Background and Objectives: To achieve overall health, physicians must understand how community and population health impacts individual health. Although several US medical schools have incorporated community health assessment project requirements into traditional curricula, examples in longitudinal integrated clerkships are unknown. This study was designed to assess alumni perceptions of the influence of community health assessment projects, a core component of the University of Minnesota Rural and Metropolitan Physician Associate Program’s (RPAP/MetroPAP) 9-month longitudinal integrated curriculum.
Methods: This 2018 study consisted of a descriptive cross-sectional survey of 480 RPAP/MetroPAP alumni who completed 457 community health assessment projects between 2004/2005 and 2016/2017. The authors administered a 14-item survey requesting date and location of RPAP/MetroPAP 9-month placement, name of project, source of project idea, and perception of project influence on professional activities. Quantitative data were collected using 4-point Likert scales. We collected qualitative data with open text boxes.
Results: The survey response rate was 42.29% (203/480). A key finding was alumni perceived project ideas arising from community partners had greater impact on their acquisition of several community engagement skills. One-half reported projects influenced their professional activities, evidenced by ongoing community engagement, interest and participation in public health and preventive health initiatives, efforts to learn about specific health issues, social determinants of health and patient advocacy.
Conclusions: This exploratory study suggests medical student community health assessment projects enhance community engagement and soliciting project ideas from community partners increases student acquisition of community engagement skills.
Since the Association of American Medical Colleges (AAMC) and Institute of Medicine (IOM) recommended improved population health education in medical schools,1,2 several incorporated community health projects into their core curricular requirements.3-6
In 2004/2005, University of Minnesota’s (UMN) Rural and Metropolitan Physician Associate Programs (RPAP/MetroPAP), established in 1971/2010 respectively, implemented Community Health Assessment Projects (CHAPs) as part of its Longitudinal Integrated Curriculum (LIC).
RPAP/MetroPAP provides a 9-month community-based educational experience for approximately 40 third-year medical students who live and train in rural and urban underserved communities across Minnesota and western Wisconsin. The goal of RPAP/MetroPAP’s CHAP requirement is to teach community engagement skills for effective community partnership to improve population health.
RPAP/MetroPAP students independently access online community-oriented primary care (COPC)
7 learning modules, review public health data, and consult with preceptors and community members to choose a CHAP. Each (1) identifies a population experiencing, or at risk for poor health, (2) defines a health problem, (3) partners with stakeholders to intervene, and (4) evaluates their intervention. Final CHAP products include research papers and posters.
Although students and faculty review the CHAP curriculum annually, its long-term influence on alumni has not been assessed. This exploratory study was designed to assist curriculum design, gather reflective feedback regarding alumni perception of CHAPs effectiveness in teaching community engagement skills, and assess CHAP’s influence on professional population health activities.
This 2018 study consisted of a descriptive cross-sectional survey of 459 RPAP and 21 MetroPAP alumni who completed 457 CHAPs from 2004/2005 through 2016/2017. We obtained contact information from the UMN RPAP/MetroPAP database. Quantitative and qualitative data were collected using the online research platform Qualtrics with 4-point Likert scales and open text boxes. The UMN Institutional Review Board deemed the study exempt.
The authors developed a 14-item survey requesting date, location of RPAP/MetroPAP 9-month placement, CHAP name, project idea source, and perception of project influence on professional activities. Alumni rated level of agreement with CHAP enhancing community engagement skills and described ongoing participation in community, population or public health initiatives. The authors oversaw all data collection. Reliability and validity of data collection instruments were not measured. Scales and format for questions regarding community engagement skills were adapted from a RPAP/MetroPAP Community Partner Evaluation form.
We summarized survey data with descriptive statistics. Fisher exact tests, comparing nonrandom associations between variables in relatively small sample sizes, were used to compare responses between time intervals, project types, CHAP idea source, and community size based on RUCA codes.8 We used SAS V9.3 (Institute Inc, Cary, NC) for analysis, and we used NVIVO (version 10.2.2.0, QRS International) for qualitative analysis of text-based data, including counting and categorizing free-text comments. We independently coded text for context, patterns and processes to understand relevance, significance and meaning, collaboratively grouping comments into themes. Disagreements in categorization were resolved by consensus.
