Background and Objectives: At a time when the US health care system needs greater access to comprehensive, on-demand primary care, the University of North Carolina Family Medicine Center found itself struggling to meet patient demands within the confines of an outdated facility. Clinic leadership sought to redesign the physical space to expand capacity, integrate other members of the care team, support extended hours of operation, and improve patient experience.
Methods: Clinic leadership employed experienced lean coaches to train our entire department in lean methodology, to implement a comprehensive approach to redesigning our workflows, and to use those perfected workflows to redesign and renovate our new clinical workspace.
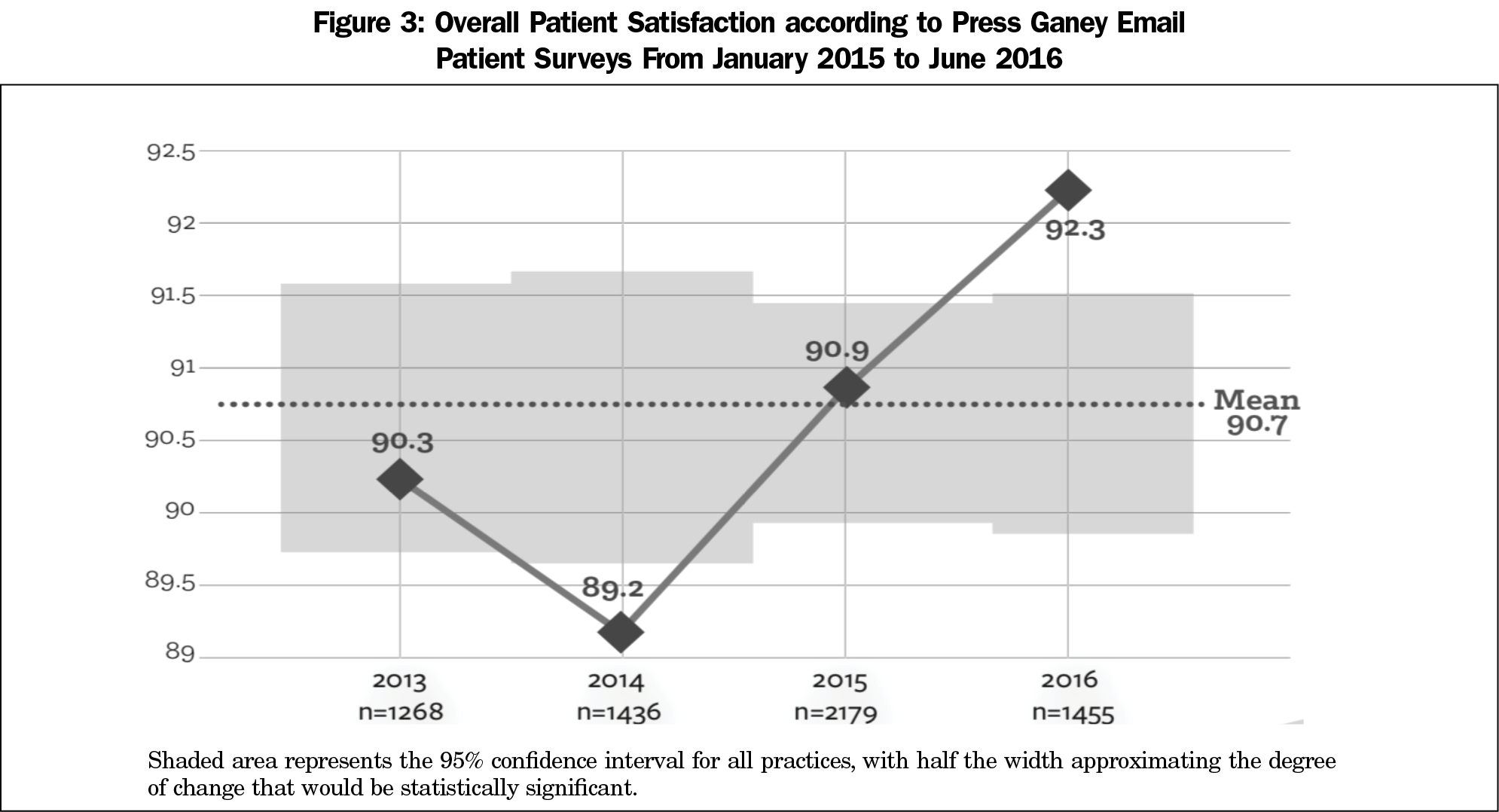
Results: Upon completion of the renovation and redesign, the clinic experienced significant growth in patient volumes (24%) and unprecedented improvement in patient satisfaction (89th to 92nd percentile).
