Background and Objectives: Medical student-run free clinics (SRFC) provide underserved patients access to health care. Few studies have examined the effects of specific care models implemented by these clinics. We looked at the impact of a continuity of care delivery model on chronic care outcomes at an SRFC sponsored by Ohio State University College of Medicine.
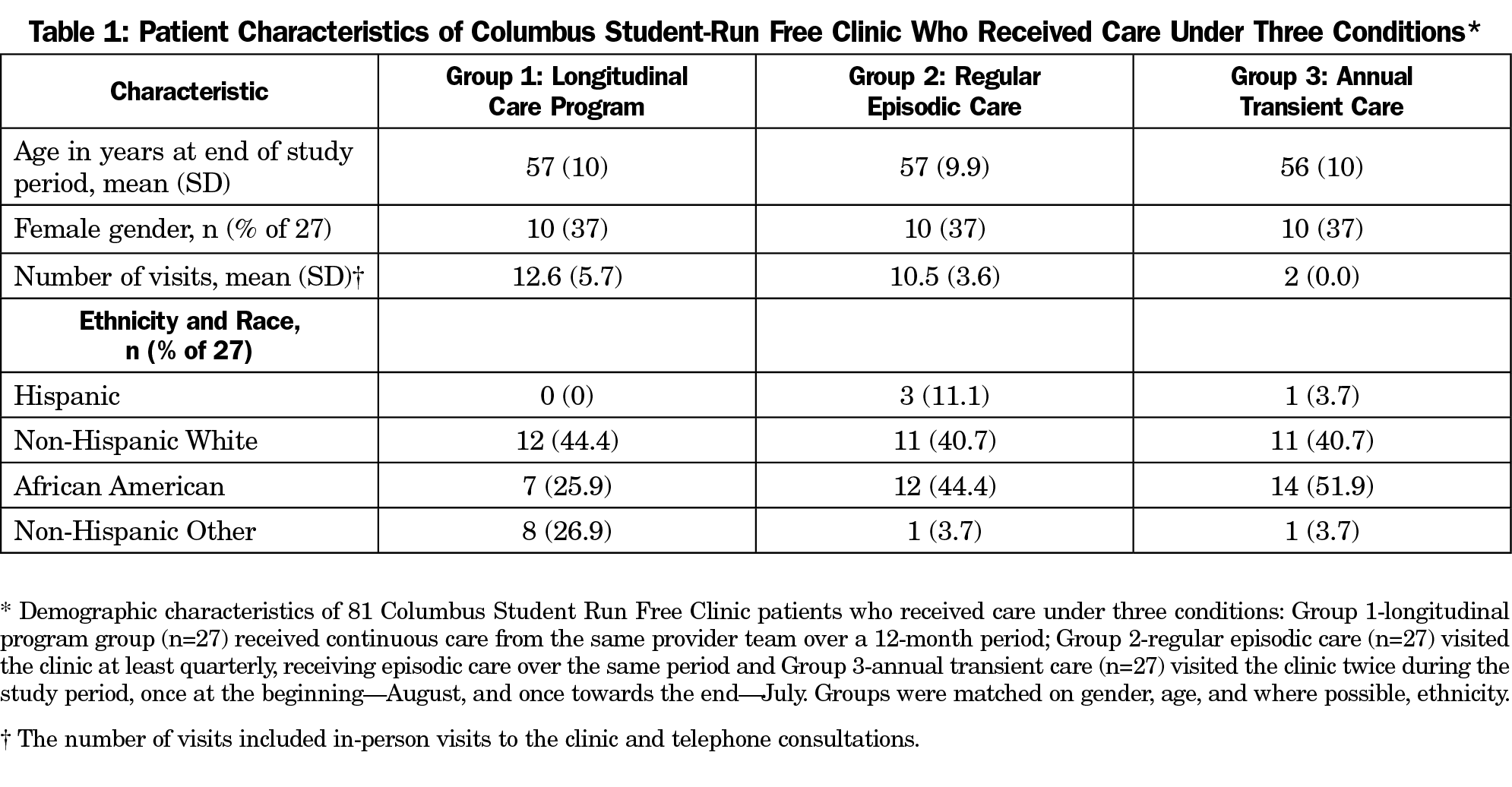
Methods: Using the SRFC electronic medical records, we abstracted health records of patients at risk for atherosclerotic cardiovascular disease (ASCVD). We formed three study groups matched on age and gender. Group 1 were the patients enrolled in a continuity of care program, Group 2 were patients who visit the SRFC at 3-month intervals, and Group 3 were sporadic visitors. Authors compared groups’ ASCVD risk score change over 12 months using a Group x Time Analysis of Variance.
