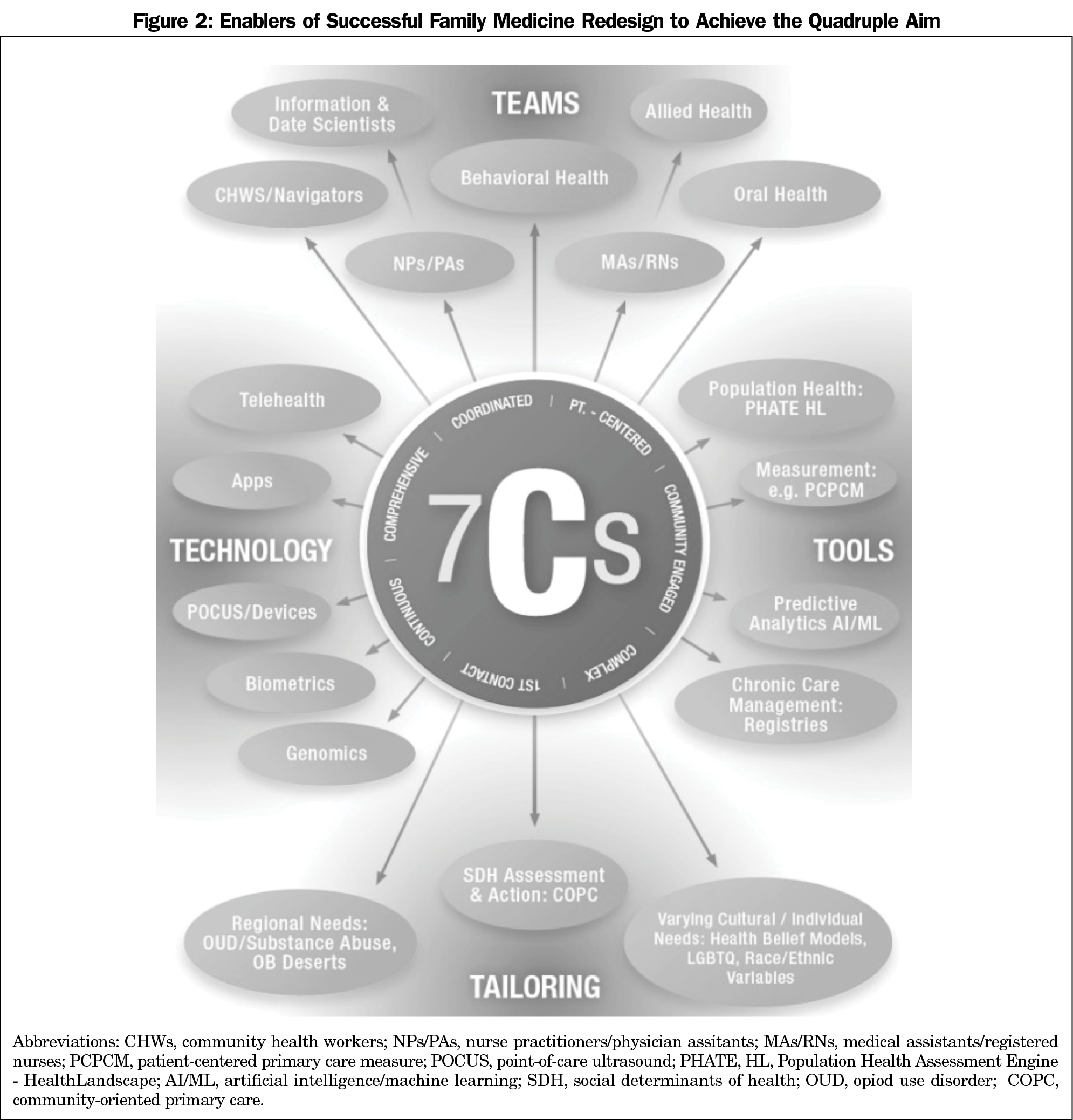
Amidst a pandemic that has acutely highlighted longstanding failings of the US health care system and the graduate medical education (GME) enterprise that serves it, educators prepare to embark on another revision of the program requirements for family medicine GME. We propose in this article a conceptual framework to guide this endeavor, built on a foundation of the core functions that Barbara Starfield suggested might explain primary care’s salutary effects. We first revisit these “4C’s”—first Contact, Continuity, Comprehensiveness, and Coordination—and how they might inform design thinking in primary care GME guideline revision. We also propose the addition of Community engagement, patient-Centeredness, and Complexity. Training residents to deliver on these “7C’s,” functions critical to the delivery of high-performing primary care, is essential if family medicine residency graduates are to serve the clearly articulated, but unrealized, quadruple aim for US health care: improved patient experience and population health at lower costs while preserving clinician well-being. Finally, we highlight and illustrate examples of four critical enablers of these 7C core functions of primary care that must be accommodated in training guidelines and reform, suggesting a need for resident competencies in Team-based, Tool- and Technology-enabled, Tailored (“4T’s”) care of patients and populations.