Conclusions: Lean methodology proved to be an effective strategy for analyzing our current workflows and use of physical space. Moreover, lean strategies proved vital for redesigning and renovating our clinic.
The ambitious challenge of a patient-centered medical home,1,2 and even more so value-based payment models, require clinics that efficiently deliver broad ranging services on an as-needed basis.3 As family medicine evolves to meet increased demands, the impact of physical workspace is often overlooked. Unfortunately, traditional office design impedes the effectiveness of primary care teams in multiple ways.4
Built in 1990, the University of North Carolina (UNC) Family Medicine Center was once a state-of-the-art facility. By 2011, faculty and staff realized they were making the most of an outdated facility. Decreased patient satisfaction, increased wait times, and poor staff/provider experience scores all indicated a need for improvement. Simultaneously, demand for services increased. That year, the clinic reached a record number of 52,000 patient visits in a building that was designed for maximum capacity of 35,000. Departmental leadership sought an innovative, patient-centered solution to expand the clinical capacity and enhance patients’ overall experience.
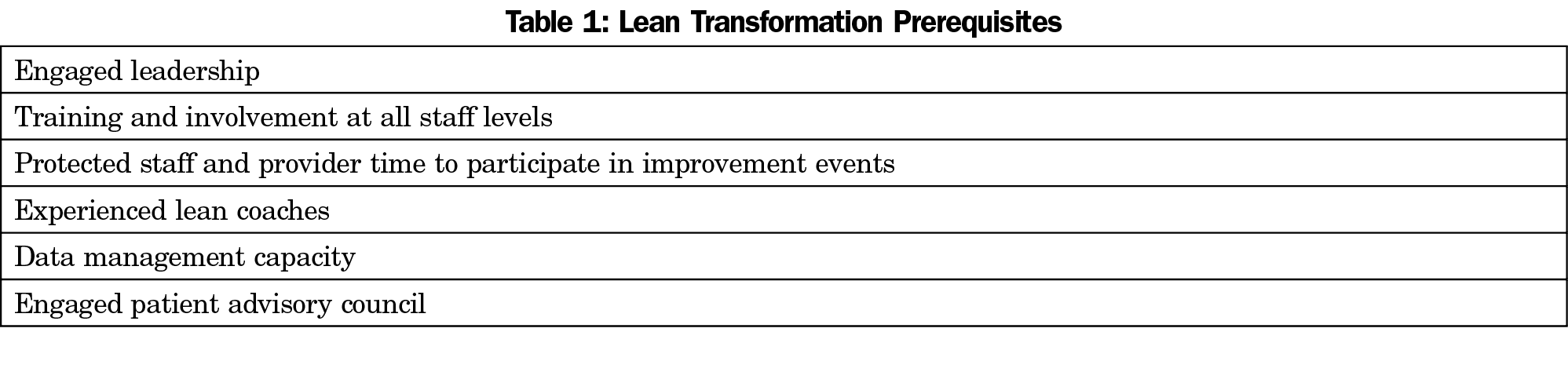
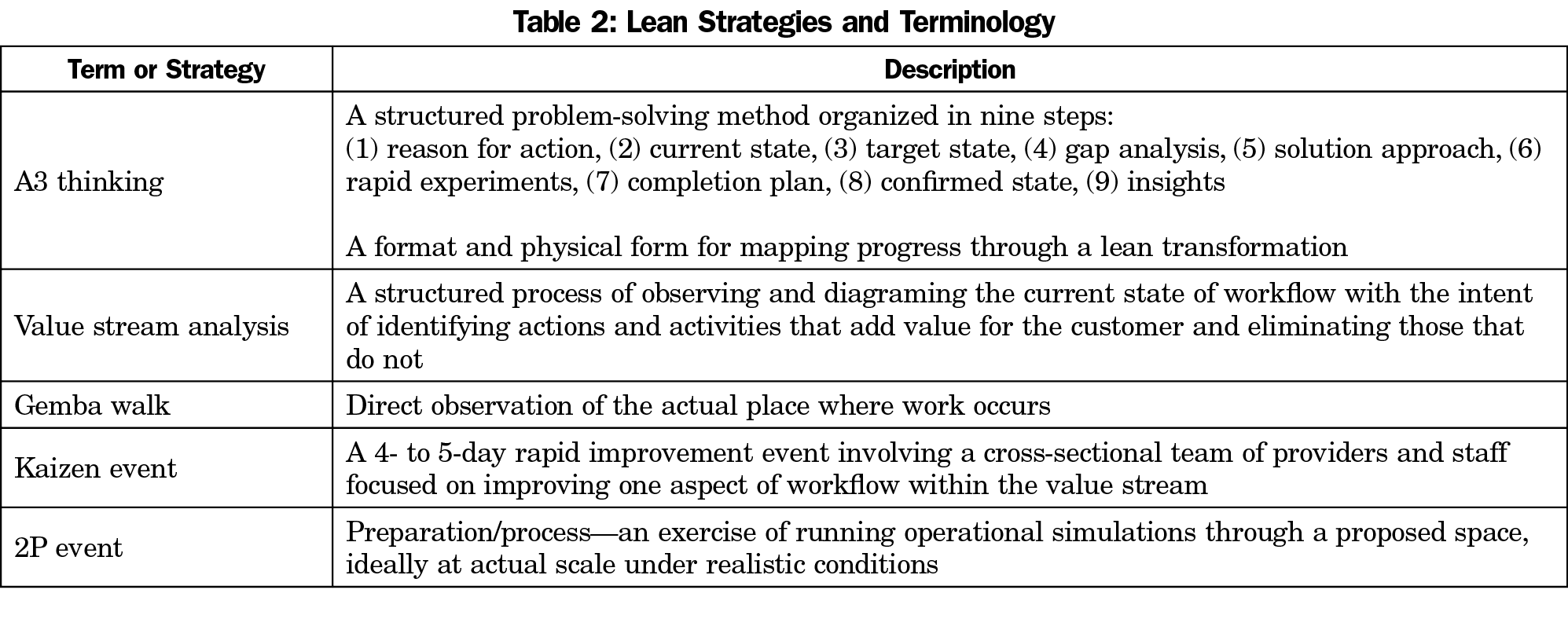
Clinic leadership partnered with the Office of Operational Efficiency (OE) to use lean methodology in renovation and redesign efforts.5 Lean methodology originates from Toyota manufacturing. It emphasizes value to the customer through continuous improvement and respect for all members of the team. Thus, all members of the clinical operation are trained and encouraged to continually identify areas of waste and eliminate steps that do not add value to the patient. Long before any construction work, lean coaches trained clinic leadership, faculty, staff, and members of the patient advisory council to ensure buy-in and a working understanding of lean principles at all organizational levels (Table 1). Once the clinic had embraced lean thinking, clinic leadership assembled a multidisciplinary team of providers, staff, patients, architects, and quality improvement coaches to renovate and redesign our clinical space and workflows using multiple lean methodologies (Table 2).
The team observed our current state and several key findings emerged. Patients spent too much time waiting at various steps in their visit (eg, in line to check in). Providers spent too much time outside of the exam room (eg, looking for supplies). Patients had to walk through the building too much to access services (eg, lab). Patients had little sense of privacy during the check-in and check-out processes.
The team then envisioned and mapped the care we aspired to provide. Using lean principles, we examined the gaps between our current and future state. We then identified metrics that would measure progress toward our ideal state. To evaluate changes in patient care capacity, we identified total number of patient visits, total patient cycle time, and the amount and proportion of space dedicated to actual patient care as our main outcomes of interest. To evaluate patient experience, we chose Press Ganey patient satisfaction surveys as our key indicator of success.