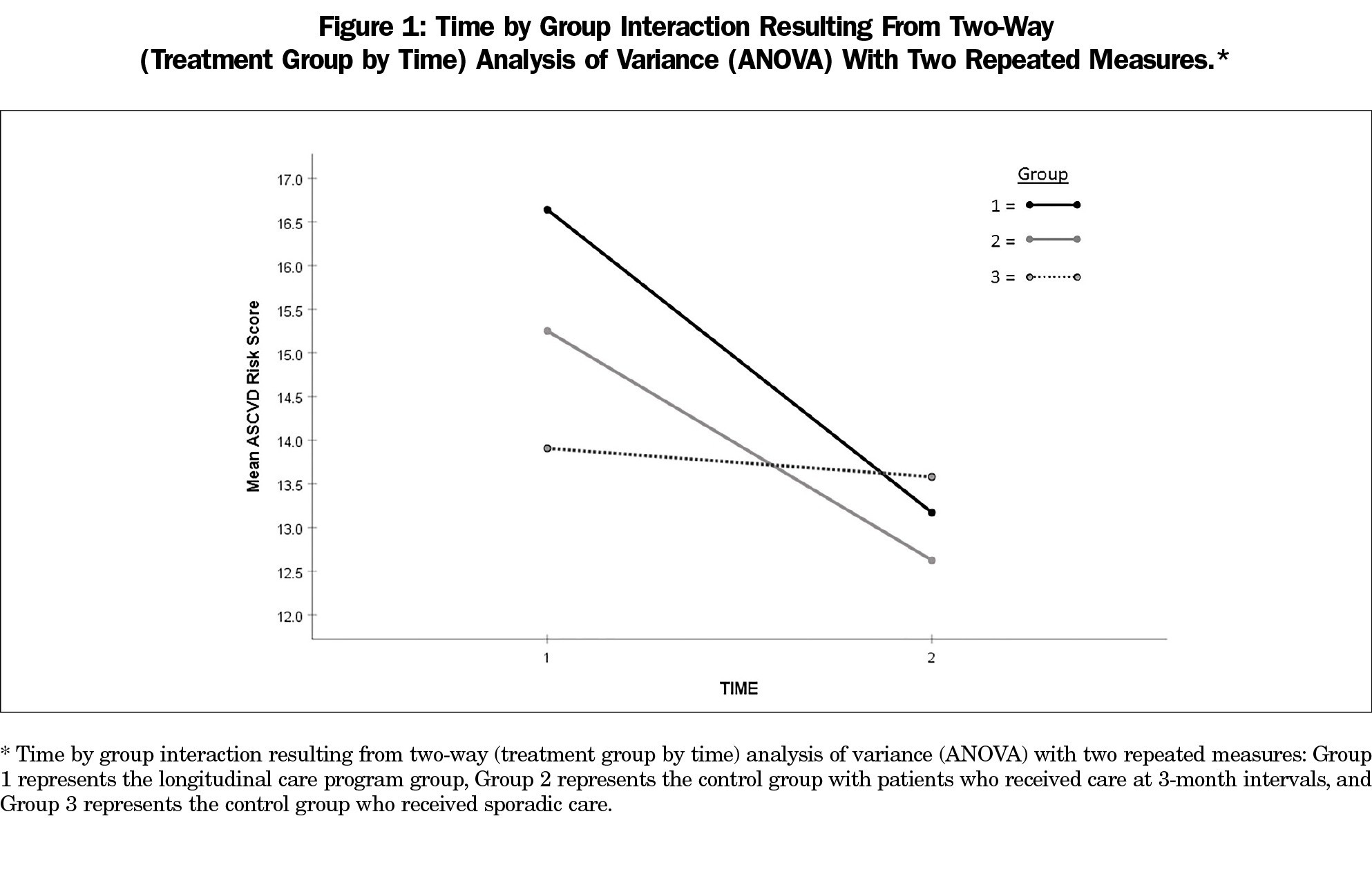
Results: We identified 81 subjects that met the qualifications for this study and assigned them to one of the three study groups. A Group x Time interaction showed that mean ASCVD risk scores improved significantly for continuity of care patients and regular visitor controls, but not for sporadic controls (F=3.82; df=2/1.72; P=.035; es=1.28).