Prior to COVID-19, the US health care system was already associated with a sicker population, living shorter lives, with less accessible and affordable health care, facing mounting health disparities, at much greater expense than peer countries.1-3 Over the last 4 decades, the gap in life expectancy between the United States and other countries of similar wealth had grown,4,5 achieving a pre-COVID milestone not seen since the 1917-1918 flu pandemic: 3 consecutive years of declines in life expectancy. While other nations have heeded Declaration of Alma Ata guidance that primary care is “essential health care” and should be the “central feature and main focus” of all countries’ health systems, the United States has consistently underinvested in primary care and its workforce, which currently constitutes only 30% of all practicing physicians despite decades of efforts to reverse its steady declines.6-9
Ominously, despite nearly $18 billion in public investment and federal advisory board calls to push primary care above 40% of the total workforce, only 25% of the products of US graduate medical education enter primary care.10,11 Pediatrics and internal medicine produce increasing proportions of subspecialty graduates each year, their primary care outputs further compounded by growing entry into hospitalists careers.7,12,13 As leaders of the largest contributor to the primary care workforce—family medicine—enter a new decade seeking to redefine its program requirements, we must also consider its role in a health system that has failed to achieve its quadruple aim: excellent patient experience and population health at lower costs all while preserving waning clinician well-being. And if family medicine GME reform requires a conceptual compass to navigate these rough waters, Dr Barbara Starfield provided an excellent starting point. She defined the core functions of primary care thought responsible for its positive effects on access, equity, cost and quality using “4C’s”: first Contact, Continuity, Comprehensiveness, and Coordination. We propose these as a conceptual foundation for the next era of training in family medicine, but suggest the need for three additional “C’s”: Community engagement, patient-Centeredness, and Complexity, and competency in “4T’s”: Teams, Tools, Technology and Tailoring, for the future family medicine residents to emerge ready to serve the quadruple aim.
Explaining Primary Care’s Salutary Effects: Starfield’s 4C’s
Over a 25-year research career, Dr Starfield generated substantial evidence of primary care’s positive effects at the national, health system, state, and county level.14 She suggested that these benefits derived from four foundational functions served by primary care in health systems: the provision of first contact, continuous, comprehensive, and coordinated care. Since their inception, the 4C’s have explained the benefits of primary care, but have yet to be used together in total to guide graduate medical education in family medicine. A brief reexamination of each and its implications for family medicine GME redesign follows.
First Contact
In Lord Dawson’s 1920 UK report, primary care was initially declared the ideal point of first contact with health services, and a facilitator of entry into the rest of the health system.15 Unlike most highly developed nations, in the United States, residents train in a system that offers neither universal nor equitable access to insurance or first contact primary care.14 In fact, recent US nationally-representative surveys reveal that fewer than one in five Americans report having a personal or individual “usual source of care,” that this has been declining for decades,16 and that this trend disproportionately impacts the most vulnerable of US populations.17 Given growth in new first-contact options competing with primary care residency graduates such as online health avatars, urgent and retail clinics, and direct marketing by hospitals, primary care GME reformers should first be concerned with the demonstration that there is continued value in primary care as first contact. Fortunately, its effect in achieving desirable health system outcomes has been shown in a number of studies. In one US investigation, it was associated with an over 50% reduction in ambulatory episode-of-care expenditures.18 Evidence also suggests that patients who use a primary care physician as an initial point of contact use specialists and emergency rooms less frequently than those who do not have this relationship.19-21 Starfield herself demonstrated that first contact with a primary care physician is associated with more appropriate, more effective, and less costly care. 22 New GME guidelines training must help residents and graduates build skills in, and habits of retaining first contact with patients. This can be done by measuring access and time to third available virtual and in-person appointments, maintaining comprehensiveness, using telehealth, asynchronous communication, open-access scheduling, artificial intelligence and online apps to help patients find them rather than first turning to “Dr Google,” specialty care, urgent and emergency care services. While the predominance of fee-for-service payment in the United States has made this function easy to ignore or to declare “beyond my control,” value-based payment and measurement will make allowing patients to unnecessarily use urgent, emergent, or no health care services more obvious, more costly, and less excusable. As such, training residents to be measured and accountable for first-contact care must be a priority in new family medicine GME guideline creation.
Continuity
According to Starfield, continuity of care implied individual use of their primary or usual source of care over time for most health care needs.14 The Institute of Medicine labeled continuity a defining characteristic of primary care, and Francis Peabody’s famous “Care of the Patient” declares there to be an implicit contract between physician and patient in which the physician assumes ongoing responsibility for the patient, and frames the personal nature of medical care, in contrast to the dehumanizing nature of disjointed care.23,24 That continuity benefits health is born of the idea that knowledge, trust, and respect develop between the patient and provider over time, allowing for better interaction and communication. Of all the 4C’s, these effects have perhaps the strongest evidence base, as continuity of primary care has been repeatedly associated with a host of benefits, including greater satisfaction with care, lowering undesirable utilization and costs of care, and numerous disease outcomes.25-28 While continuity has been recently conceptualized as a physician-level measure, and one associated with lower costs and care utilization that is potentially applicable to faculty modeling and resident evaluation, it is also important for residents to learn how to deliver and enhance continuity in the context of team-based primary care.29 Training programs must impart to residents how best to engage medical assistants, nurse colleagues, behaviorists and other teammates in team approaches to continuous care, and how delivery design, technology, and handoffs can be executed in training and practice without sacrificing continuity and its benefits to patients.30 Trainees should exit residency with an understanding not only of the positive effects of continuity on outcomes, but also of the negative impacts of disruptions in continuity of care.31 Educators living in an age of increasing fragmentation, shift work, open-access scheduling, and care seeking through technology must understand how each of these pose threats to patient-to-clinician continuity and decide how to use educational policy levers to retain continuity in training.