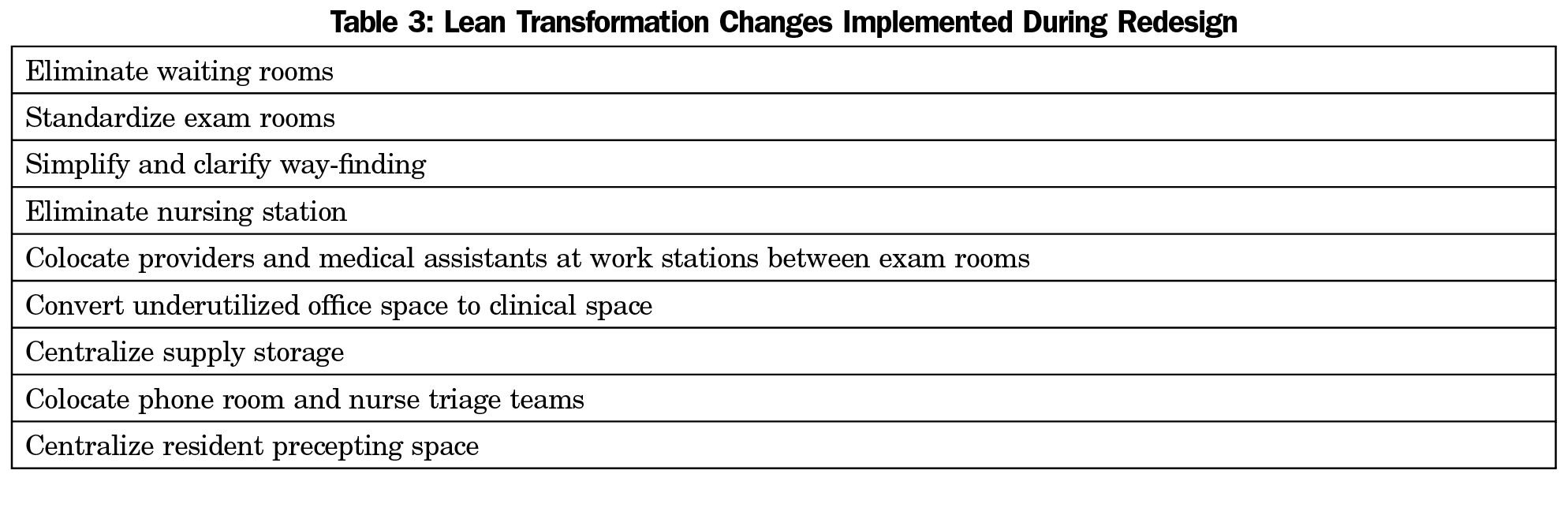
Through the lean redesign process, new patient flow was mapped out and endorsed by faculty, staff, and patients, and subsequently the team worked with architects to design a physical space to support their vision. The team completely redesigned the patient experience, eliminating waste and streamlining patient movement through the visit (Table 3). This included bold changes like eliminating the check-in desk in exchange for a process wherein every patient was briefly greeted at the front door and then taken to their exam room for check-in. To minimize loss of patient care capacity during renovation, we converted a former waiting area into examining rooms first, and then remodeled one module of four at a time.
The UNC Institutional Review Board approved this study as exempt from formal review (#19-1651).
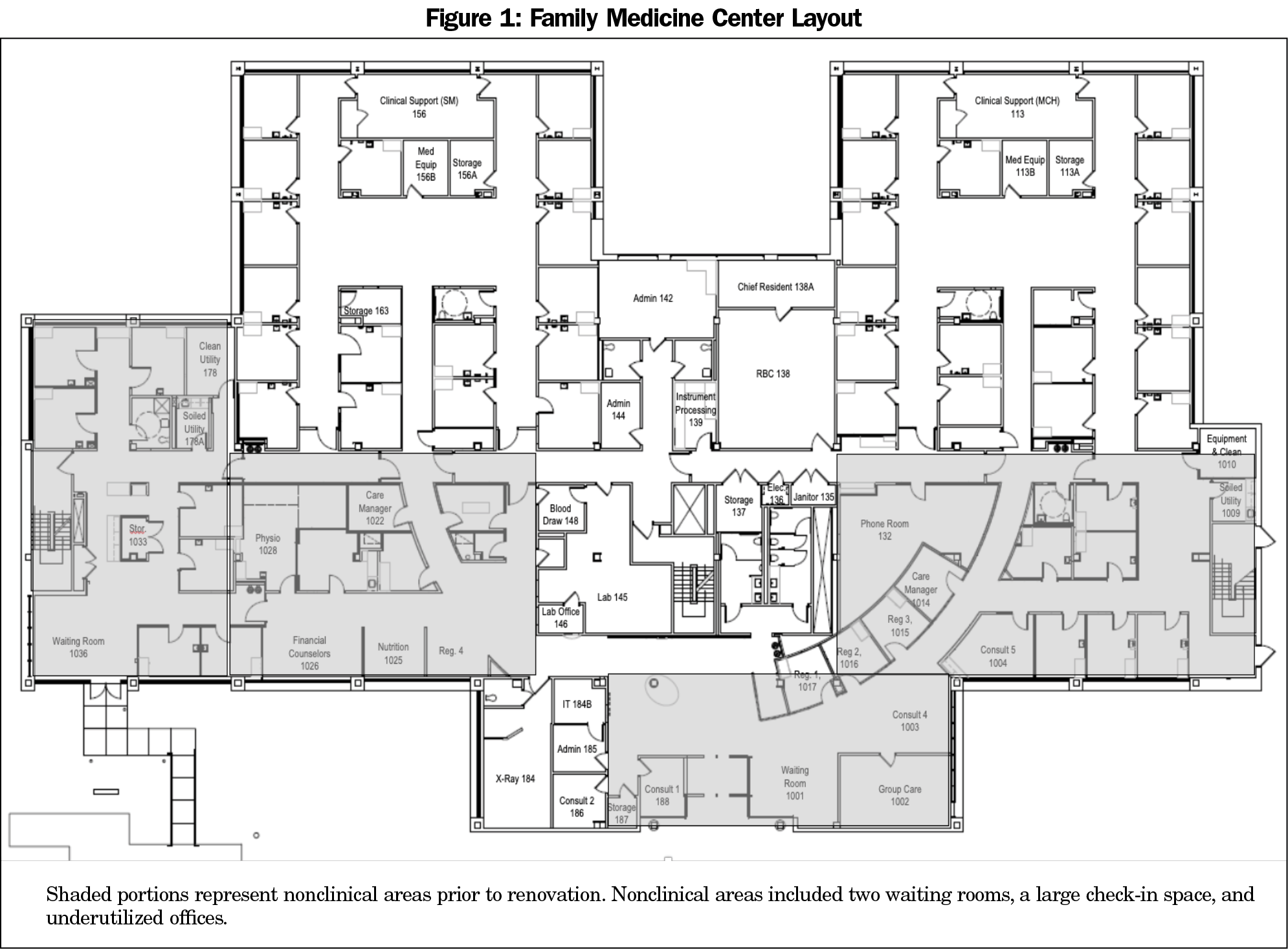
At the conclusion of this roughly $3 million project, the UNC Family Medicine Center accomplished several outcomes. First, the amount of space dedicated to clinical care increased by 31%, from 14 to 18.4 exam rooms per 10,000 square feet with a net increase from 35 to 46 rooms dedicated to clinical care, plus rooms dedicated to