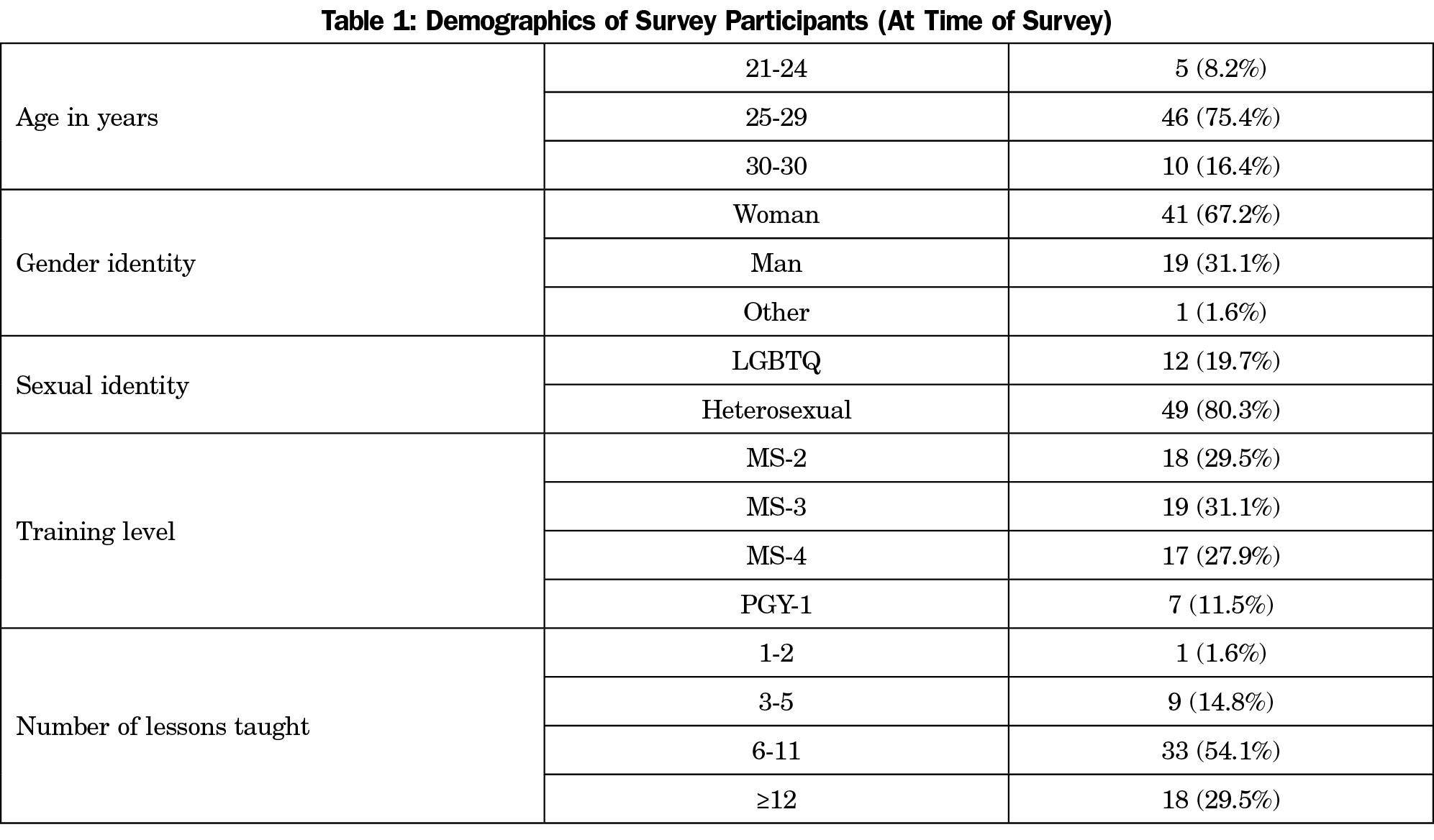
A total of 61 of 114 eligible students completed the questionnaire (53.5%). Table 1 shows baseline demographic characteristics of the survey participants.
