Background and Objectives: Interprofessional education is a critical component of medical student training, yet it is often difficult to implement. Medical students who learn with, from, and about learners from other disciplines have been shown to create more effective and safe health care teams. The investigators wanted to know how participating in two interprofessional observed structured clinical exams (OSCEs) at Tufts University School of Medicine (TUSM) would affect changes in medical students’ attitudes and values in interprofessional teamwork.
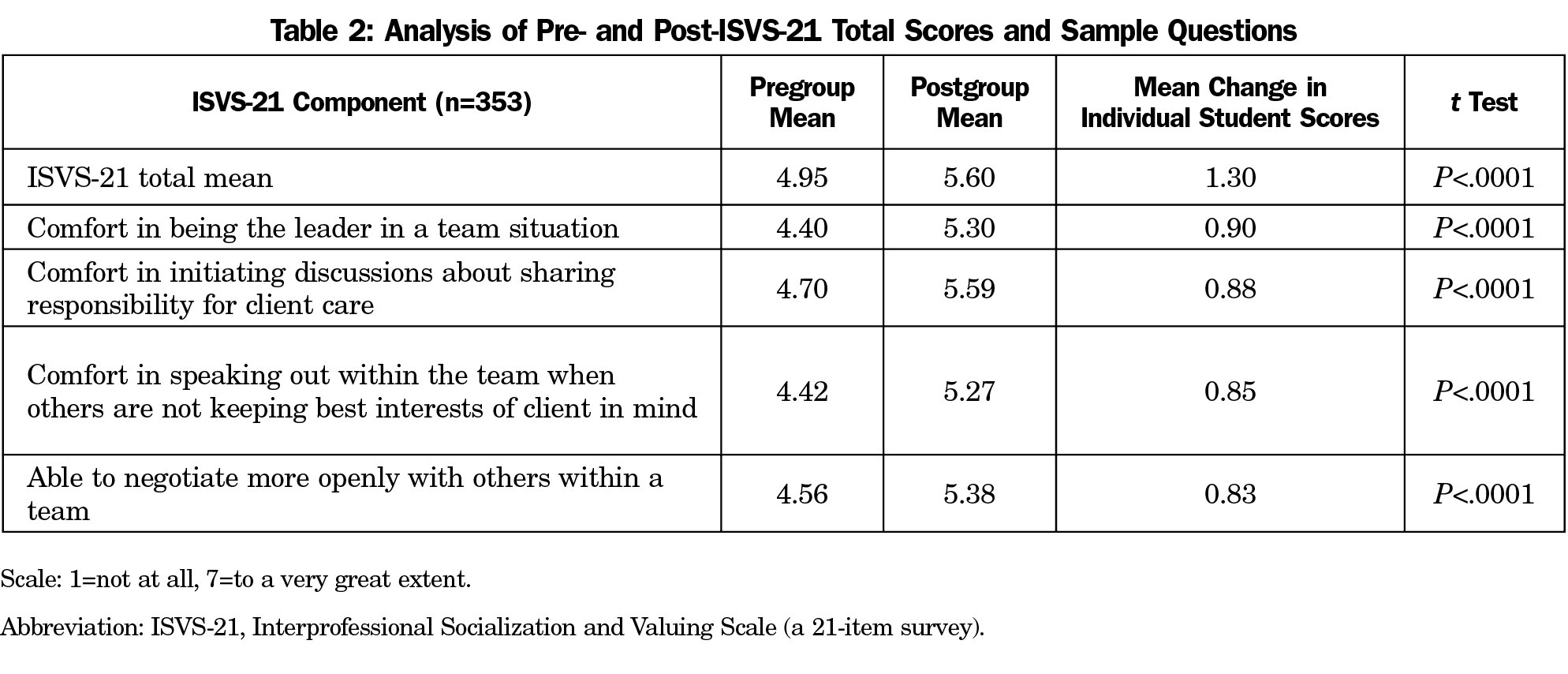
Methods: For the academic years 2017 and 2018, two interprofessional case scenarios were integrated into OSCEs for third-year medical students at TUSM, with an allied embedded actor (AEA) playing a social worker to an end-of-life scenario, and an AEA playing the role of a pharmacy student added to a chronic pain scenario. Students participated in didactic training about interprofessional teamwork and received structured feedback regarding interprofessional competencies following simulation cases. Changes in interprofessional knowledge and attitudes were assessed by comparing student pre- and postscenario mean scores on the Interprofessional Socialization and Valuing Scale (ISVS-21, a 21-item scale survey), with students rating themselves on a Likert scale from 1 (not at all) to 7 (to a very great extent). We performed paired t-test analysis on individual pre- and post-ISVS-21 means.
