Background and Objectives: Musculoskeletal problems are common in primary care, yet many family physicians lack confidence and competence in this area. The Advanced Primary Care Orthopedics (APCO) course utilizes hands-on physical exam instruction, interactive cases, and intentional repetition to teach anatomy, a standardized exam, and important diagnoses. This study assesses the effectiveness of APCO in improving musculoskeletal exam knowledge and confidence.
Methods: APCO is a 1.5-day course taught annually to family medicine residents. A 1-day course has also been conducted as a preconference workshop targeting faculty physicians. Participants completed pre- and postcourse assessments to evaluate their knowledge and confidence with the musculoskeletal exam. We compared results using mean differences with paired t-test statistics.
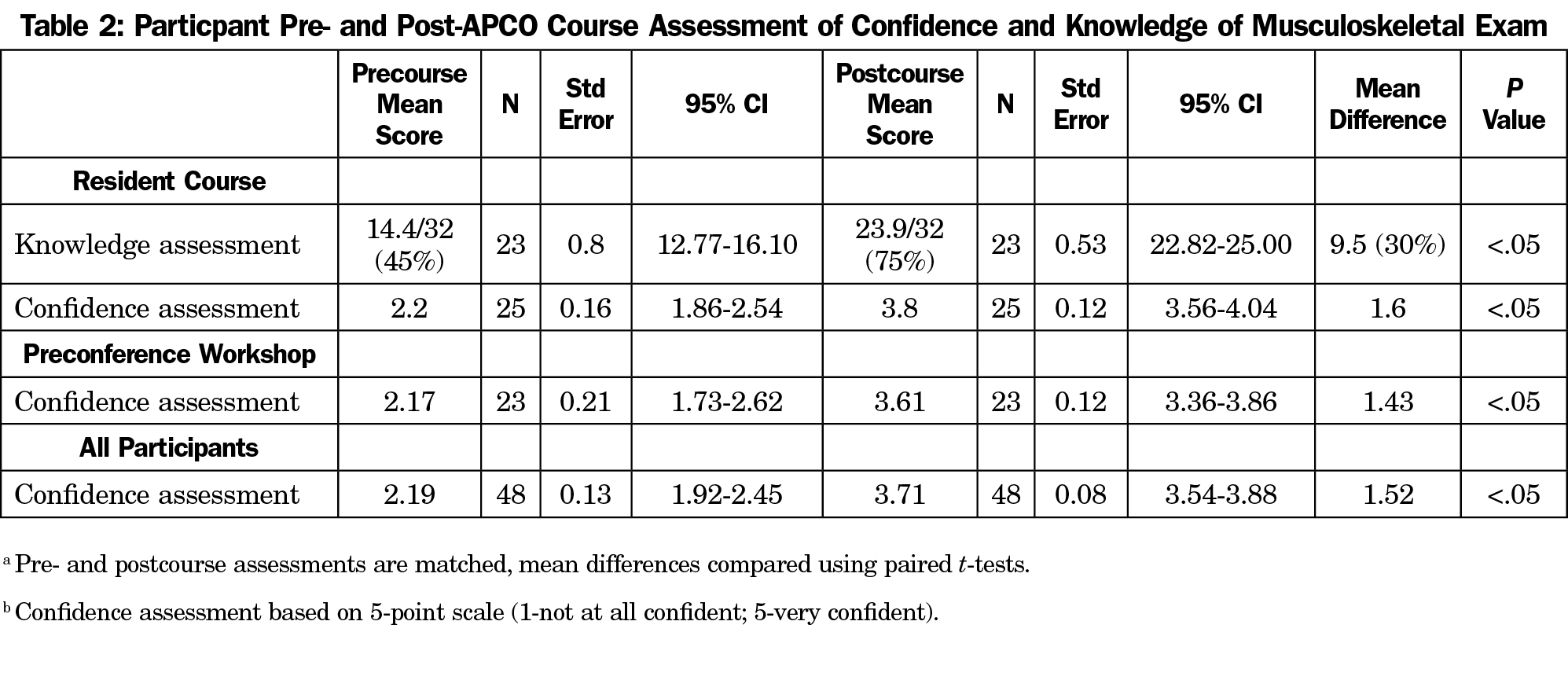
Results: In the 2018 and 2019 resident courses, 23 of 30 participants (77%) completed the knowledge assessment and 25 of 30 participants (83%) completed the confidence assessment. Knowledge assessment scores improved by 9.5 points (P<.05) after completion of the course. Confidence in the musculoskeletal exam, as assessed on a 5-point Likert scale (1–not confident at all; 5–very confident), improved from 2.2 to 3.8 after the course (P<.05). In the 2018 preconference workshop, 23 of 36 participants (64%) completed the confidence assessment. Confidence increased from 2.17 to 3.61 (P<.05) after course completion.