Comprehensiveness
Among the 4C’s, comprehensiveness remains perhaps the most conceptually diffuse, though Starfield explained:
Comprehensiveness means that all problems in the population should be cared for in primary care (with short-term referral as needed), except those that are too unusual (generally a frequency of less than one or two per thousand in the population served) for the primary care practitioner or team to treat competently.14
Since Starfield, many in the primary care community have debated whether comprehensiveness refers to the breadth of the conditions a physician cares for, the depth of their ability to take care of each condition, care in various settings, or provision of a multitude of services.32 Despite debates over its measurement, we know that comprehensiveness is inherent to the delivery of whole-person care, and a feature that distinguishes primary care physicians from other specialists as well as nonphysician providers in both behaviors and overall costs. In addition to finding that countries with higher primary care scores also had higher quality and access to care at lower costs, Starfield declared the degree of comprehensiveness to be “the feature of primary care most salient in distinguishing [these] primary care-oriented countries from others.”33,34 As the subject-matter expert on patients themselves, it is perhaps concerning to witness decreases in many dimensions of comprehensiveness among family physicians, including declines in provision of inpatient, obstetric, pediatric and procedural care.35-38
Educators revising residency guidelines should be aware that comprehensiveness, like continuity, has been recently demonstrated as measurable at the physician level and associated with lower medical costs and hospitalizations.39 Also important is its association with lower levels of burnout,40 and the finding that intended scope of practice among family medicine graduates is broader than actual practice. These suggest the need not only for reform in training but also payment, as market forces shape environments unfavorable to graduates intending broadly-scoped practice. Reformers must consider the risks versus reward of revising training for an age when less fee-for-service and greater value-based capitated payments reward residency graduates with competency in delivering team-based, broadly-scoped practice.
Coordination
Coordination of care consists of leading, organizing, and integrating patient care across different locations, specialties, and phases of care, a virtue that Starfield found lacking even in high-performing health systems.14 As a result, there is less evidence linking primary care coordination with outcomes, but real opportunity for family medicine GME reform to empower residents to better demonstrate this functional use of new technology, tools, and team-based care. Evidence makes clear the critical importance of primary care’s coordinating role from a patient perspective, again suggesting opportunity to enhance guidelines for residency training.41 Federal reports have declared primary care’s coordination role to be integral to improving effectiveness, safety, and efficiency of care, noting that most health care systems are disjointed, with variable processes, unclear patient expectations with most referrals, and unfamiliarity hampering patients’ capacity to assess and choose among services available to improve their health.42 This concept also applies to coordination of decision-making together with patients and families, including the facilitation of their understanding of treatments or procedures to be performed. Educators should consider guidelines that promote and assess resident competencies not only in directing referrals, but also being present—synchronously or asynchronously, and regardless of their continued presence in inpatient and procedural settings—when key decisions are being made by or about their patients. Guidelines should be built on expectations that resident responsibilities extend far beyond the visit, require digital and communication tool literacy, and employ principles of self-study and continuous quality improvement in testing different approaches to excellent coordination of care.43
Over time, some have asked whether Starfield’s framework should be revisited, while others have suggested additional constructs that might also explain how primary care positively influences quadruple aim outcomes. In the following sections, we propose and elaborate on several such constructs.
Community Engagement
While foundational influences on a new discipline called family medicine such as Millis, Willard, and Folsom imagined a community-facing discipline at the epicenter of “Communities of Solution,” modern residents train in a health care paradigm increasingly asked to attend to the social determinants of health, to care not only for individual patients and families, but also panels and communities with a goal of achieving population health.44, 45 This demands the more explicit declaration of a “C” only tacitly addressed in Starfield’s model: Community engagement. If family medicine residents are to remain counterculture46 to modern, reductionist and institution-bound GME, it will be because of their embrace of Virchow’s notion that “Medicine is a social science, and politics…medicine on a large scale”; of generalist John Snow’s curiosity beyond the office in tracing community-level sources of disease47; of Sidney and Emily Kark’s revolutionary principles of community-oriented primary care in addressing with communities their own health problems48; of Paul Nutting’s guidance to structure one’s practice to take a community-oriented approach to primary care49; of John Grant’s “regionalization of health care” and embrace of community partners in achieving health. Each of these legendary generalists intuited and revealed the futility of attempting to address social determinants of health with clinic-based activity and training alone.50-52
While training alone will not fix systematic inattention to social determinants and inequity, new family medicine GME guidelines cannot permit residents to graduate without basic competencies in community-engaged practice. For starters, residents should be able to gauge the size of their patient panel better than practicing family physicians,53 to estimate the geographic area that they serve and the resources available to those living within it, and to understand simple tools available to guide population health assessment and interventions such as PHATE and HealthLandscape.54,55 They should be at least versed in health policy, health systems, advocacy, and multisectoral partnerships (public health, medical-legal, social services, housing among them) required to advance the needs of their patients and communities. These competencies must be framed widely to allow tailoring to local community needs and resident interests, and fortunately, there are a growing number of examples of community engagement in the primary care training environments for educators to draw upon and an increasing array of data, tools, and curriculum in this digital age.56-58 New requirements for community engagement should include not only competencies, but also involvement and service within the community and in the advancement of policies and community action favorable to health.