Conclusions: This SRFCs continuity of care delivery had no appreciable impact on lowering ASCVD Risk scores over and above frequent regular visits to the clinic. This finding suggests that SRFCs should focus on getting their chronic patient population to maintain a schedule of frequent check-ups, without investing in continuity of care. Longer-term studies are needed to detect a continuity of care delivery model effect.
The modern free health clinic movement originated in the 1960s, but did not become a common medical education venue until 2008.1-3 By 2017, most (72%) graduating medical students reported participation in student-run free clinics (SRFCs),4 that serve an estimated 10 million disadvantaged or uninsured Americans as their sole source of medical care.5-6 The early literature on SRFCs focused on learner benefits rather than care effectiveness.7-8 More recently, there has been a shift toward the study of chronic care quality delivered at SRFCs.9-13
Beyond offering patient care experience to medical learners, SFRCs can teach new health care delivery models, including the patient-centered medical home (PCMH).14-15 The PCMH is defined by the core tenants of primary care, and emphasizes a physician-patient partnership that includes improved communication, coordination and continuity of care.14, 16
The purpose of this study was to compare the Atherosclerotic Cardiovascular Disease (ASCVD) Risk scores of chronic patients enrolled in our SRFC’s Longitudinal Care Program (LCP) with two matched sample control groups: episodic visitors, and infrequent visitors. Our hypothesis was that LCP patients would show significantly reduced ASCVD risk scores compared to both control groups.
Program Setting
Our SRFC serves an average of 30 uninsured/underserved patients with chronic conditions per weekly session. During the study year, we adopted an LCP based on the tenets of PCMHs, which provided patients: (1) continuity—a relationship with a single student provider for 12 months, (2) coordination of care across the healthcare network, and (3) quarterly check-ups with coaching related to medication and lifestyle management.14,16-18 Patients with chronic conditions who declined LCP participation received care under the previous episodic model.
Providers and Provider Training
LCP providers were volunteer fourth-year medical students supervised by attending physicians. Providers received training that covered topics related to treating patients with chronic diseases, including health coaching communication strategies.
Study Procedures
We used the SRFCs dedicated electronic medical records (EMR) to retrospectively identify three patient types: LCP participants, episodic, and infrequent visitors; and to extract patient health records, including comorbidities, smoking status, blood pressure, high-density (HDL) and low-density (LDL) lipoprotein levels, and total cholesterol. We matched LCP participants to the other patient types by age, gender, and the presence of ASCVD risk factors. This provided two control groups: the episodic visitors (had similar visit patterns to the LCP) provided a comparison for evaluating the continuity-of-care effect; and infrequent visitors (visited twice, almost a year apart) provided a comparison for evaluating the effect of quarterly checkups. We excluded LCP patients with incomplete health records or unsuitable matched controls (n=6).
We chose ASCVD risk as our primary outcome because it consists of modifiable risk factors susceptible to change through coaching, thus serving as a good measure of longitudinal chronic care benefits.19-21 We used the ASCVD Risk Estimator Plus to calculate risk scores.22 Our institutional review board approved this study as a retrospective chart review.