Conclusions: Participation in the APCO course increased short-term musculoskeletal knowledge and confidence. APCO has many potential applications for residency curricula, faculty development, and continuing medical education.
Musculoskeletal (MSK) problems account for 10%-20% of primary care visits,1,2 and 124 million American adults reported a MSK condition in 2015.3 However, studies have shown that family medicine (FM) residents and attendings lack MSK knowledge and confidence.4-6 This may be due to divergent approaches to MSK problems and lack of faculty confidence in teaching the exam.7,8
Various attempts have been made to improve MSK training, and interactive small group sessions are more effective than didactic sessions.9 Both direct observation with feedback and multiday structured interventions improve exam competence and confidence compared to traditional teaching methods.10-12 A standardized approach taught in a concentrated session is effective in obstetrics (ALSO), newborn resuscitation (NRP),13 and life support (ACLS),14 but is uncommon outside of emergent care situations.
We developed Advanced Primary Care Orthopedics (APCO) as an innovative method of teaching the MSK exam in a concentrated session combining small group interactive learning and direct observation with the proven pedagogical principle of intentional repetition. In APCO, a standardized approach is taken for each joint exam and repeated using multiple modalities to maximize learner engagement and retention of material. We conducted this study to assess the effectiveness of APCO in improving MSK exam knowledge and confidence.
Curriculum
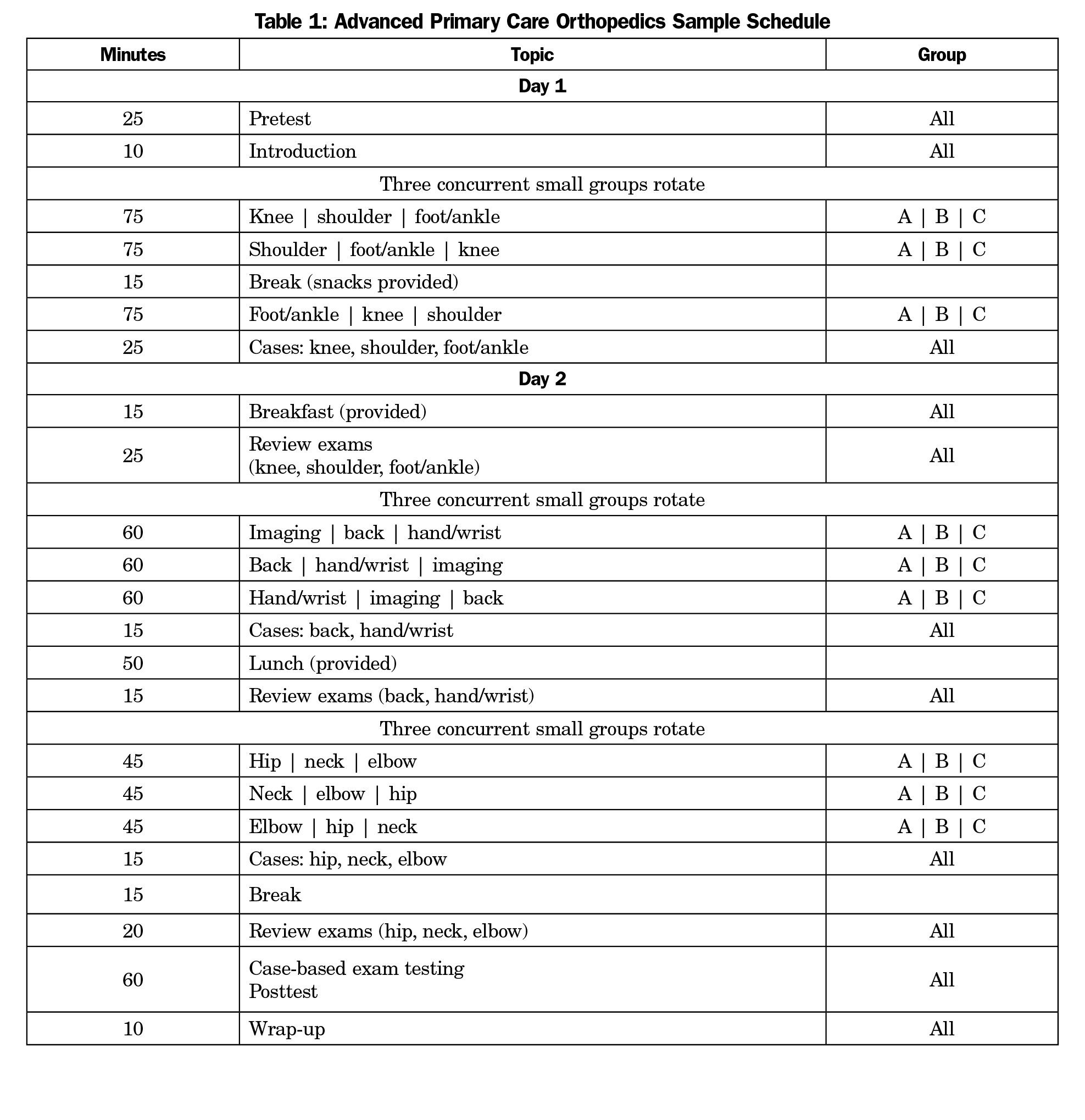
APCO has been taught annually as a 1.5-day course to residents at our urban community hospital-based FM residency program since 2012. Teaching faculty include four FM residency faculty with an interest in MSK education and one sports medicine physician. The course primarily consists of small group sessions that include a brief presentation, demonstration of a standardized physical exam with clinical correlations, and exam practice with direct observation and feedback (Table 1; course details: https://swedish-fh.squarespace.com/apco). Repetition occurs through cases, exam demonstrations, and assessment of participants’ physical examination skills using clinical cases. We did not cover treatment to limit the course length, and instead focus on establishing competency in physical exam and diagnostic skills. After internal work to refine APCO, two sports medicine fellowship-trained physician educators comprehensively reviewed course material in 2018. Further, an orthopedic surgeon has participated as course advisor and reviewed the material for accuracy. The 2018 and 2019 courses had a combined 30 participants (19 PGY1’s, 10 senior residents, 1 nurse practitioner). A 1-day version of APCO was conducted as a preconference workshop at the 2018 STFM Annual Spring Conference with 36 participants, primarily faculty physicians at FM residency programs. The workshop included all core exam skills and content areas, but excluded the elbow, imaging, the pre/posttest, exam review, and the case-based exam testing.