Results: Three hundred fifty-three of the 417 participating medical students fully completed pre- and postsurveys. Students reported significant changes in interprofessional knowledge and attitudes (mean change=1.3, P<.0001). Students and faculty regarded the interprofessional cases very highly.
Conclusions: Placing interprofessional cases involving AEAs into OSCE events is easily replicated, and positively impacts students’ attitudes and values in interprofessional knowledge.
Joint, active learning experiences with multiple disciplines are believed to be an effective approach to preparing professionals to work in collaborative health care teams and settings.1-7 However, the logistical challenges of training students in an interprofessional education (IPE) environment can be daunting. We wanted to know how participating in two interprofessional observed structured clinical exams (OSCEs) at TUSM would affect changes in medical students’ attitudes and values in interprofessional teamwork. The OSCEs are a series of standardized patient (SP) experiences that incorporate observation and evaluation of students for a variety of clinical skills.8 We explored the effects of incorporating allied embedded actors (AEAs) into two interprofessional case scenarios. AEAs are individuals added to an SP scenario who are scripted to provide realism, specific challenges, or additional information, such as assuming the role of a pharmacist or social worker.9,10 The AEAs may be either outside nonprofessionals or students in the relevant discipline. In our scenarios, the AEAs played the roles of social work and pharmacy students in an end-of-life discussion and a chronic pain management scenario, respectively, both complex situations requiring interprofessional teamwork.
Although other studies have reported use of embedded actors, OSCEs and IPE training,11,12 our study is unique in that we incorporated all three of these aspects and studied it with a validated tool.
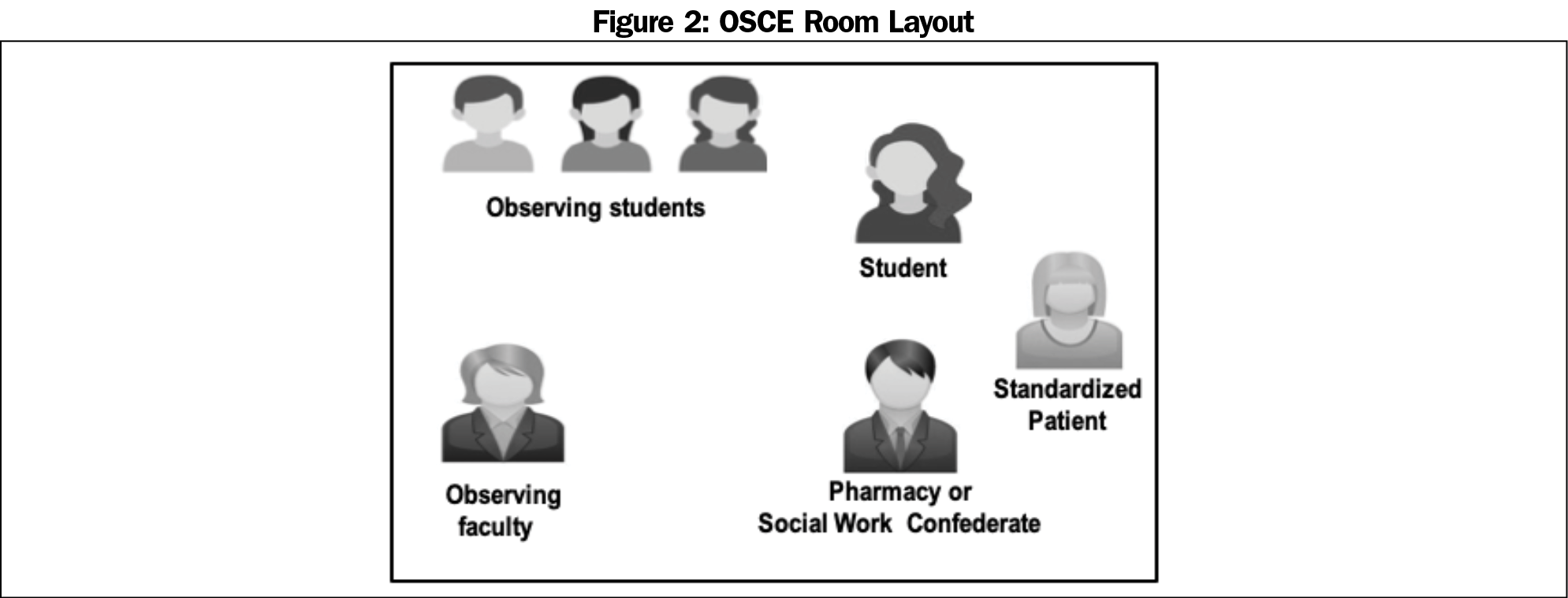
Our pilot study was conducted in the fall of 2017 and 2018 at three different locations: TUSM and two of its affiliates. The two interprofessional case scenarios were integrated into a required half-day formative OSCE for all TUSM third-year medical students. After an orientation that involved faculty teaching on end-of-life care, chronic pain and interprofessional teamwork, the students participated as the interviewer or one of several student observers in eight total stations. The two IPE stations involved a medical student meeting with: (1) the wife, adult child, and an AEA playing the role of a social worker regarding end-of-life issues in the ICU; and (2) An AEA playing the role of a pharmacy student and patient with complex chronic medical and pharmacy needs. In year 1 of the study the AEAs were professional standardized patients (SPs). In year 2 one actual social work student participated at all three sites, and one actual pharmacy student participated at one site. Prior to participation in the OSCEs, a clinical pharmacist, a social worker and a physician provided training for the SPs and AEAs through mock scenarios.
