Background and Objectives: There has been a growth in the demand for convenient, walk-in access in health care across the United States, resulting in primary care practices seeing a shift in services to urgent care centers (UCCs). In order to incorporate the flexibility of a UCC and improve primary care access and preventive care for our regular patients, the University of North Carolina (UNC) Family Medicine Center (FMC) established a UCC within the practice. This report describes that process and the impact of the new UCC on our academic practice.
Methods: With the support of the UNC health care system, our primary objectives were to provide enhanced access for patients with acute problems, decrease emergency department (ED) utilization, and increase enrollment of new patients for ongoing primary care. As part of our intervention, we asked providers to respond to a series of questions at the end of each visit. These questions, along with data regarding number of visits and revenue, were tracked longitudinally.
Results: By the end of our first year, we were treating about 900 patients per month, of which approximately one-third would have otherwise visited the ED. We averaged 115 new patients establishing care per quarter. In addition to the success of this new service line, our primary practice maintained provider continuity and grew at a higher rate than prior to opening the UCC.
Conclusions: The opening of urgent care at the UNC FMC provided improved access for our patients, increased the number of patients empaneled in our primary care practice, and provided a new revenue stream.
Long wait times, inflexible hours, and scheduling difficulties in primary care practices lead many patients to seek nonemergency care in emergency departments (EDs).1 An estimated 13%-27% of ED visits could be handled by other facilities, saving $4.4 billion per year.1 This demand for convenient, cost-effective care has led to the rise of urgent care centers (UCCs) as evidenced by 1,725% growth in UCC visits from 2007-2016.2,3 In November 2018, the number of UCCs reached 8,774, an increase of 8% from 2017,4 comprising a nearly $18 billion industry.5
Despite the convenience of UCCs, they lack the continuity and comprehensiveness provided by primary care practices.6 This report describes the development and 1-year outcomes of a UCC at the Family Medicine Center (FMC) of the University of North Carolina at Chapel Hill (UNC)–a Patient-Centered Medical Home (PCMH) site. Our goals were to provide after-hours care to patients and to introduce new patients to our continuity practice, while decreasing ED utilization. We hoped to manage both acute issues and chronic diseases.
Description of the Intervention
The UNC FMC is a large, resident-training clinic located approximately one mile from UNC Hospitals. The clinic serves approximately 19,000 patients. Before opening the UCC in February 2018, the clinic operated from 7 am to 7 pm on Monday, Tuesday, and Thursday, 9:30 am to 7 pm on Wednesday, 8 am to 5 pm on Friday, and 8 am to 12 pm on Saturday. By adding a UCC to the practice, the hours expanded to 7 am to 9 pm on Monday-Friday, 8 am to 5 pm on Saturday, and 12 pm to 5 pm on Sunday. We collaborated with our partners in the health care system to increase our inventory of supplies and medications accordingly (See Appendix 1).
Our weekday UCC staffing included one physician, one medical assistant (MA), and one licensed practical nurse (LPN) or registered nurse (RN) from 7 am to 8 am and 5 pm to 9 pm. From 8 am to 5 pm on weekdays, two providers, two MAs, and one LPN/RN staffed the UCC. Weekends were staffed with two providers, two MAs, and one LPN/RN. We also worked with our laboratory and radiology partners to ensure access to their services (including on-site access for lab draws and plain film radiology). This staffing was in addition to our required staffing for the continuity clinic.