Data Analysis
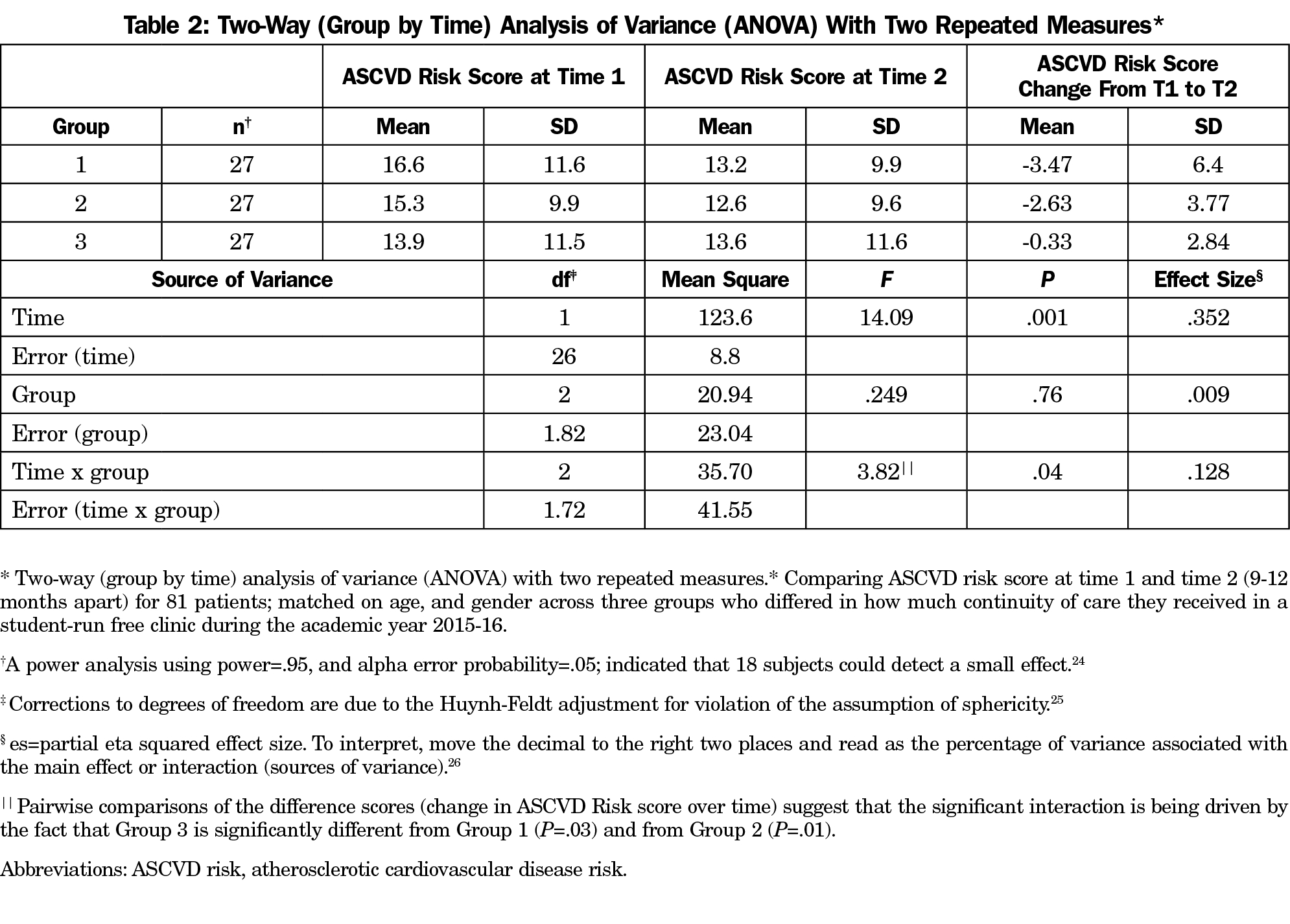
We compared ASCVD risk scores using a two-way (group by time) analysis of variance (ANOVA) with two repeated measures. Post hoc tests were conducted on significant main effects or interactions. Time between baseline (T1) and follow-up (T2) ASCVD risk scores was 12 months. We interpreted P values <.05 as significant.23
We identified 81 patients to create three matched groups of 27 subjects each (Table 1). The two-way ANOVA showed a main effect for time, (F=14.09; df=1,26; P=.001; effect size [es]=.352) suggesting that ASCVD risk scores declined significantly by the end of the study period for all three groups combined (Table 2). More importantly, we observed a significant time x group interaction (F=3.82; df 2, 1.72; P=.035; es=.128; Table 2, Figure 1) that indicated differences between groups in their rate of ASCVD Risk score decline. Post hoc analysis of the difference scores (Change from T1-T2) and Figure 1 showed that the significant interaction was driven by Group 3’s zero rate of change.