The designated student interviewer was asked to huddle with the AEAs prior to conducting the patient interview. The Individual Teamwork Observation and Feedback tool (iTOFT, a checklist designed for completion during live observation and tested primarily in simulated sessions with a focus on teamwork, behaviors, and skills) guided feedback.13 We incorporated faculty instruction on end-of-life and chronic pain discussions, as well as education on IPE competencies into the event. We solicited faculty and student feedback after the event as described in Table 1.
We assessed the impact on interprofessional attitudes and values through comparison of students’ individual responses to pre- and post-Interprofessional Socialization and Valuing Scale (ISVS-21, a 21-item Likert-scale survey found to reliably measure changes in interprofessional attitudes and values in students and medical providers).14 The presurvey was completed immediately before the start of the OSCES and the postsurvey was completed immediately after the completion of the OSCES. A paired t test analyzed the difference between students’ pre- and post-ISVS-21 individual mean scores. See Table 1 for an outline of the educational event. All of our teaching materials can be viewed on the STFM Resource Library.15 The Institutional Review Board of TUSM and Maine Medical Center determined the study to be exempt.
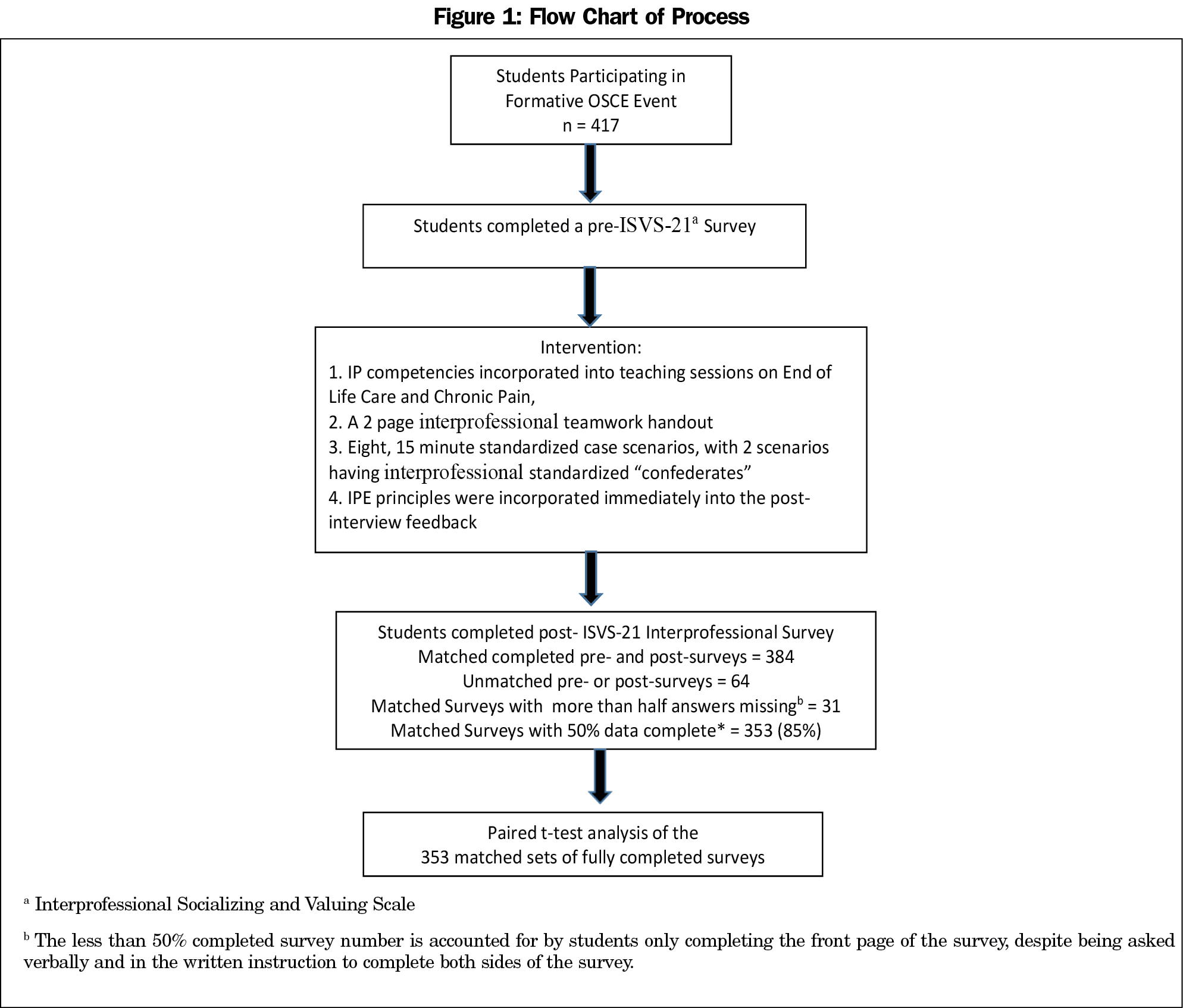
Three hundred fifty-three of 417 third-year medical students (85%) participated and completed matched pre- and post-ISVS-21 surveys (Figure 1). Table 2 illustrates the group means, change in individual pre- and post-OSCE means, and the significance level for the total ISVS-21 score and select questions. The pre-ISVS-21 group mean score of 4.95 on this 7-point scale was significantly different from the post-ISVS mean score of 5.60. (P<.0001). Faculty and student feedback was very positive, instructive, and used to improve the process over the 2 years of the study. Students self-reported “increased understanding of social work and pharmacy roles,” the “usefulness of huddles in clarifying roles,” and the “benefits of including other professionals on the team in difficult situations.”