Evaluation
In the 2018 and 2019 resident courses, participant knowledge was assessed before and after the course through a written knowledge assessment comprised of 32 multiple-choice questions. Participants were asked one question to assess overall confidence in their MSK examination skills using a 5-point Likert scale (1–not confident at all; 5–very confident) before and after the course. Participants in the preconference workshop were asked to assess their confidence only. Our institutional review board reviewed our methodology and determined the project to be exempt.
Analysis
We compared pre- and postcourse knowledge and confidence assessment results using mean differences and paired t-test statistics using Stata.
In the 2018 resident course, 11 of 17 participants (65%) completed pre- and postcourse knowledge assessments and 12 of 17 participants (71%) completed pre- and postcourse assessments of MSK exam confidence. In the 2019 resident course, 12 of 13 participants (92%) completed the knowledge assessments and 13 of 13 participants completed the confidence assessments. In the 2018 preconference workshop, 23 of 36 participants (64%) completed pre- and postcourse confidence assessments.
After completion of the resident course, participant scoring on the knowledge exam improved by 9.5 points (95% CI: 7.85–11.11; a 30% increase) and confidence improved by a mean difference of 1.6 points (t[24]=13.86, P<.05) on a 5-point scale. Prior to APCO, 36% of participants reported a confidence score of 3 (somewhat confident) or higher with the MSK exam. This improved to 100% after APCO (Table 2).
In the preconference workshop, participant confidence in the MSK exam improved by a mean difference of 1.43 points (t(22)=10.38, P<.05) on a 5-point Likert scale. Prior to the course, 39% respondents reported a confidence score of 3 (somewhat confident) or higher with the MSK exam, which improved to 100% after APCO (Table 2).
APCO is a unique solution to improving MSK education that provides a standardized approach to the MSK physical exam and helps participants confidently diagnose their patients’ MSK conditions. Our approach builds on existing literature that demonstrates the value of mixed educational methods and small group learning,9-11 and is innovative in its condensed length, integration of multiple joint exams and intentional repetition of material.