nutrition, physical therapy, behavioral health, and group visits (Figure 1). Increased clinical space and streamlined workflow allowed an increase from a prerenovation maximum of roughly 384 to a postrenovation capacity for over 480 patients per day.
We achieved this increase in space and efficiency without sacrificing patient visits during renovation. Careful staging of the renovation allowed us to increase patient visits by 10% during the construction time frame.
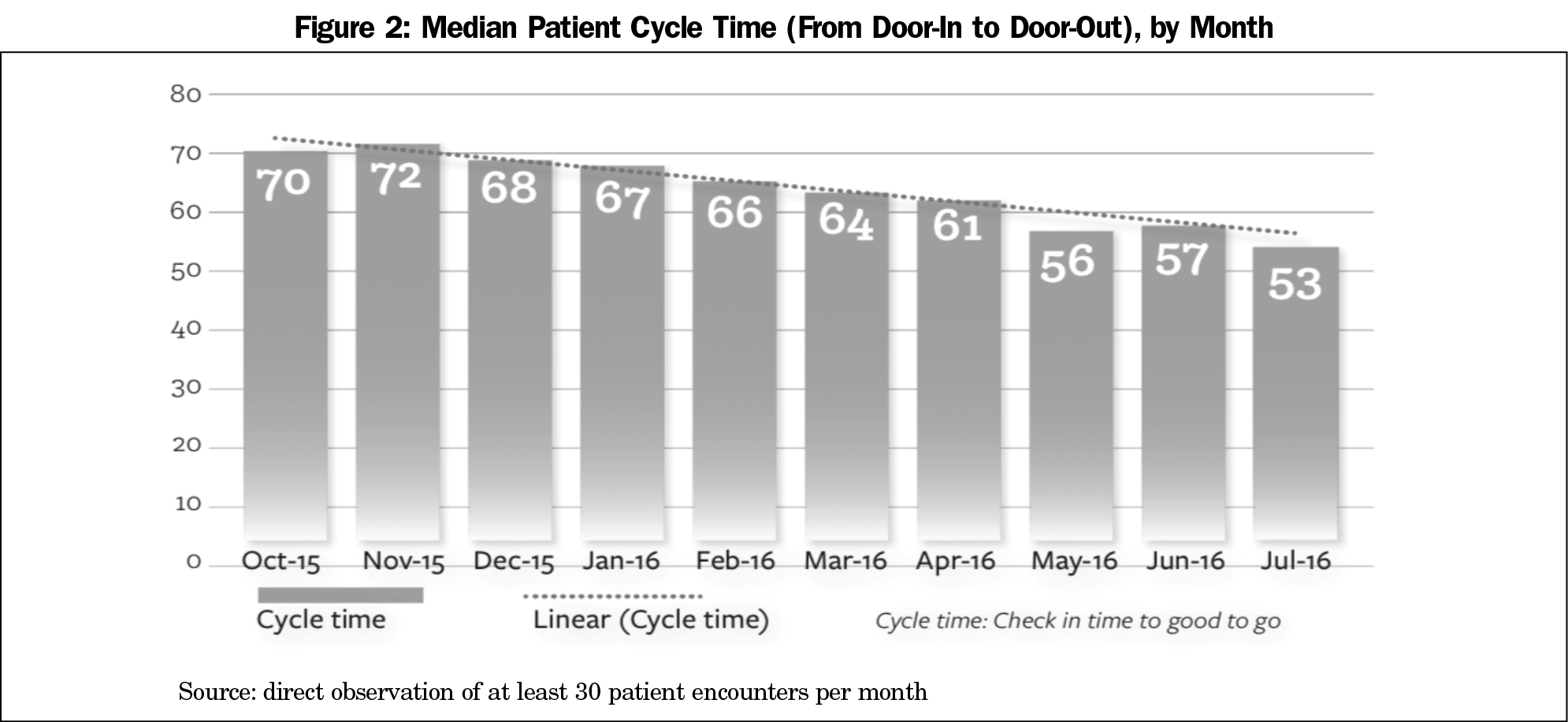
Once the renovation was complete, total patient cycle time improved from an average of 74 minutes per visit to a low of 53 minutes (Figure 2). Additionally, repurposed nonclinical space allowed for the eventual implementation of a dedicated urgent care space, drastically improving on-demand access to our patients and the community and further increasing capacity.
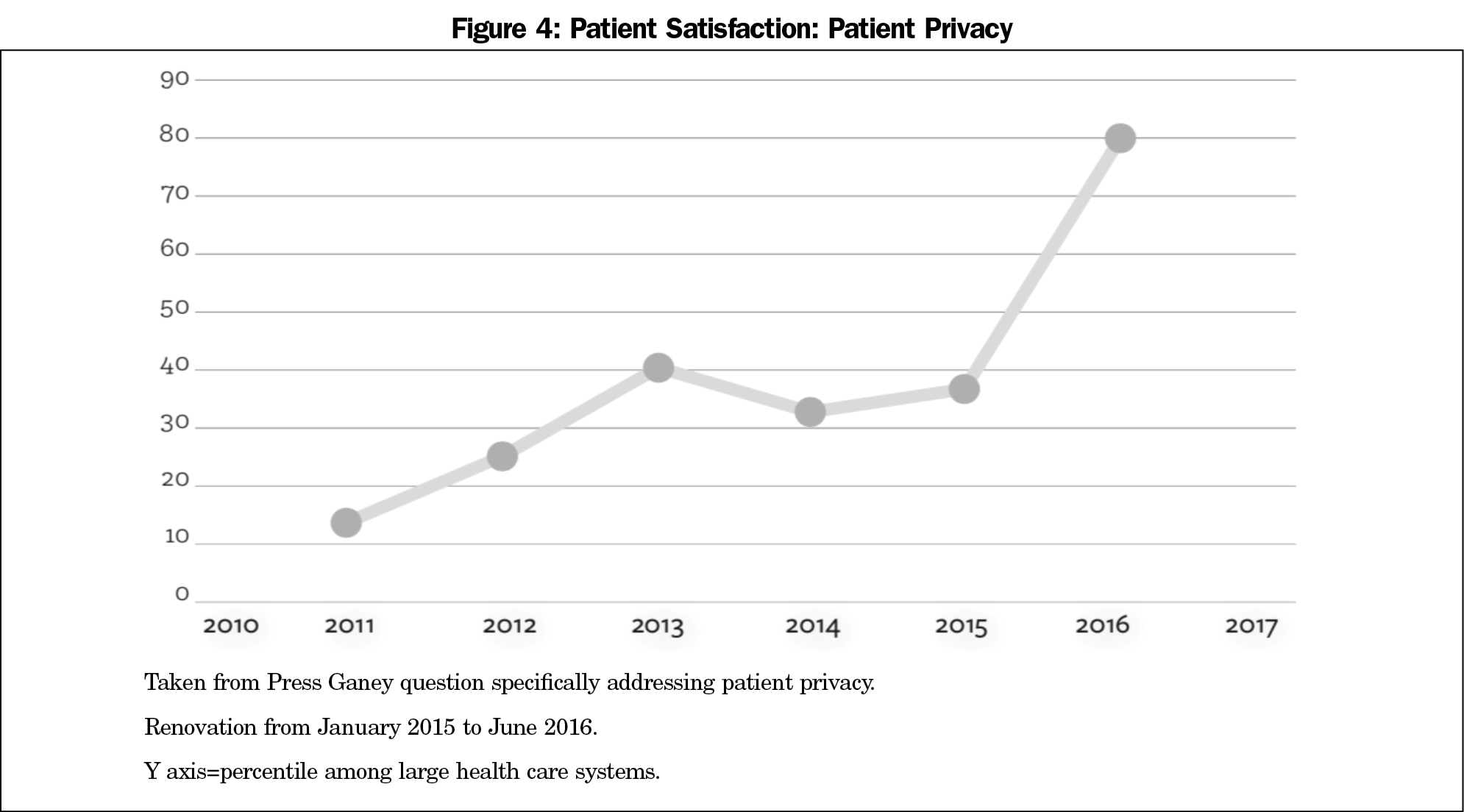
Overall patient satisfaction improved from 89.2 in 2014 to 93.7 in 2017 (Figure 3) and our patients’ sense of privacy improved from the 30th percentile among large health care systems to the 81st percentile (Figure 4).