Patient-Centeredness
Conversations and considerable action over the last 2 decades have returned the patient to the center of US and global health system design and delivery. Most residents today train in patient-centered medical homes(PCMHs), theoretically places of rapid cycle innovation, built around patient-centered care concepts such as “nothing about me without me.”59,60 However, the practice of modern medicine remains fundamentally disease-centered, a construct served by value-based payments for mostly illness-based quality measures. A relational discipline by nature, family medicine training must resist these tendencies and continue to emphasize and build on a growing evidence base that supports excellent patient experience. In this regard, the residency clinic itself and its approach to care truly are the classroom. Guidelines should emphasize and embrace whole-person and team-based care that is centered around patient needs rather than physician convenience, including meeting the patient where they are with information when they need it. The overarching ideal of shared decision-making—understanding a patient for who they are as a person rather than a disease, identifying patient goals, and adjusting plan of care based on a patient’s understanding and capability—is also central to providing patient-centered care and demands attention in curriculum redesign.61 This requires adaptive competency in an array of apps, portals, and other means of virtual and asynchronous communication. It is essential that family medicine educators model, teach, and hold residents accountable to the shared principles of what it truly means to be patient-centered in a family, occupational, and community context, and how to serve patients’ “physical, emotional, psychological and spiritual well-being, as well as cultural, linguistic and social needs.”62 Residents should understand that this is achieved not merely through PCMH certification, yet be well versed in the lessons emerging from over a decade of innovative PCMH experiments in patient-centered primary care, a literature that continues to expand each year.63 Revisers of the Family Medicine Residency Review Committee guidelines can draw upon a growing array of single-program and collaborative approaches to building competencies in patient-centered care, but must also acknowledge patient-centeredness across all FM curricular requirements.64-66
Complexity
In addition to patient-centeredness, complexity has also emerged as the defining construct for primary care and its graduate medical education enterprise. As previously noted, our population is growing older, more obese, more diverse, and increasingly multimorbid, driving up both costs of care and mortality rates while our strategies for care grow increasingly fragmented, subspecialized, and siloed by disease and organ system. Family medicine represents an antidote to this tendency. As T.F. Fox famously noted, “the more complex medicine becomes, the stronger the reasons why everyone should have a personal doctor,”67 and it is no surprise that generalist disciplines deliver the most quantifiably complex care of all specialties when measured by quantity of inputs and outputs per encounter and their variability and diversity of work across the spectrum of care.68 New FM residency guidelines must walk a fine line in requiring residents to demonstrate minimum quanta of visits or care for certain disease categories (obstetrics, orthopedics, and so on), while also showing a more qualitative competency in addressing multimorbidity, caring for complex and undifferentiated illness and functioning in complex adaptive systems of care.69 This will require not only familiarity with disease-specific guidelines and tools, but the ability to synthesize and to adapt care to patient and population complexity, and understand and implement interventions that improve outcomes for patients with a growing array of multiple chronic conditions. 70
Sailing the 7C’s Is Not a Solo Voyage: 4T’s to Enable a Successful Journey
It is critical to note that burden of conveying and achieving competency as a purveyor of such multidimensional primary care cannot be borne by the individual educator and resident alone. Success will depend on many enabling factors in the residency built environment, among them training in teams, using tools, technology, and tailoring to local context. A built environment that models high-performing primary care, as defined by its attention to the 7C’s functions, with attention to these enablers and translation into measurable milestones, give opportunity for imprinting positive downstream behaviors and achieving desirable health system outcomes (Figure 1).
Teams
The age of the doctor-diva is long past, replaced with an awareness that physicians must respectfully operate within health care teams. Achievement of each of the 7C’s functions depends on such competency, which begins in the structure of a training-built environment in order to imprint positive team behaviors downstream. This requires curricular inclusion of skills in team-based care, leadership, and knowledge of the optimal deployment of a range of teammates in the delivery of comprehensive, complex, community engaged care. These should include not only certified health care teammates from other specialties, the fields of nursing, pharmacy, oral, behavioral, and allied health, but also lay partners bearing an array of labels: community health worker, patient navigator, family caregiver, and patients themselves. Optimally, training also includes lessons or experience in optimal engagement with data and information scientists, public health officials, and social services. Fortunately, many residents already perceive that they are well trained in team-based care, but much work remains to embody true team-based training and practice.71
Tools
It is impossible to imagine achieving continuous, coordinated, complex and community-engaged care absent familiarity with myriad tools now available to generalist physicians. Graduating without a demonstrated understanding of smartphone-based apps, tools for asynchronous care management, registries such as PRIME, population health implements, or measurement tools will condemn residents to burnout and failure in an evolving health system.72,73 Available tools for future physicians include not only technology as described in the following section, but separately information review in journals, patient handouts and information, peer education, networks of educators and contacts throughout subspecialties, and other implements that empower further resident and patient understanding of disease. Education on available information will provide residents and family physicians the tools to deliver improved patient- and community-centered care.