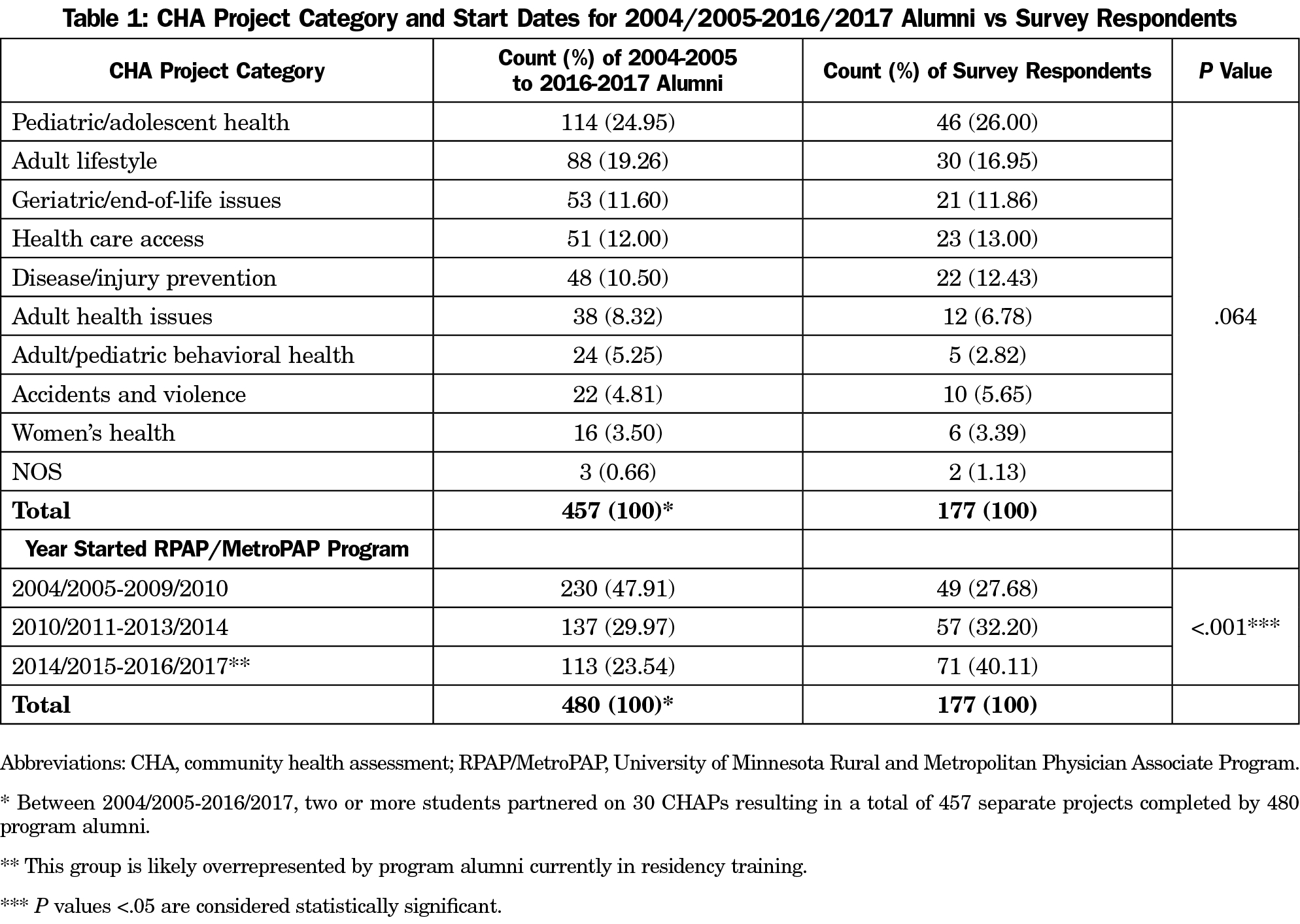
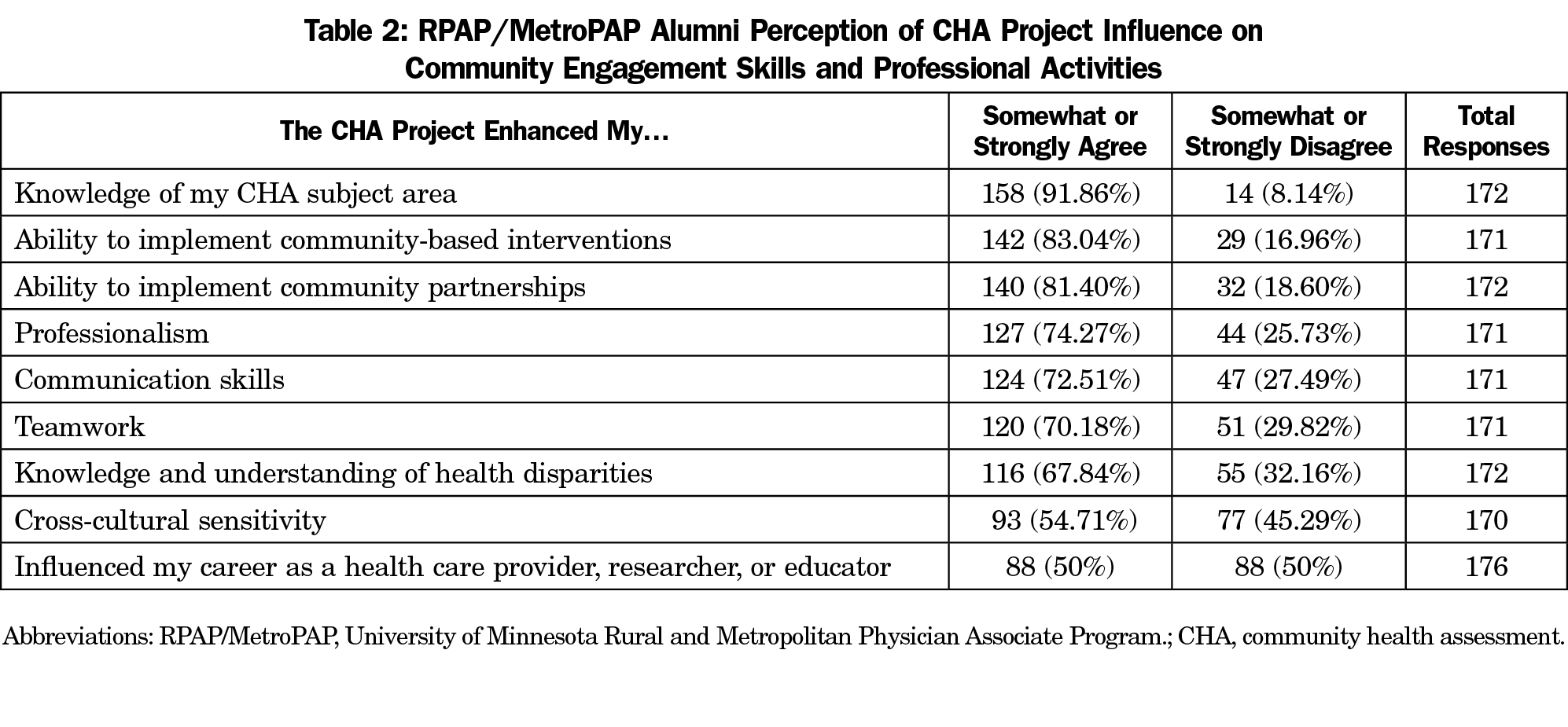
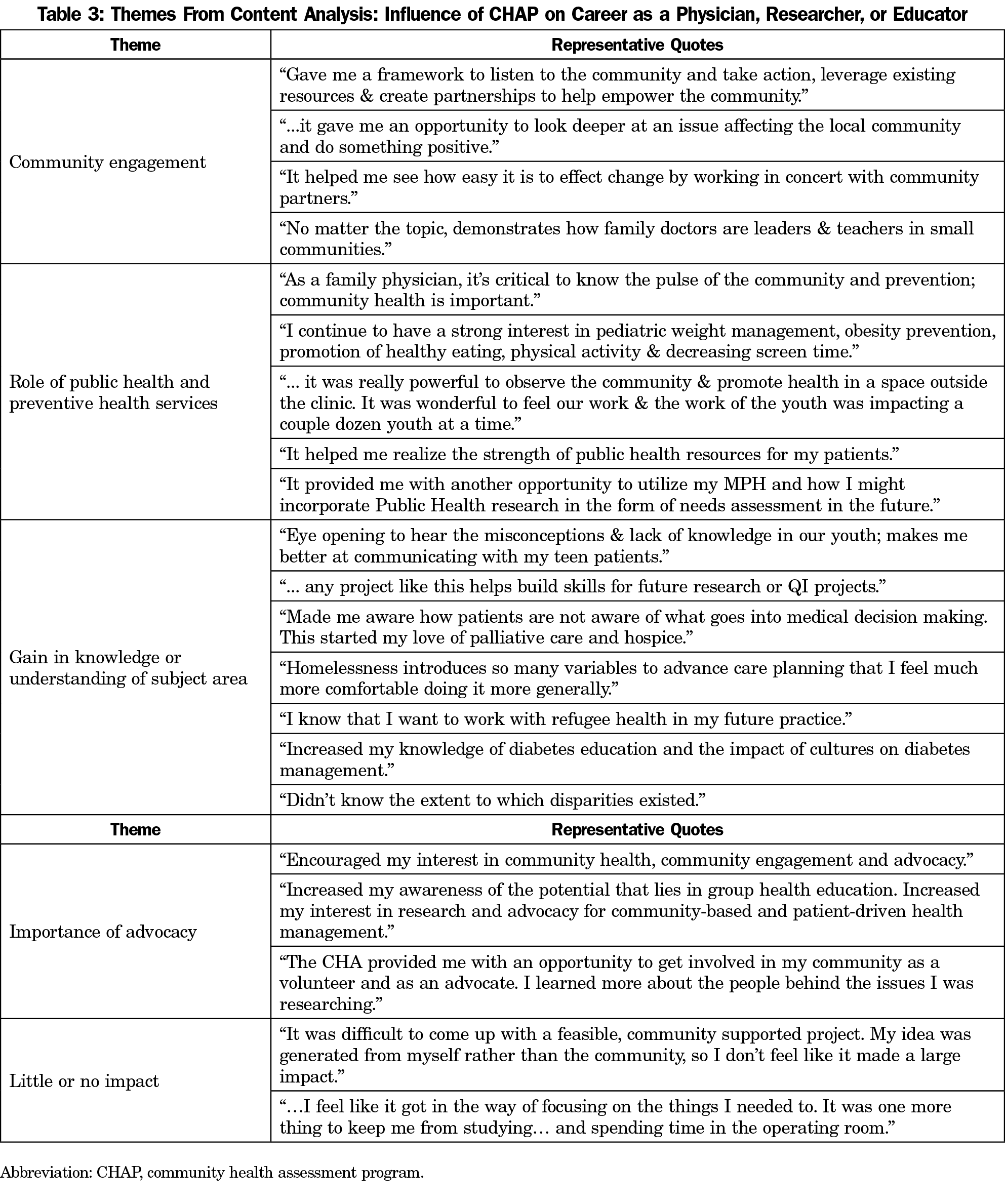
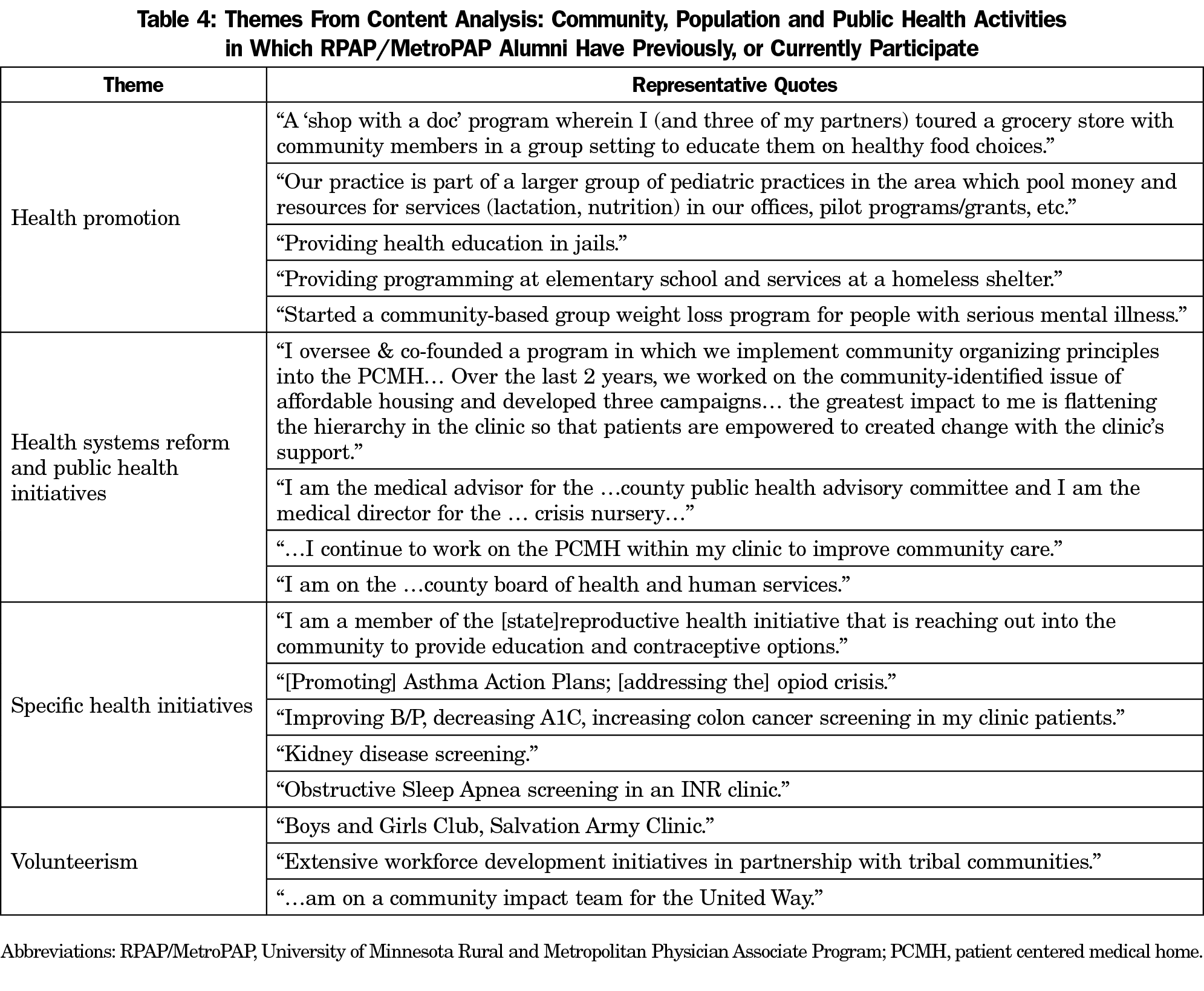
The survey response rate was 42.29% (203/480). Table 1 compares all program alumni participation years and CHAP categories with respondents. Table 2 demonstrates two-thirds of respondents perceived enhanced community engagement skills in all but cross-cultural sensitivity. One-half (88/176) agreed CHAPs influenced their careers as health care providers, researchers, or educators. Tables 3 and 4 list career-influenced themes and types of community, population, or public health activities in which alumni participated.