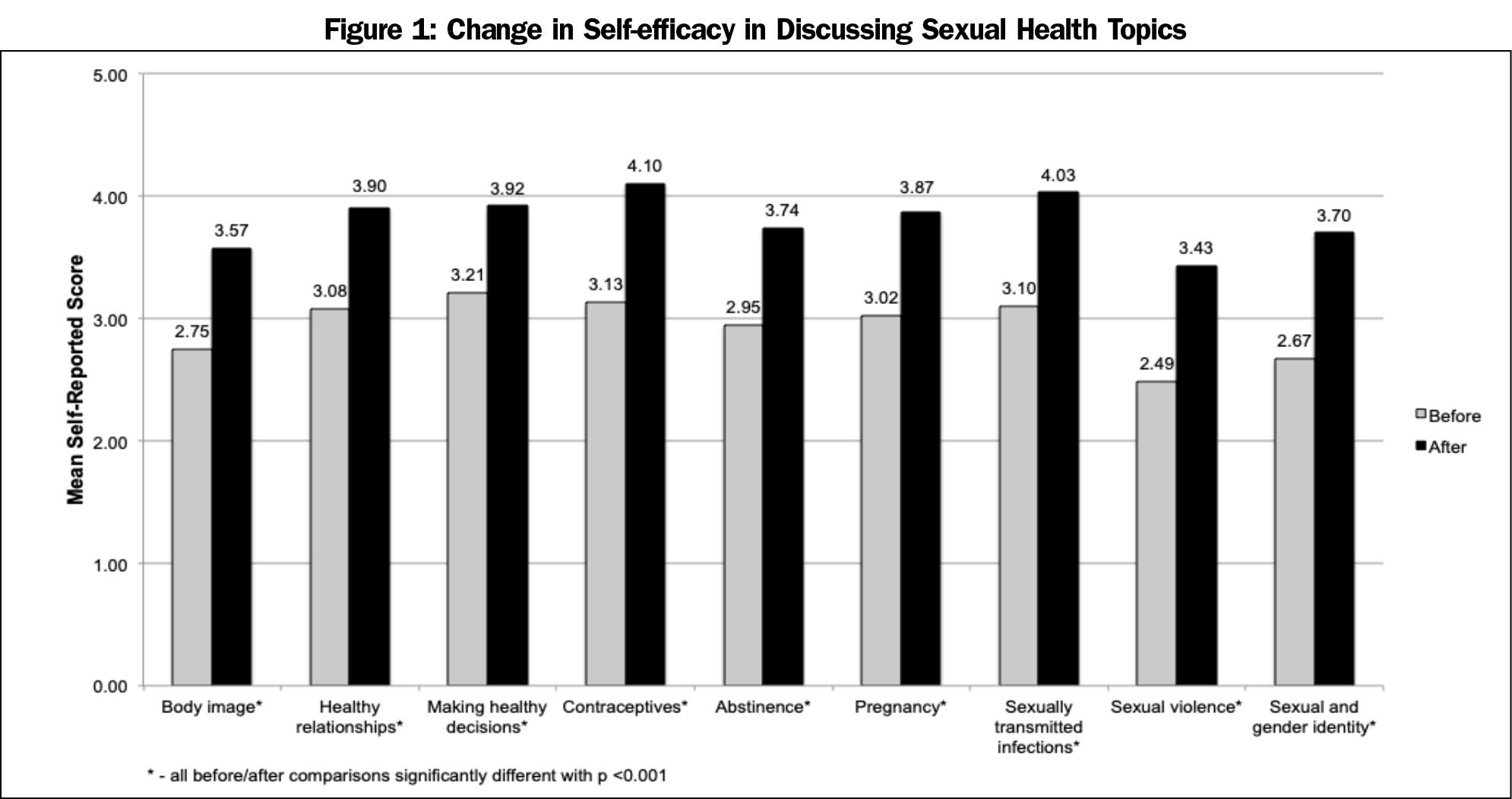
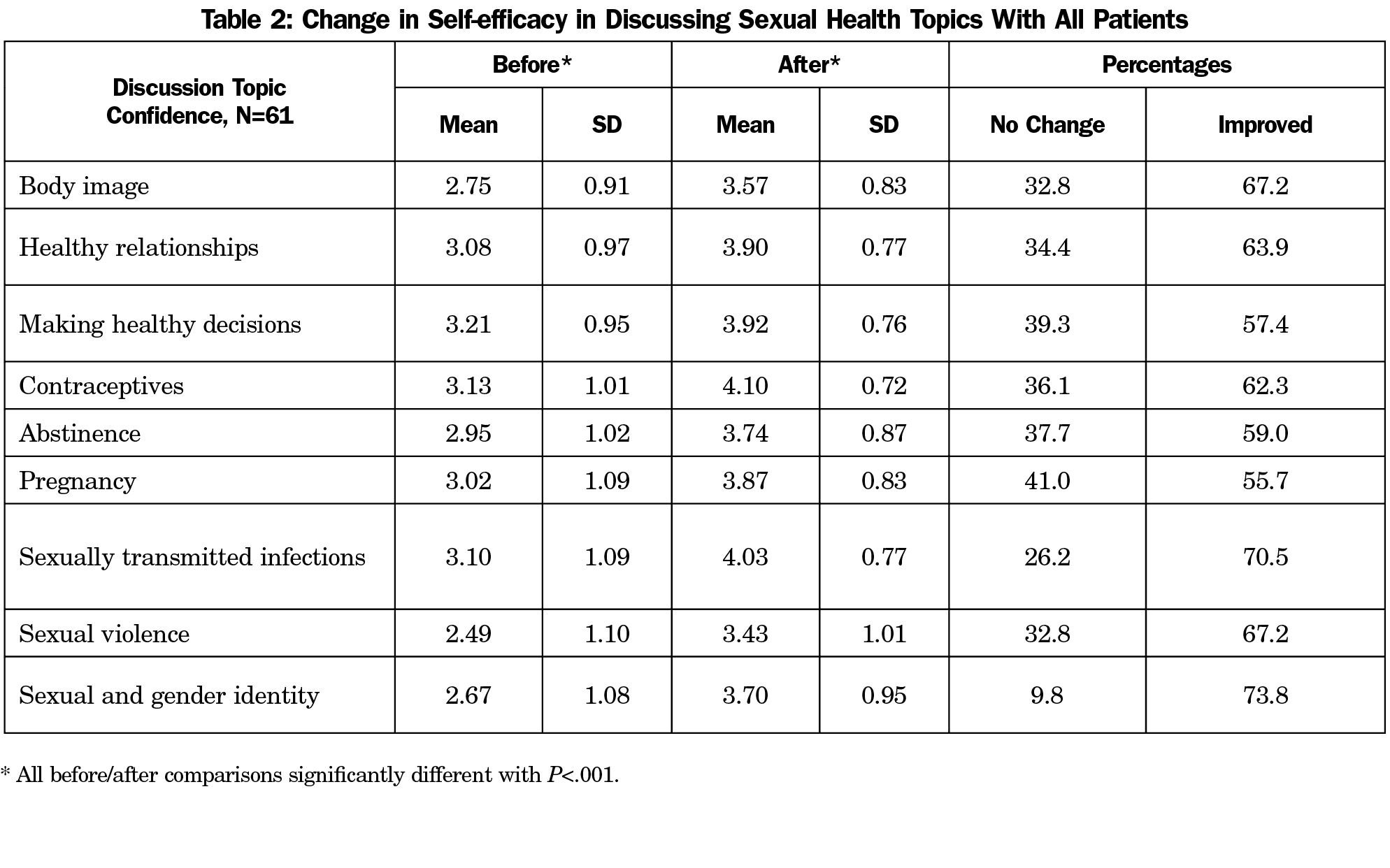
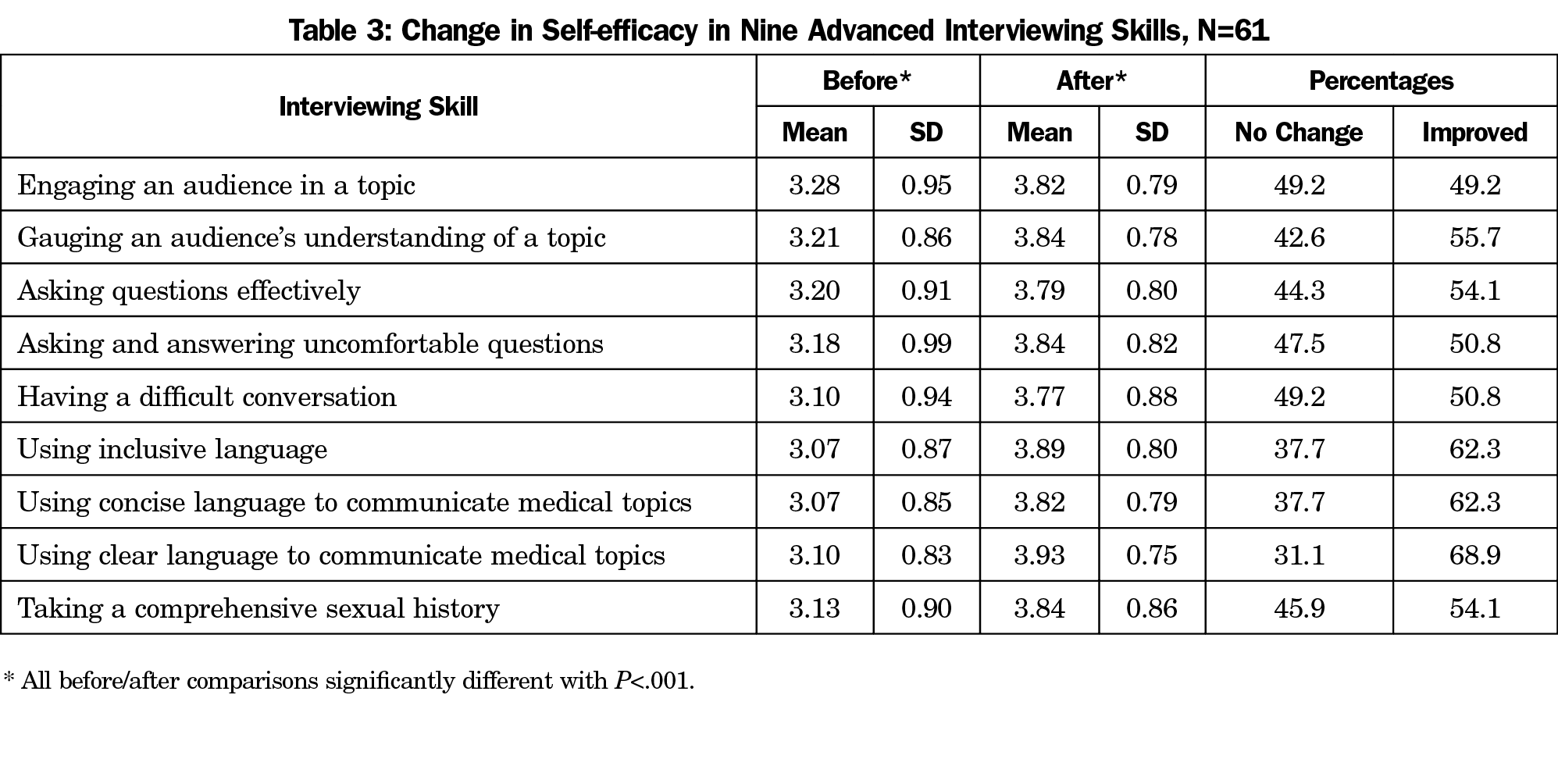
Self-efficacy in discussing all sexual health topics and using all advanced interviewing skills improved (Figure 1, Table 2, and Table 3). Further analysis found a dose-response relationship between the number of lessons taught and self-efficacy in discussion of abstinence, pregnancy, and making healthy decisions (P=.02, .01, and .01, respectively).
Respondents who identified as men reported a greater increase in self-efficacy in discussing pregnancy compared to women (1.350 vs 0.610, P=.02). Respondents who identified as LGBTQ reported a greater increase in self-efficacy in discussing seven categories than non-LGBTQ-identifying participants.
The majority of respondents agreed or strongly agreed that participating in this elective helped them feel more prepared to discuss sexual health topics with adolescents (90.1%) and other age groups (72.1%), and that participating in this program increased their self-efficacy in discussing sexual health topics with adolescents (91.8%) and other age groups (83.6%). Moreover, 75.6% of respondents agreed or strongly agreed that they used the skills learned in this elective to discuss sexual health topics in the clinical setting, and 73.8% reported increased interest in incorporating sexual health into their professional work.