Technology
Technology is a tool of sufficient importance to warrant particular attention. Technology interconnects the health care world and the primary care environment in ways we couldn’t imagine in previous updates to training requirements. The COVID-19 pandemic has only heightened our dependence on previously underutilized telehealth, and many providers are now working on their third or fourth electronic medical record systems or portal for asynchronous communication with patients or other providers. While not all residents can undertake informatics fellowship training, curricular guidelines for their future success must include appropriate understanding and employment of advanced technology. As noted before, any hopes to improve care coordination begin with technologically competent generalists. Conversely, residents graduating without technologic competence adaptable to an increasing and ever shifting digital platform can hardly be expected to maintain professional wellness. Family medicine and its training enterprise must help to shape and direct how artificial intelligence and machine learning, genomics, and biometrics are used to address delivery processes and patient care, lest they see “solutions” not built for or tested in the primary care space continue to be imposed upon them by commercial entities and hospital systems. Such “solutions” likely to create more unintended costs, health care disparities, undesirable side effects, fragmentation, and burnout. Finally, overcoming trends when fewer and fewer patients are inclined to in-person visits and longitudinal relationships with primary care depends on our embrace of technology, and putting the right information in the hands of the patient when and where they want it. In short, ensuring technologically fluent generalists is an obligation for creators of new family medicine GME guidelines.
Tailoring
To deliver on the seven core features that explain the value of primary care, the family medicine resident must be trained to think and act the part of the tailor. Instead of being rigidly bound to an increasing array of evidence-based chronic care and preventive guidelines common to lower levels of clinician training, the primary care physician must adapt broad knowledge and tailor care to the complexity, needs, health care beliefs, and care-seeking behaviors of the whole patient. A contemporary iteration of Fox’s “personal physician,”67 this extension of patient-centeredness will require skills or competencies to be developed in many areas not traditional to disease- and organ-based education, among them cultural humility and awareness; how conceptualization of race in health care shapes decisions, trust, and outcomes; and the specific health needs related to differences in gender identity, health belief models and trust.74 Training the “tailor” would also enhance continuity and coordination, as some patients and populations will best be approached with a heavy dose of apps, telehealth, wearable technology, and asynchronous delivery, while others will continue to prefer and be best served by predominantly synchronous and visit-based care. At the community level, program directors must also train them to tailor their comprehensiveness of training to community needs and population demands, trained across a broad array of care and settings but also able to refine, enhance, or add new skills based on local or evolving demands. And once again, this likely requires explicit training and experience in engagement and advocacy, as well as data-driven understanding of panel size, community and service area characteristics unfamiliar to most current FPs.53,75 This concept of adapting to local need is of particular importance to the family medicine GME enterprise, whose small, widely distributed, and largely community-based training sites yield graduates particularly likely to practice within 100 miles of GME training.76
Implications for Residency Redesign and Evidence Gaps
Current GME standards, like current payment models and their resulting delivery system, are insufficient to ensure resident competency across the broad architecture we propose. It is also important to recognize that these 7C’s are hardly orthogonal, and occasionally competing; tradeoffs must be accommodated in Residency Review Committee guidelines that might otherwise push residents to increase first-contact care through open access and greater outpatient presence, but at the expense of more continuity visits and greater comprehensiveness through increased nonoutpatient training. That said, these core values can instead be seen as mutually synergistic; increasing first-contact care may provide opportunity for expansion of one’s patient panel and improvement in continuity, and the diversity of undifferentiated signs and symptoms experienced in first-contact care would provide training in comprehensive care. Seeking balance across the competing obligations and principles of generalist training is nothing new for the leaders of family medicine education. Their greater risk lies in a microscopic gaze or a reductionist approach to revising program requirements. To lose sight of core principles and a macroscopic view of the goals of training risks producing not the ideal definition of a contemporary family physician as recently declared by the discipline, but instead its foil (Figure 2). Others would point out that requirements have evolved considerably and positively in ways that already support the 7C’s and onto which further integration is easily imagined. For example, evaluation of first contact might already be found in the ACGME Milestones for Family Medicine “Ongoing Care of Patients With Undifferentiated Signs, Symptoms, or Health Concerns.”77 Perhaps further integration of first contact as a foundation of family medicine training could be achieved through definitional refinement rather than complete restructuring of evaluation.
Measurement skeptics will undoubtedly question whether current guidelines are consistent with attaining the ideals of Starfield’s Cs. They might point out that a hard minimum patient number doesn’t lead to greater competency as a provider of continuity and community health as other metrics might, for example, the ability to identify one’s patient panel or the number of patients that consider a resident their principal and trusted source of care. Some might advocate for broader Residency Review Committee guidelines for continuity, the specifics of which could be defined by residency programs tailored to the needs of their individual panels or community. For the numerically-inclined, could an alternative to 1,600+ total visits be a requirement for residents who have at least 200 patients, identifiable by patient and provider alike as a “continuity panel,” with whom the resident has a minimum number of visits. The current structure of continuity clinics as block rotations in many programs meets service demands, but not necessarily educational demands. Restructured longitudinal requirements for continuity clinics could support follow-up with the same resident as a primary care physician and assist with imprinting the importance and efficacy of longitudinal patient continuity on future family physicians. ACGME Milestones already exist that examine continuity relationships with patients, leaving one to hope that its measurement would require expansion, not invention.