Our results showed that LCP patients and patients who visited the SRFC at similar time intervals, lowered their ASCVD Risk scores at about the same rate. This finding suggests that continuity of care and our LCP program did not have an appreciable effect on improving patient outcomes over and above regular visits to the clinic. However, these two groups demonstrated improved outcomes when compared to the other control group who received episodic care at least 9 months apart, suggesting that SRFCs should focus on promoting quarterly check-ups among chronic care patients.
This retrospective study builds on the work of others by evaluating an SRFC’s implementation of a PCMH model for longitudinal patient care through direct measures of patient outcomes.16 Although we were unable to document an effect related to continuity of care, we were able to show the importance of consistent, regular care of patients with chronic conditions related to ASCVD risk.
Limitations
One explanation of our findings is that the study period was not long enough to detect the impact of continuity of care and adherence to a PCMH model. Another is that there was not an appreciable difference between the LCP and regular visit cohorts regarding motivation to improve their health. We did not monitor the performance of the SRFC providers, so we cannot say whether they established the rapport needed to promote treatment plan adherence.
We suggest that SRFCs continue to assess the patient care outcomes for two reasons. First, because a central tenet of service learning is a reciprocal benefit between both parties involved, and second, because evidence-based practice is a central tenant of modern patient care. Using fourth-year medical students with faculty oversight, SRFCs can provide value to both the community and students through the evaluation and implementation of new patient care models.
Future Directions
These results merit further study of the potential long-term benefits associated with using a PCMH model with continuity of care in an SRFC. Further research should monitor patient outcomes of this care model for a longer period.
Acknowledgments
The authors acknowledge Tricia Mary Smith, undergraduate student in biology, for her help in abstracting and verifying patient data from the student-run free clinic electronic medical record.
References
- Reynolds HY. Free medical clinics: helping indigent patients and dealing with emerging health care needs. Acad Med. 2009;84(10):1434-1439. doi:10.1097/ACM.0b013e3181b6c3eb
- Meah YS, Smith EL, Thomas DC. Student-run health clinic: novel arena to educate medical students on systems-based practice. Mt Sinai J Med. 2009;76(4):344-356. doi:10.1002/msj.20128
- Liaison Committee on Medical Education Accreditation Standards. Functions and Structure of a Medical School. Standards for Accreditation of Medical Education Programs Leading to the MD Degree. Standard on Service Learning: Standard 6.6. Washington, DC: Association of American Medical Colleges; 2018. https://LCME.ORG/Publications/. Accessed September 4, 2020.
- Association of American Medical Colleges. AAMC Medical School Graduation Questionnaire, 2017 All Schools Summary Report. Washington, DC: Association of American Medical Colleges; July 2017.