This study demonstrates that APCO significantly improves resident knowledge and confidence with the MSK exam. Offering the course at the beginning of FM residency training establishes a standardized physical exam and helps early trainees gain confidence with their exam skills. Further, our experience suggests that APCO can also be applied to teach FM faculty and improves faculty confidence in their own exam skills.
There are several limitations to this study. Our sample size was small and included participants from only three courses run by a single program without an external comparison group. Further, only 70% of participants completed the assessments and there may have been differences between those who did and did not complete them. We assessed participant confidence and knowledge immediately after the APCO course, but did not assess long-term effects and whether improvements persist. We plan to repeat annual knowledge assessments as residents progress through training to better assess long-term knowledge retention. Finally, our study focused on a course that has been refined over several years prior to this assessment; it is difficult to extrapolate how our findings might apply at other locations when first implemented. Further efforts will focus on assessing knowledge and confidence over time and the benefits of utilizing the APCO model for faculty development.
Acknowledgments
Presentations: This study was presented as a workshop at both the Society of Teachers of Family Medicine 2017 Annual Spring Conference in San Diego, California, and at the Society of Teachers of Family Medicine 2018 Annual Spring Conference in Washington, DC.
References
- Rui P, Okeyode T. National Ambulatory Medical Care Survey: 2015 State and National Summary Tables. 2015. http://www.cdc.gov/nchs/ahcd/ahcd_products.htm. Accessed December 17, 2018.
- Garry J. Musculoskeletal medicine in the USA: education and training of family physicians. Qual Prim Care. 2003;11:159-162.
- Lezin N, Watkins-Castillo S. The Burden of Musculoskeletal Diseases in the United States: Prevalence. Rosemont, IL: Societal and Economic Cost; 2018.
- Amoako AO, Amoako AB, Pujalte GG. Family medicine residents' perceived level of comfort in treating common sports injuries across residency programs in the United States. Open Access J Sports Med. 2015;6:81-6..
- Lynch JR, Schmale GA, Schaad DC, Leopold SS. Important demographic variables impact the musculoskeletal knowledge and confidence of academic primary care physicians. J Bone Joint Surg Am. 2006;88(7):1589-1595. https://doi.org/10.2106/00004623-200607000-00021
- Matzkin E, Smith EL, Freccero D, Richardson AB. Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am. 2005;87(2):310-314. https://doi.org/10.2106/00004623-200502000-00011
- Walker DJ, Kay LJ. Musculoskeletal examination for medical students: the need to agree what we teach. Rheumatology (Oxford). 2002;41(11):1221-1223. https://doi.org/10.1093/rheumatology/41.11.1221
- Coady DA, Walker DJ, Kay LJ. Teaching medical students musculoskeletal examination skills: identifying barriers to learning and ways of overcoming them. Scand J Rheumatol. 2004;33(1):47-51. https://doi.org/10.1080/03009740310004108
- O’Dunn-Orto A, Hartling L, Campbell S, Oswald AE. Teaching musculoskeletal clinical skills to medical trainees and physicians: a Best Evidence in Medical Education systematic review of strategies and their effectiveness: BEME Guide No. 18. Med Teach. 2012;34(2):93-102. https://doi.org/10.3109/0142159X.2011.613961
- Hose MK, Fontanesi J, Woytowitz M, Jarrin D, Quan A. Competency based clinical shoulder examination training improves physical exam, confidence, and knowledge in common shoulder conditions. J Gen Intern Med. 2017;32(11):1261-5
- Battistone MJ, Barker AM, Grotzke MP, Beck JP, Lawrence P, Cannon GW. Mini-residency in musculoskeletal care: a national continuing professional development program for primary care providers. J Gen Intern Med. 2016;31(11):1301-7.
- Battistone MJ, Barker AM, Grotzke MP. Effectiveness of an interprofessional and multidisciplinary musculoskeletal training program. J Grad Med Educ. 2016;8(3):398-404.
- Pammi M, Dempsey EM, Ryan CA, Barrington KJ. Newborn resuscitation training programmes reduce early neonatal mortality. Neonatology. 2016;110(3):210-224. https://doi.org/10.1159/000443875
- Moretti MA, Cesar LA, Nusbacher A, Kern KB, Timerman S, Ramires JA. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. 2007;72(3):458-465. https://doi.org/10.1016/j.resuscitation.2006.06.039



There are no comments for this article.