Comprehensiveness remains a cornerstone of residency requirements in family medicine, but its dimensions must be reexamined in the face of scope declines, graduate challenges finding positions commensurate with training and intent, and opportunities for collective comprehensiveness delivered across teams and practices. Measurement of first-contact care warrants attention in curriculum redesign; time to third available appointment has been used to measure access previously; how should this indicator be adjusted as residencies incorporate telehealth? Coordination of care is listed among the new ACGME Resident Milestones, but revisions could consider its specifics, eg, whether to require participation in care coordinator rounds, review of social service work with hospital or clinic patients, or rotations that involve explicit care coordination or social work resembling practice management requirements. It will also be important to explicitly define and outline the differences between community engagement and coordination of care, as well as the advocacy and policy development activities already reflected in the new ACGME milestones. Patient-centeredness and complexity will face similar questions concerning best practices, feasibility and burden of measurement, and competing demands. In short, educators considering a 7C’s framework have many questions to consider, of which we capture only a sample in Table 1.
Using a simple 4C’s mnemonic, Barbara Starfield provided not only an explanatory framework for the benefits of investing in high-performing primary care, but also a guidepost if family medicine GME reform is to produce graduates relevant to the aims of public, payor, and policy stakeholders. Such relevance will require graduates to attend to the additional core primary care functions of community engagement, patient-centeredness, and complexity, and to competently harness the power of teams, tools, technology and tailoring to achieve a national quadruple aim. We hope that the family medicine residency review committee will find such a conceptual model useful in linking revised residency requirements to imprinted graduate behaviors capable of serving desired national outcomes for our expensive and underperforming health care system.
References
- Osborn R, Squires D, Doty MM, Sarnak DO, Schneider EC. In new survey of eleven countries, US adults still struggle with access to and affordability of health care. Health Aff (Millwood). 12 2016;35(12):2327-2336. doi:10.1377/hlthaff.2016.1088
- Anderson GF, Hussey P, Petrosyan V. It's still the prices, stupid: why the US spends so much on health care, and a tibute to Uwe Reinhardt. Health Aff (Millwood). 01 2019;38(1):87-95. doi:10.1377/hlthaff.2018.05144
- National Research Council; Institute of Medicine. US Health in International Perspective: Shorter Lives, Poorer Health. Woolf SH, Aron L, editors. Washington, DC: National Academies Press; 2013.
- Meslé F, Vallin J. Diverging trends in female old-age mortality: the United States and the Netherlands versus France and Japan. Popul Dev Rev. 2006;32(1):123-145. doi:10.1111/j.1728-4457.2006.00108.x
- National Research Council Panel on Understanding Divergent Trends in Longevity in High-Income Countries. Explaining Divergent Levels of Longevity in High-Income Countries. Crimmins EM, Preston SH, Cohen B, editors. Washington, DC: National Academies Press; 2011.
- World Health Organization. Declaration of Alma-Ata. USSR; September 1978. https://www.who.int/publications/almaata_declaration_en.pdf. Accessed April 19, 2021.
- Bazemore A, Wilkinson E, Petterson S, Green LA. Proportional erosion of the primary care physician workforce has continued since 2010. Am Fam Physician. 2019 Aug 15;100(4):211-212.
- Baillieu R, Kidd M, Phillips R, et al. The Primary Care Spend Model: a systems approach to measuring investment in primary care. BMJ Glob Health. 2019;4(4):e001601. doi:10.1136/bmjgh-2019-001601
- Martin S, Phillips RL Jr, Petterson S, Levin Z, Bazemore AW. Primary Care Spending in the United States, 2002-2016. JAMA Intern Med. 2020;180(7):1019-1020. doi:10.1001/jamainternmed.2020.1360
- Chen C, Petterson S, Phillips RL, Mullan F, Bazemore A, O’Donnell SD. Toward graduate medical education (GME) accountability: measuring the outcomes of GME institutions. Acad Med. 2013;88(9):1267-1280. doi:10.1097/ACM.0b013e31829a3ce9
- Council on Graduate Medical Education. Advancing Primary Care. Washington DC: Health Resources and Services Administration; December 2010.
- Hamel MB, Drazen JM, Epstein AM. The growth of hospitalists and the changing face of primary care. N Engl J Med. 2009;360(11):1141-1143. doi:10.1056/NEJMe0900796
- Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102-1112. doi:10.1056/NEJMsa0802381
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. doi:10.1111/j.1468-0009.2005.00409.x
- Future provision of medical services: Lord Dawson on the consultative council's report. Br Med J. 1920 Jun 12;1(3102):800-2.
- Liaw W, Jetty A, Petterson S, Bazemore A, Green L. Trends in the types of usual sources of care: a shift from people to places or nothing at all. Health Serv Res. 08 2018;53(4):2346-2367. doi:10.1111/1475-6773.12753
- Agency for Healthcare Research and Quality. 2004 National Healthcare Disparities Report. Rockville, MD: AHRQ; 2004.
- Forrest CB, Starfield B. The effect of first-contact care with primary care clinicians on ambulatory health care expenditures. J Fam Pract. 1996;43(1):40-48.
- Martin DP, Diehr P, Price KF, Richardson WC. Effect of a gatekeeper plan on health services use and charges: a randomized trial. Am J Public Health. 1989;79(12):1628-1632. doi:10.2105/AJPH.79.12.1628
- Kronman AC, Ash AS, Freund KM, Hanchate A, Emanuel EJ. Can primary care visits reduce hospital utilization among Medicare beneficiaries at the end of life? J Gen Intern Med. 2008;23(9):1330-1335. doi:10.1007/s11606-008-0638-5
- Hurley RE, Freund DA, Taylor DE. Emergency room use and primary care case management: evidence from four Medicaid demonstration programs. Am J Public Health. 1989;79(7):843-846. doi:10.2105/AJPH.79.7.843
- Starfield B. Primary care: balancing health needs, services and technology. New York: Oxford University Press; 1998:448.