Our experience indicates lean methodology is an effective tool for redesigning patient flow and planning clinical space. The processes we implemented allowed us to envision and create new clinical space that was more efficient, private, and satisfying for our patients. We were also able to successfully integrate additional members of the health care team into our workflow.
As more clinics embrace the principles of a patient-centered medical home or transition to value-based models, lean processes could be used to redesign existing clinical space and design more comprehensive indirect care.
We benefitted from a highly motivated, talented leadership team with significant experience and buy-in regarding lean methodology. They were able to quickly pick up new lean principles and communicate earnestly about their value with colleagues. In addition, UNC HealthCare has a large team of expert lean coaches. Our project was supported by a health care system that highly values the contribution of primary care, and to them, the return on investment was clear. These factors may have contributed to a more successful than usual lean transformation of our workflow and space.
In conclusion, the application of lean principles led to a successful transformation of our clinic. Patient satisfaction and sense of privacy increased. Total cycle time decreased. Multiple clinical quality metrics increased. The number of patients seen also increased. Future endeavors of this kind should carefully consider the multiple lean processes we implemented to identify the most effective steps among the many we employed.
References
- Epstein, AJ. The role of public clinics in preventable hospitalizations among vulnerable populations. Health Serv Res. 2001; 36:405-420.
- Yarnall KS, Østbye T, Krause KM, Pollak KI, Gradison M, Michener JL. Family physicians as team leaders: time to share the care. Prevention of Chronic Disease. 2009; 6(2): A59.
- Enthoven, AC, Crosson, FJ, Shortell SM. Redefining health care: medical homes or archipelagos to navigate? Health Aff (Millwood). 2007; 26:1366-1372. https://doi.org/10.1377/hlthaff.26.5.1366
- McGough P, Jaffy M, Norris T, Sheffield P, Shumway M. Redesigning your workspace to support team-based care. Fam Pract Manag. 2013; 20(2):20-24.
- Lawal AK, Rotter T, Kinsman L, et al. Lean management in health care: definition, concepts, methodology and effects reported (systematic review protocol). Syst Rev. 2014;3(1):103. https://doi.org/10.1186/2046-4053-3-103



There are no comments for this article.