Our study demonstrates that simulation in the form of OSCE cases with allied embedded actors is a viable and effective method for incorporating IPE education into the medical school curriculum. The utilization of AEAs provides a unique opportunity for joint, active learning with students or professionals from other fields. Improvements in ISVS-21 survey scores indicate that this form of deliberate teaching and feedback can contribute to improved attitudes and values pertaining to interprofessional teamwork, as well as improved perceptions and understanding of other professional’s roles. The iTOFT served as a resource for structured feedback on observable behaviors related to shared decision making and the ability to successfully collaborate. As the use of standardized patient events (eg, OSCEs), are a ubiquitous form of clinical teaching in medical schools across the country,16 this avenue of student education is an accessible and realistic avenue to increase IPE education.17 Challenges include the additional time and possible expense of training standardized patient AEAs or, preferably, coordination with students of other disciplines, as well as enrolling faculty with expertise to facilitate IPE discussions.
Limitations to our study include the use of a single institution and its affiliates. Not all students completed the survey, and those who did may have been in an observational role as opposed to actively participating as the interviewer. Also, most AEAs were simulated interprofessional standardized patients rather than actual social work or pharmacy students, and there was some variability in their performance from year to year. However, this difference in consistency between the 2 years did not affect the survey scores.
Next steps would be to expand the study by including multiple schools, conducting more interprofessional cases, and having all AEAs be health profession students and have all participants complete the pre- and post-ISVS-21. Data could be organized to discern differences between interviewing and observing students, and differentiating the impact between the teaching and the OSCE. The ISVS-21 may be seen as containing medical-centric questions, so the development of another validated instrument to detect variables of interest following an IPE intervention for all health professions would also be helpful.
As the benefit and necessity of training the next generation of medical professionals in the skills and concepts needed for interprofessional collaboration become increasingly clear, the challenge remains to find available avenues to incorporate this training into modern medical school curricula. Our study highlights the impact that placing interprofessional cases involving AEAs into OSCE events has on student interprofessional attitudes and values. We believe this intervention is generalizable to other medical school settings and may help to address the gap in meaningful IPE experiences.