Evaluation Methods
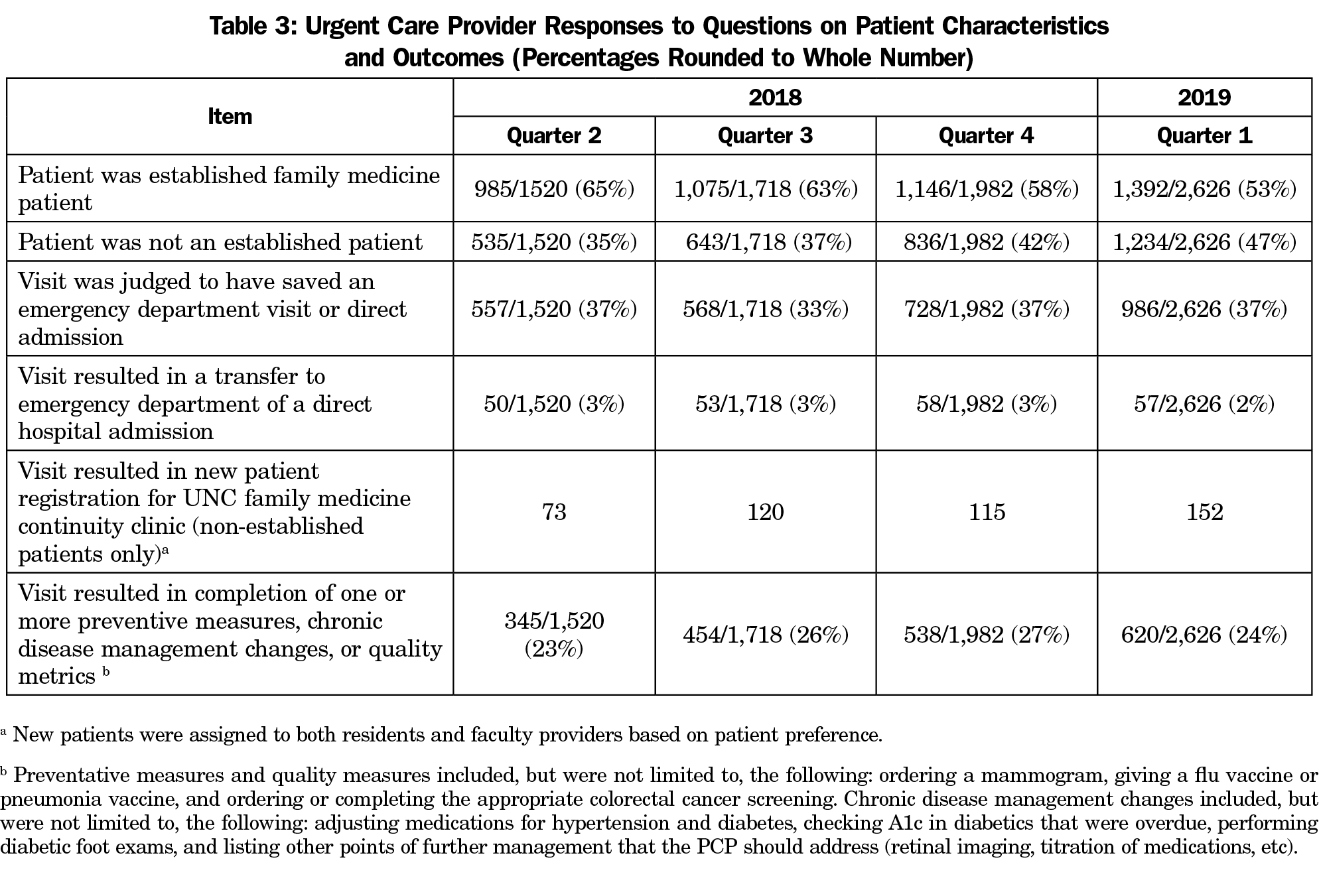
We defined measurements that reflected quality, access to care, prevention of unnecessary ED utilization, and enrollment of new patients who did not have a primary care physician (PCP). We added questions into an electronic medical record (EMR) note template that required a manual response from the provider via a selection menu. We asked providers to document responses to these questions at the end of each encounter (Table 3). In addition, patient volumes, continuity data in the FMC, and financial data were extracted from existing systems. The UNC Institutional Review Board exempted this process.