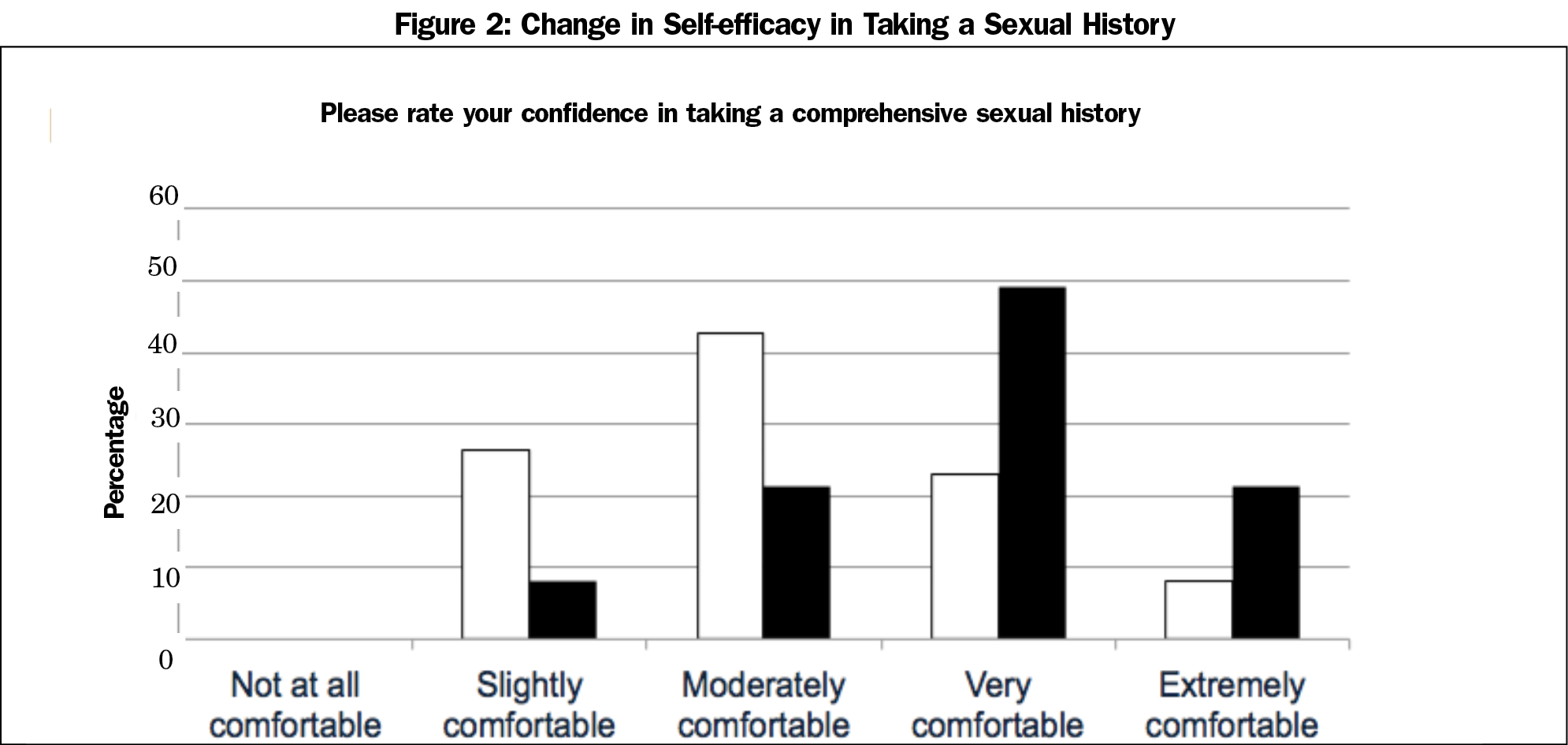
Medical students report improved self-efficacy in advanced interviewing skills after participating in the program. Notably, the mean self-efficacy for taking a comprehensive sexual history was 3.13 (“somewhat comfortable”) before program participation vs 3.84 (“very comfortable”) after program participation, with 54.1% of respondents reporting improvement (Figure 2). This improvement in critical interviewing skills in every category suggests that medical students gain meaningful skills through teaching Sex Ed by Brown Med.
Participants also reported increased self-efficacy in discussing all 12 sexual health topics. The largest proportion of students reported improvement in discussing sexual orientation/gender identity and sexually transmitted infections (73.8% and 70.5%, respectively.) The former topic in particular does not get significant coverage in US medical school curricula.25 While we also found that LGBTQ-identifying respondents report a greater increase in self-efficacy in discussing sexual health topics than non-LGBTQ identifying participants, further research should analyze potential reasons for this difference.