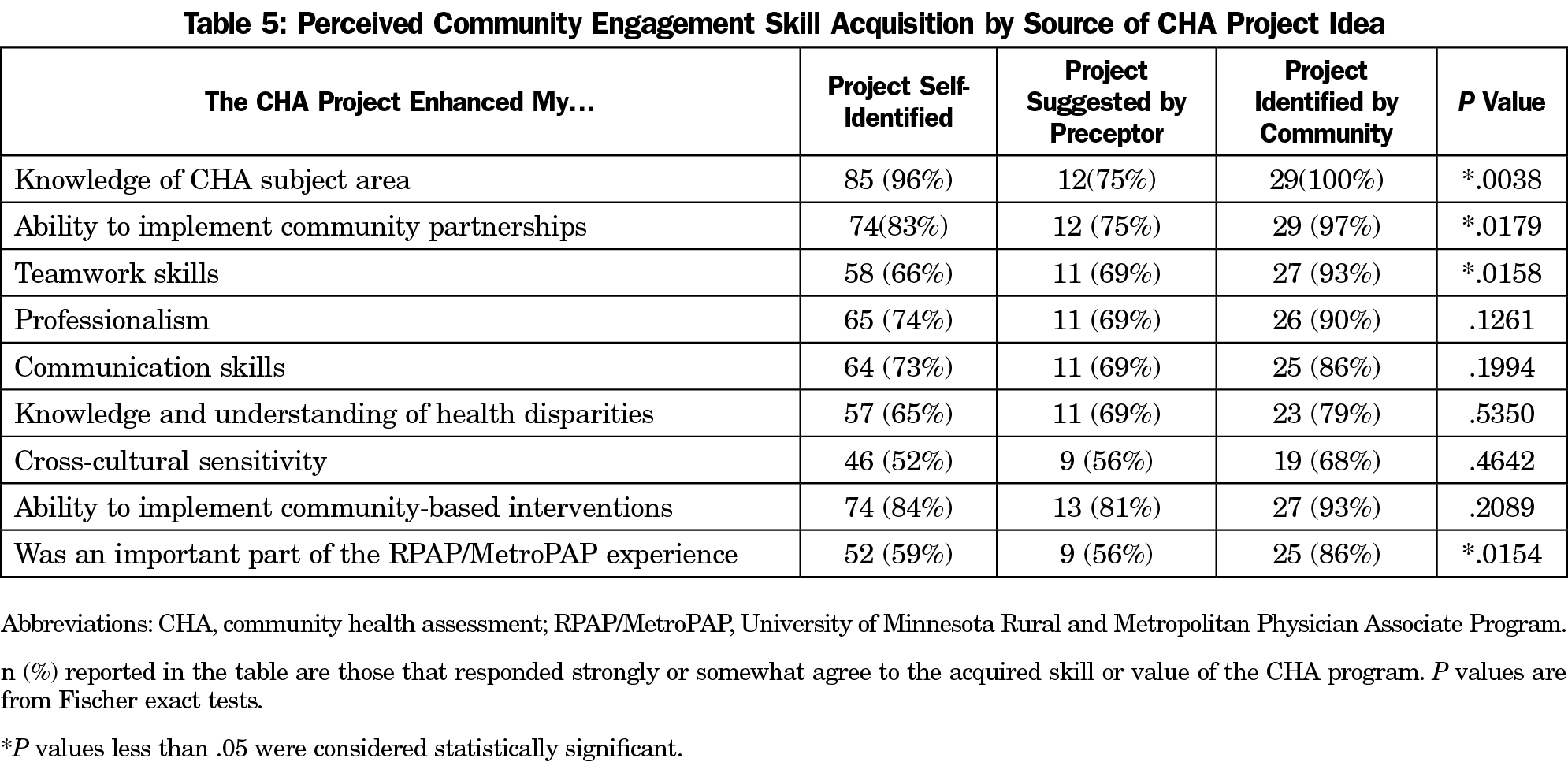
We compared perceived engagement skill acquisition to CHAP idea source. Table 5 shows alumni perceived gaining significantly greater knowledge of CHAP subject, ability to create community partnerships, and teamwork skills when CHAPs were identified by community, versus by preceptors or themselves. Data also shows they perceived CHAPs more important to the RPAP/MetroPAP experience.
Though recent studies have shown enhanced short-term acquisition of community health assessment knowledge and skills in preclinical years,9,10 data on perceived long-term influence of CHAP’s completed on traditional clerkships and LIC’s have not been reported. The RPAP/MetroPAP CHAP requirement was designed to emphasize the physician role in forging community partnerships to improve population health. This necessitates teaching community engagement skills and may be more easily accomplished on LICs, where medical students are embedded in primary care settings for extended time. Alumni perception of increased skill acquisition with community partner-identified projects should influence CHAP curricular design.