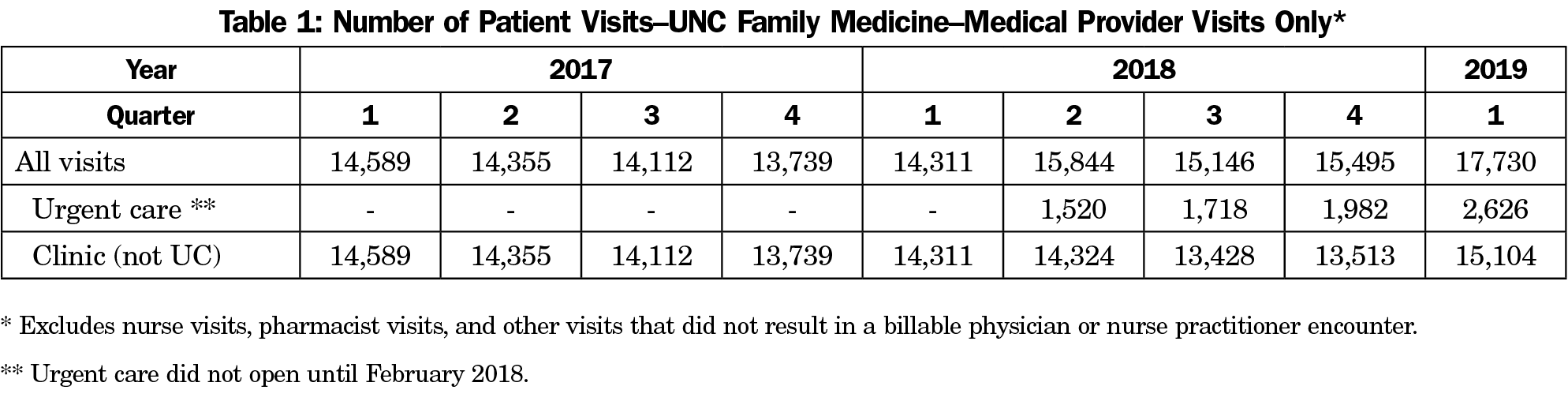
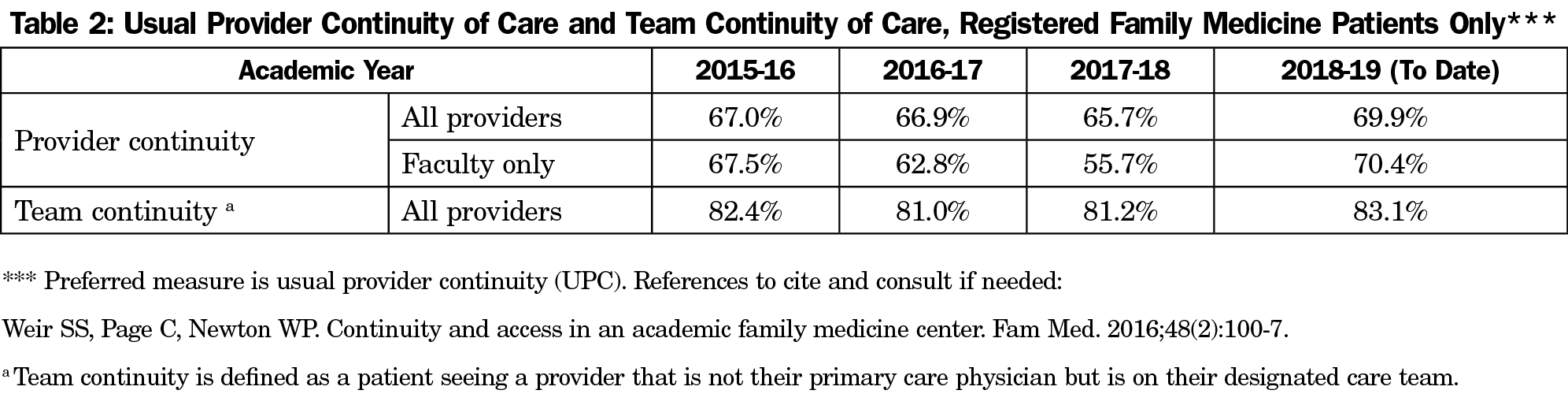
Patient growth was gradual at first and continued to rise, with volume stabilizing around 900 patients/month (Table 1). The growth in the UCC did not negatively impact patient volumes and continuity rates in our clinical practice, with 2018-2019 showing the highest rate of continuity over the last 4 years (Table 2).
Cumulative data from provider notes indicated that over 33% of UCC patient encounters may have prevented an ED visit. This response was based on the provider’s judgement and/or the patient voicing they would have gone to the ED when asked. Of all visits, fewer than 3% resulted in a direct admission to a hospital or transfer to the ED. Furthermore, 25% of patients seen (regardless of PCP) had preventive or chronic disease management needs addressed, and an average of 115 new patients (largely patients who were not considering our practice prior to coming to the UCC for primary care) per quarter established care after coming to the UCC (Table 3).
Financially, we tracked revenue and costs on a quarterly basis. Including all initial staffing and supply costs, we project a break-even point after 3 years. If quarterly balances are computed without carryover of upfront costs, our UCC was profitable by the fifth quarter of operations.