This study has several limitations. Time between participation in the elective and survey response ranged from 6 months to 4 years, therefore respondent memory of their confidence prior to participating in Sex Ed by Brown Med may be a limitation. Selection bias may have affected results because participants in the elective and in the study were self-selecting groups. Students who chose to participate in the elective may have been more motivated to gain comfort in discussing sexual health topics than the typical medical student. Response bias may have affected results: former teachers with a more favorable experience in the program may have been more likely to respond to the survey and to indicate greater growth in comfort and skills. This type of research is complicated by individual interpretation of terms such as “healthy relationships.” We operationalized these terms by defining them during in prelesson training sessions and lesson plans. Confounding variables may have included other clinical experiences during this time or the effect of progression through medical training. To address this, for the next phase of research, we will survey program participants and a control group of nonparticipating medical students.
Our program increases future clinicians’ comfort and confidence in discussing sexual health topics with adolescents and patients of all ages, while increasing adolescents’ knowledge of sexual health topics. Programs similar to Sex Ed by Brown Med may be useful to improve medical students’ ability to adequately care for their patients’ sexual health while providing evidence-based comprehensive sexual health education to adolescents. Schools interested in implementing a similar program should contact the corresponding author.
Acknowledgments
Financial support: This work was supported by Petersen Educational Enrichment Fund, Alpert Medical School Student Senate Funding Board, and Alpert Medical School Office of Medical Education.
Presentations: The content of this manuscript was presented at the 2018 American Medical Association Accelerating Change in Medical Education Spring Consortium Meeting at The Warren Alpert Medical School at Brown University in Providence, Rhode Island on April 9, 2018.
References
- Final Update Summary: Sexually Transmitted Infections: Behavioral Counseling. U.S. Preventative Services Task Force. September 2016. www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/sexually-transmitted-infections-behavioral-counseling1. Accessed May 11, 2018.
- American Academy of Pediatrics. American Academy of Pediatrics: Committee on Psychosocial Aspects of Child and Family Health and Committee on Adolescence. Sexuality education for children and adolescents. Pediatrics. 2001;108(2):498-502.
- Sadovsky R, Nusbaum M. Sexual health inquiry and support is a primary care priority. J Sex Med. 2006;3(1):3-11. https://doi.org/10.1111/j.1743-6109.2005.00193.x
- Bayer CR, Satcher D. Moving Medical Education and Sexuality Education Forward. Curr Sex Health Rep. 2015;7(3):133-139. https://doi.org/10.1007/s11930-015-0050-1
- Donaldson AA, Lindberg LD, Ellen JM, Marcell AV. Receipt of sexual health information from parents, teachers, and healthcare providers by sexually experienced U.S. adolescents. J Adolesc Health. 2013;53(2):235-240. https://doi.org/10.1016/j.jadohealth.2013.03.017
- Alexander SC, Fortenberry JD, Pollak KI, et al. Sexuality talk during adolescent health maintenance visits. JAMA Pediatr. 2014;168(2):163-169. https://doi.org/10.1001/jamapediatrics.2013.4338
- Boekeloo BO. Will you ask? Will they tell you? Are you ready to hear and respond?: barriers to physician-adolescent discussion about sexuality. JAMA Pediatr. 2014;168(2):111-113. https://doi.org/10.1001/jamapediatrics.2013.4605
- Henry-Reid LM, O’Connor KG, Klein JD, Cooper E, Flynn P, Futterman DC. Current pediatrician practices in identifying high-risk behaviors of adolescents. Pediatrics. 2010;125(4):e741-e747. https://doi.org/10.1542/peds.2009-0271
- Skelton JR, Matthews PM. Teaching sexual history taking to health care professionals in primary care. Med Educ. 2001;35(6):603-608. https://doi.org/10.1046/j.1365-2923.2001.00926.x