- Peabody FW. The care of the patient. JAMA. 2015;313(18):1868. doi:10.1001/jama.2014.11744
- Institute of Medicine. Primary Care: America’s Health in a New Era. Washington, DC: The National Academies Press; 1996.
- McWhinney IR. Continuity of care in family practice. Part 2: implications of continuity. J Fam Pract. 1975;2(5):373-374.
- Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005 Mar-Apr 2005;3(2):159-66. doi:10.1370/afm.285
- Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004 Sep-Oct 2004;2(5):445-51. doi:10.1370/afm.91
- Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996;86(12):1742-1747. doi:10.2105/AJPH.86.12.1742
- Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL. Higher primary care physician continuity is associated with lower costs and hospitalizations. Ann Fam Med. 11 2018;16(6):492-497. doi:10.1370/afm.2308
- Wieland ML, Halvorsen AJ, Chaudhry R, Reed DA, McDonald FS, Thomas KG. An evaluation of continuity clinic redesign. J Gen Intern Med. 2013;28(12):1557. doi:10.1007/s11606-013-2613-z
- Sabety AH, Jena AB, Barnett ML. Changes in health care use and outcomes after turnover in rimary Cacre. JAMA Intern Med. 2020;(Nov). doi:10.1001/jamainternmed.2020.6288
- Grumbach K. To be or not to be comprehensive. Ann Fam Med. 2015;13(3):204-205. doi:10.1370/afm.1788
- Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60(3):201-218. doi:10.1016/S0168-8510(01)00208-1
- Starfield B. Pathways of influence on equity in health. Soc Sci Med. 2007;64(7):1355-1362. doi:10.1016/j.socscimed.2006.11.027
- Jetty A, Jabbarpour Y, Petterson S, Eden A, Bazemore A. The declining presence of family physicians in hospital-based care. J Am Board Fam Med. 2019 Nov-Dec 2019;32(6):771-772. doi:10.3122/jabfm.2019.06.190152
- Peterson LE, Nasim U, Madabhushi V. Declining endoscopic care by family physicians in both rural and urban areas. J Am Board Fam Med. 2019 Jul-Aug 2019;32(4):460-461. doi:10.3122/jabfm.2019.04.190064
- Barreto T, Peterson LE, Petterson S, Bazemore AW. Family physicians practicing high-volume obstetric care have recently dropped by one-half. Am Fam Physician. 06 2017;95(12):762.
- Bazemore AW, Makaroff LA, Puffer JC, et al. Declining numbers of family physicians are caring for children. J Am Board Fam Med. 2012 Mar-Apr 2012;25(2):139-40. doi:10.3122/jabfm.2012.02.110203
- Bazemore A, Petterson S, Peterson LE, Phillips RL. More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations. Ann Fam Med. 2015 May-Jun 2015;13(3):206-13. doi:10.1370/afm.1787
- Weidner AKH, Phillips RL, Fang B, Peterson LE. Burnout and scope of practice in new family physicians. Ann Fam Med. 05 2018;16(3):200-205. doi:10.1370/afm.2221
- Droz M, Senn N, Cohidon C. Communication, continuity and coordination of care are the most important patients' values for family medicine in a fee-for-services health system. BMC Fam Pract. 01 2019;20(1):19. doi:10.1186/s12875-018-0895-2
- AHRQ. Process quality indicators in Fam Med: results of an international comparison. Care coordination. Agency for Healthcare Research and Quality; 2016.
- Agency for Healthcare Research and Quality. All Papers, Briefs, and Other Resources on the PCMH. Rockville, MD: AHRQ. https://pcmh.ahrq.gov/page/papers-briefs-and-resources. Accessed April 19, 2021.
- Millis J. The Millis Commission report. GP. 1966 Dec;34(6):173-88 contd.
- Folsom Group. Communities of solution: the Folsom Report revisited. Ann Fam Med. 2012 May-Jun 2012;10(3):250-60. doi:10.1370/afm.1350
- Stephens GG. Family medicine as counterculture. Fam Med. 1998;30(9):629-636.
- Snow J. Cholera and the qater aupply in the south districts of London in 1854. J Public Health Sanit Rev. 1856;2(7):239-257.
- Kark JD, Abramson JH. Sidney Kark’s contributions to epidemiology and community medicine. Int J Epidemiol. 2003;32(5):882-884. doi:10.1093/ije/dyg291
- Nutting PA. Cmmunity-oriented primary care: an integrated model for practice, research, and education. Am J Prev Med. 1986 May-Jun 1986;2(3):140-7. doi:10.1016/S0749-3797(18)31339-4
- Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care—the growing importance of the community health center. N Engl J Med. 2010;362(22):2047-2050. doi:10.1056/NEJMp1003729
- Geiger HJ. The political future of social medicine: reflections on physicians as activists. Acad Med. 03 2017;92(3):282-284. doi:10.1097/ACM.0000000000001538
- Longlett SK, Kruse JE, Wesley RM. Community-oriented primary care: historical perspective. J Am Board Fam Pract. 2001 Jan-Feb 2001;14(1):54-63.