By opening a UCC, we saw more people enter primary care, provided a comprehensive approach to UCCs, reduced unnecessary ED visits, and provided our practice with a new revenue stream. Reducing ED burden was a primary motivation for our initial institutional financial support, and our data on prevented ED visits is testimony to the program’s success. Prior studies have shown that UCC visits cost around $200 to $400 less than the same care at an ED.7,8 We project that our UCC saved the health care system between $568,000 and $1,136,000 based on the estimated savings of $200 to $400 saved per ED visit avoided.
Our UCC provided improved access to the comprehensive care provided at a PCMH. Through a provider questionnaire that was integrated into each visit note, we were able to track quality and utilization metrics. Furthermore, access to the entire EMR and a comprehensive, primary care approach toward the UCC process allowed us to close preventive care or chronic disease quality gaps on a quarter of patient visits.
Initiating the UCC posed both financial and personnel challenges. Since the health care system was a partner, we worked on developing an extended hour schedule that would allow us to be open during the peak hours of ED demand to help offload our emergency room. Extended hours posed scheduling challenges due to an increase in staffing demand that we overcame through moonlighting pay and overtime. The financial support of our health care system allowed us to achieve profitability in less than 18 months; however, the lack of such support would likely lead to more time needed to achieve profitability for others trying to replicate our design.
Another potential challenge that we were well poised for was limitations in space. Fortunately, we recently remodeled our clinic for efficient space utilization, increasing our exam rooms by a third on the same footprint. This allowed us to open the UCC without new construction.
We acknowledge some limitations to our data. Provider response rates to our questions waned on busy days, leaving our data incomplete and constituting a potential source of error. We also did not track patients after their UCC visit to see if they presented to an ED. At times, we were unable to staff an LPN/RN and required providers to start IVs and administer medications. Lab and imaging staffing were absent on limited occasions. Likewise, we did not collect any patient satisfaction data.
In summary, we have seen a large increase in patient visits in our practice through the incorporation of a UCC. While acute problems are the focus of urgent care, we found that a significant amount of visits could also address chronic or preventative care. In addition to providing expanded service, we added value to the health care system by decreasing unnecessary ED visits and attracting new patients into primary care.
Acknowledgments
The authors acknowledge Addison Newman for his assistance with the graphical information and the data tables, and Dr Philip Sloane for assistance in manuscript development and editing.
References
- Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood). 2010;29(9):1630-1636. https://doi.org/10.1377/hlthaff.2009.0748
- Weinick R, Betancourt R. No appointment needed: the resurgence of urgent care centers in the United States. Oakland, CA: California Healthcare Foundation; 2007.
- Cummins J. Uurgent Care Volume Growth Easily Outstrips ERS. HealthLeaders. March 21, 2018. https://www.healthleadersmedia.com/finance/urgent-care-volume-growth-easily-outstrips-ers. Accessed June 29, 2019.
- Sanborn B. Urgent care centers grow in number, reach thanks to comprehensive capabilities, convenience, demand. Healthcare Finance. March 12, 2019. https://www.healthcarefinancenews.com/news/urgent-care-centers-grow-number-reach-thanks-comprehensive-capabilities-convenience-millennial. Accessed June 29, 2019.
- Japsen B. Urgent Care Industry Hits $18 Billion As Big Players Drive Growth. Forbes. February 23, l2018. https://www.forbes.com/sites/brucejapsen/2018/02/23/urgent-care-industry-hits-18b-as-big-players-drive-growth/#6dc9ef154d89. Accessed June 29, 2019.
- McGough PM, Norris TE, Scott JD, Burner TG. Meeting the demands of the Affordable Care Act: improving access to primary care. Popul Health Manag. 2017;20(2):87-89. https://doi.org/10.1089/pop.2016.0030
- Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151(5):321-328. https://doi.org/10.7326/0003-4819-151-5-200909010-00006
- Thygeson M, Van Vorst KA, Maciosek MV, Solberg L. Use and costs of care in retail clinics versus traditional care sites. Health Aff (Millwood). 2008;27(5):1283-1292. https://doi.org/10.1377/hlthaff.27.5.1283
- Manley M. Should your primary care practice expand into urgent care? Medical Economics. November 25, 2013. https://www.medicaleconomics.com/practice-expansion/should-your-primary-care-practice-expand-urgent-care. Accessed June 29,2019.



There are no comments for this article.