- Sack S, Drabant B, Perrin E. Communicating about sexuality: an initiative across the core clerkships. Acad Med. 2002;77(11):1159-1160. https://doi.org/10.1097/00001888-200211000-00025
- Shindel AW, Parish SJ. Sexuality education in North American medical schools: current status and future directions. J Sex Med. 2013;10(1):3-17. https://doi.org/10.1111/j.1743-6109.2012.02987.x
- Malhotra S, Khurshid A, Hendricks KA, Mann JR. Medical school sexual health curriculum and training in the United States. J Natl Med Assoc. 2008;100(9):1097-1106. https://doi.org/10.1016/S0027-9684(15)31452-8
- Coleman E, Elders J, Satcher D, et al. Summit on medical school education in sexual health: report of an expert consultation. J Sex Med. 2013;10(4):924-938. https://doi.org/10.1111/jsm.12142
- Benni E, Sacco S, Bianchi L, et al; SISM educators group. Evaluation outcomes of a sex education strategy in high schools of Pavia (Italy). Glob Health Promot Educ. 2016;23(2):15-29. https://doi.org/10.1177/1757975914558309
- Kuo K, Zhu TY, Raidoo S, Zhao LX, Sammarco A, Ashby K. Partnering with public schools: a resident-driven reproductive health education initiative. J Pediatr Adolesc Gynecol. 2014;27(1):20-24. https://doi.org/10.1016/j.jpag.2013.08.006
- Bretelle F, Shojai R, Brunet J, et al. Medical students as sexual health peer educators: who benefits more? BMC Med Educ. 2014;14(1):162. https://doi.org/10.1186/1472-6920-14-162
- Johnson K, Rullo J, Faubion S. Student-Initiated Sexual Health Selective as a Curricular Tool. Sex Med. 2015;3(2):118-127. https://doi.org/10.1002/sm2.57
- Faulder GS, Riley SC, Stone N, Glasier A. Teaching sex education improves medical students’ confidence in dealing with sexual health issues. Contraception. 2004;70(2):135-139. https://doi.org/10.1016/j.contraception.2004.03.010
- Duh E, Medina SP, Coppersmith N, Adjei N, Roberts MB, Magee S. Sex Ed by Brown Med: a student-run curriculum and its impact on sexual health knowledge. Fam Med. 2017;49(10):785–8.
- Stewart T, Wubbena Z. An overview of infusing service-learning in medical education. Int J Med Educ. 2014;5:147-156. https://doi.org/10.5116/ijme.53ae.c907
- Howard GS, Ralph KM, Gulanick NA, Maxwell SE, Nance DW, Gerber SK. Internal invalidity in pretest-posttest self-report evaluations and a re-evaluation of retrospective pretests. Appl Psychol Meas. 1979;3(1):1-23. https://doi.org/10.1177/014662167900300101
- Pratt CC, McGuigan WM, Katzev AR. Measuring program outcomes: using retrospective pretest methodology. Am J Eval. 2000;21(3):341-349. https://doi.org/10.1177/109821400002100305
- Skeff KM, Stratos GA, Bergen MR. Evaluation of a medical faculty development program: a comparison of traditional pre/post and retrospective pre/post self-assessment ratings. Eval Health Prof. 1992;15(3):350-366. https://doi.org/10.1177/016327879201500307
- Drennan J, Hyde A. Controlling response shift bias: the use of the retrospective pre‐test design in the evaluation of a master’s programme. Assess Eval High Educ. 2008;33(6):699-709. https://doi.org/10.1080/02602930701773026
- Rubin ES, Rullo J, Tsai P, et al. Best practices in North American pre-clinical medical education in sexual history taking: consensus from the summits in medical education in sexual health. J Sex Med. 2018;15(10):1414-1425. https://doi.org/10.1016/j.jsxm.2018.08.008
Lead Author
Sarah J. F. Bourne, BA
Affiliations: The Warren Alpert Medical School of Brown University, Providence, RI
Co-Authors
Charlotte M. Lee, BA - The Warren Alpert Medical School of Brown University, Providence, RI
Elizabeth Taliaferro, BA - The Warren Alpert Medical School of Brown University, Providence, RI
Angela Y. Zhang, BA - The Warren Alpert Medical School of Brown University, Providence, RI
Natasha F. Dalomba, BA - The Warren Alpert Medical School of Brown University, Providence, RI
Constance Panton, BA - The Warren Alpert Medical School of Brown University, Providence, RI
Mary B. Roberts, MS - Care New England Medical Group/Primary Care & Specialty Services, Pawtucket, RI
Susanna Magee, MD, MPH - The Warren Alpert Medical School of Brown University, Providence, RI
Corresponding Author
Sarah J. F. Bourne, BA
Correspondence: Sarah Bourne, Brown University, Box G-9999, Providence, RI 02912. 717-773-6487
Email: sarah_bourne@brown.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.