- Trumbo SP, Schuering KM, Kallos JA, et al. The effect of a student-run free clinic on hospital utilization. J Health Care Poor Underserved. 2018;29(2):701-710. doi:10.1353/hpu.2018.0053
- Simpson SA, Long JA. Medical student-run health clinics: important contributors to patient care and medical education. J Gen Intern Med. 2007;22(3):352-356. doi:10.1007/s11606-006-0073-4
- Tran K, Kovalskiy A, Desai A, Imran A, Ismail R, Hernandez C. The effect of volunteering at a student-run free healthcare clinic on medical students’ self-efficacy, comfortableness, attitude, and interest in working with the underserved population and interest in primary care. Cureus. 2017;9(2):e1051. doi:10.7759/cureus.1051
- Smith SD, Johnson ML, Rodriguez N, Moutier C, Beck E. Medical student perceptions of the educational value of a student-run free clinic. Fam Med. 2012;44(9):646-649.
- Gorrindo P, Peltz A, Ladner TR, et al. Medical students as health educators at a student-run free clinic: improving the clinical outcomes of diabetic patients. Acad Med. 2014;89(4):625-631. doi:10.1097/ACM.0000000000000164
- Smith SD, Marrone L, Gomez A, Johnson ML, Edland SD, Beck E. Clinical outcomes of diabetic patients at a student-run free clinic project. Fam Med. 2014;46(3):198-203.
- Soltani M, Smith S, Beck E, Johnson M. Universal depression screening, diagnosis, management, and outcomes at a student-run free clinic. Acad Psychiatry. 2015;39(3):259-266. doi:10.1007/s40596-014-0257-x
- Rojas SM, Smith SD, Rojas S, Vaida F. Longitudinal hyperlipidemia outcomes at three student-run free clinic sites. Fam Med. 2015;47(4):309-314.
- Smith SD, Rojas SM, Huang J, Yang K, Vaida F. Longitudinal hypertension outcomes at four student-run free clinic sites. Fam Med. 2017;49(1):28-34.
- Riddle MC, Lin J, Steinman JB, et al. Incorporating the principles of the patient-centered medical home into a student-run free clinic. Adv Med Educ Pract. 2014;5:289-297. doi:10.2147/AMEP.S66762
- Lee JS, Combs K, Pasarica M; KNIGHTS Research Group 2016. Improving efficiency while improving patient care in a student-run free clinic. J Am Board Fam Med. 2017;30(4):513-519. doi:10.3122/jabfm.2017.04.170044
- Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601-612. doi:10.1007/s11606-010-1291-3
- Asgarova S, MacKenzie M, Bates J. Learning from patients: why continuity matters. Acad Med. 2017;92(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 56th Annual Research in Medical Education Sessions)(suppl):S55-S60. doi:10.1097/ACM.0000000000001911
- Gulliford M, Naithani S, Morgan M. What is ‘continuity of care’? J Health Serv Res Policy. 2006;11(4):248-250. doi:10.1258/135581906778476490
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. doi:10.1016/j.jacc.2017.11.006
- Berman AN, Blankstein R. Optimizing Dyslipidemia Management for the Prevention of Cardiovascular Disease: a Focus on Risk Assessment and Therapeutic Options. Curr Cardiol Rep. 2019;21(9):110. doi:10.1007/s11886-019-1175-z
- Rosenblit PD. Lowering Targeted Atherogenic Lipoprotein Cholesterol Goals for Patients at “Extreme” ASCVD Risk. Curr Diab Rep. 2019;19(12):146. doi:10.1007/s11892-019-1246-y
- ASCVD Risk Estimator Plus. Washington, DC: American College of Cardiology; Updated March 2019. http://tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate/. Accessed June 2018 through September 2019.
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0. Released 2017. Armonk, NY: IBM Corp.
- Faul F, Erdfelder E, Lang A-G, et al. G*Power Version 3.1.9.4. A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175-191. doi:10.3758/BF03193146
- Keppel G. Design and Analysis: A Researcher’s Handbook. 2nd ed. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1982:470-472.
- Draper SW. Effect size. http://www.psy.gla.ac.uk/~steve/best/effect.html. Published March 25, 2011, Updated January 26, 2020. Accessed March 14, 2020.



There are no comments for this article.