- Peterson LE, Cochrane A, Bazemore A, Baxley E, Phillips RL. Only one third of family physicians can estimate their patient panel size. J Am Board Fam Med. 2015 Mar-Apr 2015;28(2):173-4. doi:10.3122/jabfm.2015.02.140276
- Bazemore A, Carroza M, Turner S, Zhang X, Phillips R. Democratizing and Displaying Health Data: Introducing HealthLandscape.org. Jun. 2007. https://proceedings.esri.com/library/userconf/proc07/papers/papers/pap_1152.pdf. Accessed April 19, 2021
- Bambekova PG, Liaw W, Phillips RL, Bazemore A. Integrating community and clinical data to assess patient risks with a population health assessment engine (PHATE). J Am Board Fam Med. 2020 May-Jun 2020;33(3):463-467. doi:10.3122/jabfm.2020.03.190206
- National Committee for Quality Assurance. Social Determinants of Health Resource Guide. NCQA; 2020.
- Robert Graham Center. Community Oriented Primary Care (COPD) Curriculum. https://www.graham-center.org/rgc/maps-data-tools/tools/copc.html#:~:text=The%20Community%20Oriented%20Primary%20Care,COPC%20implementations%20in%20their%20communities. Accessed April 19, 2021.
- Bazemore AW, Cottrell EK, Gold R, et al. “Community vital signs”: incorporating geocoded social determinants into electronic records to promote patient and population health. J Am Med Inform Assoc. 2016;23(2):407-412. doi:10.1093/jamia/ocv088
- Davis K, Schoenbaum SC, Audet AMA. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953-957. doi:10.1111/j.1525-1497.2005.0178.x
- Berwick D. Escape Fire. New York: The Commonwealth Fund; 2002.
- Tonelli MR, Sullivan MD. Person-centred shared decision making. J Eval Clin Pract. 2019;25(6):1057-1062. doi:10.1111/jep.13260
- Primary Care Collaborative. Shared Principles of Primary Care. http://www.pcpcc.org/about/shared-principles. Accessed March 24, 2021.
- Kieber-Emmons AM, Miller WL. The Patient-Centered Medical Home (PCMH) Framing Typology for Understanding the Structure, Function, and Outcomes of PCMHs. J Am Board Fam Med. 2017 Jul-Aug 2017;30(4):472-479. doi:10.3122/jabfm.2017.04.170058
- Brown CM, Cronholm PF, Wright J, Warning WJ II, Radosh L, Gabbay R. A collaborative approach to achieving NCQA PCMH recognition within family medicine residency practices. Fam Med. 2014;46(1):19-27.
- Chandran R, Furey C, Goldberg A, Ashley D, Anandarajah G. Training family medicine residents to build and remodel a patient centered medical home in Rhode Island: a team based approach to PCMH education. R I Med J (2013). Apr 2014;98(4):35-41.
- Fernald D, Hall T, Montgomery L, et al. Colorado Residency PCMH Project: results rrom a 6-year transformation effort. Fam Med. 2019;51(7):578-586. doi:10.22454/FamMed.2019.928558
- Fox TF. The personal doctor and his relation to the hospital. Observations and reflections on some American experiments in general practice by groups. Lancet. 1960;1(7127):743-760. doi:10.1016/S0140-6736(60)90632-2
- Katerndahl D, Wood R, Jaén CR. Complexity of ambulatory care across disciplines. Healthc (Amst). 2015;3(2):89-96.
- Sturmberg JP, Martin CM, Katerndahl DA. Systems and complexity thinking in the general practice literature: an integrative, historical narrative review. Ann Fam Med. 2014 Jan-Feb 2014;12(1):66-74. doi:10.1370/afm.1593
- Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016;3:CD006560. doi:10.1002/14651858.CD006560.pub3
- Carney PA, Waller E, Dexter E, et al. Team training in family medicine residency programs and its impact on team-based practice post-graduation. Fam Med. 2017;49(5):346-352.
- Franko OI, Tirrell TF. Smartphone app use among medical providers in ACGME training programs. J Med Syst. 2012;36(5):3135-3139. doi:10.1007/s10916-011-9798-7
- Phillips R. The PRIME registry helps thousands of primary care clinicians liberate EHR data and prepare for MIPS. J Am Board Fam Med. 2017;30(4):559. doi:10.3122/jabfm.2017.04.170193
- Park ER, Betancourt JR, Miller E, et al. Internal medicine residents’ perceptions of cross-cultural training. Barriers, needs, and educational recommendations. J Gen Intern Med. 2006;21(5):476-480. doi:10.1111/j.1525-1497.2006.00430.x
- Rock RM, Liaw WR, Krist AH, et al. Clinicians' overestimation of their geographic service area. Ann Fam Med. 08 2019;17(Suppl 1):S63-S66. doi:10.1370/afm.2383
- Fagan EB, Gibbons C, Finnegan SC, et al. Family medicine graduate proximity to their site of training: policy options for improving the distribution of primary care access. Fam Med. 2015;47(2):124-130.
- The Accreditation Council for Graduate Medical Education. Family Medicine Milestones. Chicago: ACGME; 2019.





There are no comments for this article.