The significance of finding half of alumni agree CHAPs influenced their career is unclear, due to the time passed since participation. However, qualitative analysis of favorable comments reveals alumni gained understanding of ways physicians can assess and respond to community needs, learn about public and preventive health initiatives and advocate for patients. Examples of professional activities in which alumni engaged demonstrate their continued interest in promoting population health within the community.
Limitations
The study survey instrument was created by the authors and not validated prior to use. We did not provide definitions of survey terms; different interpretations may have influenced responses. Low response rate and potential nonresponse bias are also limitations. Those influenced most or least strongly by RPAP/MetroPAP may have been more likely to complete surveys. There is no within-sample comparison of CHAPs to other LIC curricular elements, potentially contributing to a reporting bias toward desirable answers. Recall bias is a study limitation, but data retrieval from program records supplemented the 15.71% (30/191) of alumni reporting no recollection of CHAP details. Since 40.11% (71/176) of respondents may have been residents, residency curricula likely influenced their professional activities.
A commitment to primary care and underserved rural or urban populations is required for student acceptance in RPAP/MetroPAP. Study findings may not be generalizable to academic programs with different student eligibility criteria. This study relies on alumni perceptions and does not test causation or objectively assess learning outcomes. By assessing engagement skills of alumni before and after RPAP/MetroPAP, compared to a matched control group, a more accurate measure of CHAPs long-term effectiveness could be determined.
Data gathered from this cross-sectional survey of UMN RPAP/MetroPAP alumni provides important information regarding perception of one LIC’s CHAP requirement. Findings suggest curricula supporting projects identified by community partners are more effective at enhancing engagement skills acquisition than those identified by students or preceptors. This understanding is key to teaching medical students the importance of community partnership to improve population health.
Acknowledgments
The authors acknowledge Deborah Finstad for guidance with project study design and Qualtrics survey development, Scott Lunos, MS, and Ms Finstad, Kirby Clark, MD, and Darin Brink, MD, for assistance with data analysis.
Disclaimer: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) Award Number UL1TR000114. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- Association of American Medical Colleges. Medical School Objectives Project: Report II Contemporary issues in medicine: medical informatics and population health. Washington, DC: AAMC; June 1998.
- Institute of Medicine. Who Will Keep the Public Healthy? Educating public health professionals for the 21st century. Washington, DC: National Academies Press; 2007.
- Magill MK, Quinn R, Babitz M, Saffel-Shrier S, Shomaker S. Integrating public health into medical education: community health projects in a Primary Care Preceptorship. Acad Med. 2001;76(10):1076-1079. doi:10.1097/00001888-200110000-00022
- McIntosh S, Block RC, Kapsak G, Pearson TA. Training medical students in community health: a novel required fourth-year clerkship at the University of Rochester. Acad Med. 2008;83(4):357-364. doi:10.1097/ACM.0b013e3181668410
- Bonafede K, Reed VA, Pipas CF. Self-directed community health assessment projects in a required family medicine clerkship: an effective way to teach community-oriented primary care. Fam Med. 2009;41(10):701-707.
- Prunuske J, Remington PL. A Community Health Assessment Curriculum to Develop Population Health Competencies. PRiMER. 2017;1:1. doi:10.22454/PRiMER.2017.1.1
- Liaw W, Rankin J, Bazemore A, Ventres W. Teaching population health: community-oriented primary care revisited. Acad Med. 2017;92(3):419. doi:10.1097/ACM.0000000000001552
- United States Department of Agriculture Economic Research Service. 2010 Rural-Urban Commuting Area (RUCA) Codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation/. Accessed July 8, 2020.
- Abu-Odeh D, Martos AJ, Sheffer CE. Teaching population health to medical students through the community health assessment. Educ Prim Care. 2017;28(4):237-242. doi:10.1080/14739879.2016.1259591
- Beehler S, Boulger J, Friedrichsen SC, Onello EC. Teaching community health needs assessment to first year medical students: integrating with longitudinal clinical experience in rural communities. J Community Health. 2019;44(4):784-789. doi:10.1007/s10900-019-00651-8



There are no comments for this article.