Acknowledgments
Funding Statement: This study was financially supported by a Tufts University of Medicine Innovations in Education Grant.
Presentations: This study appeared as a poster presentation at the Tufts University School of Medicine Mary Y. Lee Research Day on April 2, 2019.
References
- Barr H. Toward a theoretical framework for interprofessional education. J Interprof Care. 2013;27(1):4-9. https://doi.org/10.3109/13561820.2012.698328
- Gilbert J, Orchard C, Bainbridge L. A national interprofessional competency framework. 2010; www.cihc.ca/files/CIHC_IPCompetencies_Feb1210.pdf. Accessed March, 2014.
- Kent F, Keating J. Patient outcomes from a student-led interprofessional clinic in primary care. J Interprof Care. 2013;27(4):336-338. https://doi.org/10.3109/13561820.2013.767226
- National Center for Interprofessional Practice and Education. Interprofessional NCf, Education Pa. 2015. https://nexusipe.org/. Accessed April 4, 2017.
- Reeves S, Fletcher S, Barr H, et al. A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Med Teach. 2016;38(7):656-668. https://doi.org/10.3109/0142159X.2016.1173663
- Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2008;1(1):CD002213. https://doi.org/10.1002/14651858.CD002213.pub2
- Lutfiyya MN, Chang LF, McGrath C, Dana C, Lipsky MS. The state of the science of interprofessional collaborative practice: a scoping review of the patient health-related outcomes based literature published between 2010 and 2018. PLoS One. 2019;14(6):e0218578. https://doi.org/10.1371/journal.pone.0218578
- Cömert M, Zill JM, Christalle E, Dirmaier J, Härter M, Scholl I. Assessing communication skills of medical students in Objective Structured Clinical Examinations (OSCE)-A systematic review of rating scales. PLoS One. 2016;11(3):e0152717. https://doi.org/10.1371/journal.pone.0152717
- Nestel D, Mobley BL, Hunt EA, Eppich WJ. Confederates in health care simulations: not as simple as it seems. J Clinical Simulation in Nursing. 2014;10(12):611-616. https://doi.org/10.1016/j.ecns.2014.09.007
- Sanko JS, Shekhter I, Kyle RR Jr, Di Benedetto S, Birnbach DJ. Establishing a convention for acting in healthcare simulation: merging art and science. Simul Healthc. 2013;8(4):215-220. https://doi.org/10.1097/SIH.0b013e318293b814
- Kumar SP, Prasad K, Sciences A. Use of objective structured clinical examination and structured clinical instruction module for interprofessional education on cancer: A focused review. International Journal of Health. 2012;1(3):135.
- Shinnick M, O’Gara E. Interprofessional Objective Structured Clinical Examination (IP-OSCE). 2015. https://apps.medsch.ucla.edu/ipe/docs/9A_ip_osce_background_guide_FINAL.pdf. Accessed July 9, 2019.
- Thistlethwaite J, Dallest K, Moran M, et al. Introducing the individual Teamwork Observation and Feedback Tool (iTOFT): development and description of a new interprofessional teamwork measure. J Interprof Care. 2016;30(4):526-528. https://doi.org/10.3109/13561820.2016.1169262
- Bloorview Research Institute. Interprofessional Socialization and Valuing Scale. 2017. http://research.hollandbloorview.ca/Outcomemeasures/isvs. Accessed April, 2019.
- Cyr P, Schirmer J, Hayes V. Incorporating Interprofessional Standardized Patient Experiences into OSCEs. STFM Resource Library; 2019. https://resourcelibrary.stfm.org/viewdocument/incorporating-interprofessional-sta?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments&CLK=06752064-48a1-4055-aa08-40ce1a2f0029. Accessed September 9, 2019.
- Association of American Medical Colleges. Number of Medical Schools Requiring Final SP/OSCE Examination. LCME Annual Medical School Questionnaire Part II, 2006-2007 Through 2015-2016. 2019; https://www.aamc.org/initiatives/cir/406426/9.html. Accessed May 13, 2019.
- Mann KV, Mcfetridge-Durdle J, Martin-Misener R, et al. Interprofessional education for students of the health professions: the “Seamless Care” model. J Interprof Care. 2009;23(3):224-233. https://doi.org/10.1080/13561820802697735



There are no comments for this article.