Background and Objectives: Primary care is associated with improved patient health and reductions in health disparities. Consequently, the demand for primary care physicians is increasing. To meet this demand, medical schools have employed strategies to graduate students interested in primary care careers, including medical education pathways—structured, longitudinal experiences that are explicitly separate from the main curricular scope of the undergraduate medical education experience. Our goal was to explore and identify common characteristics of medical education pathways that influence primary care specialty choice.
Methods: Using research articles identified through a scoping review, we performed a qualitative content analysis of studies that evaluated the impact of medical education pathways on medical students’ choices of primary care careers.
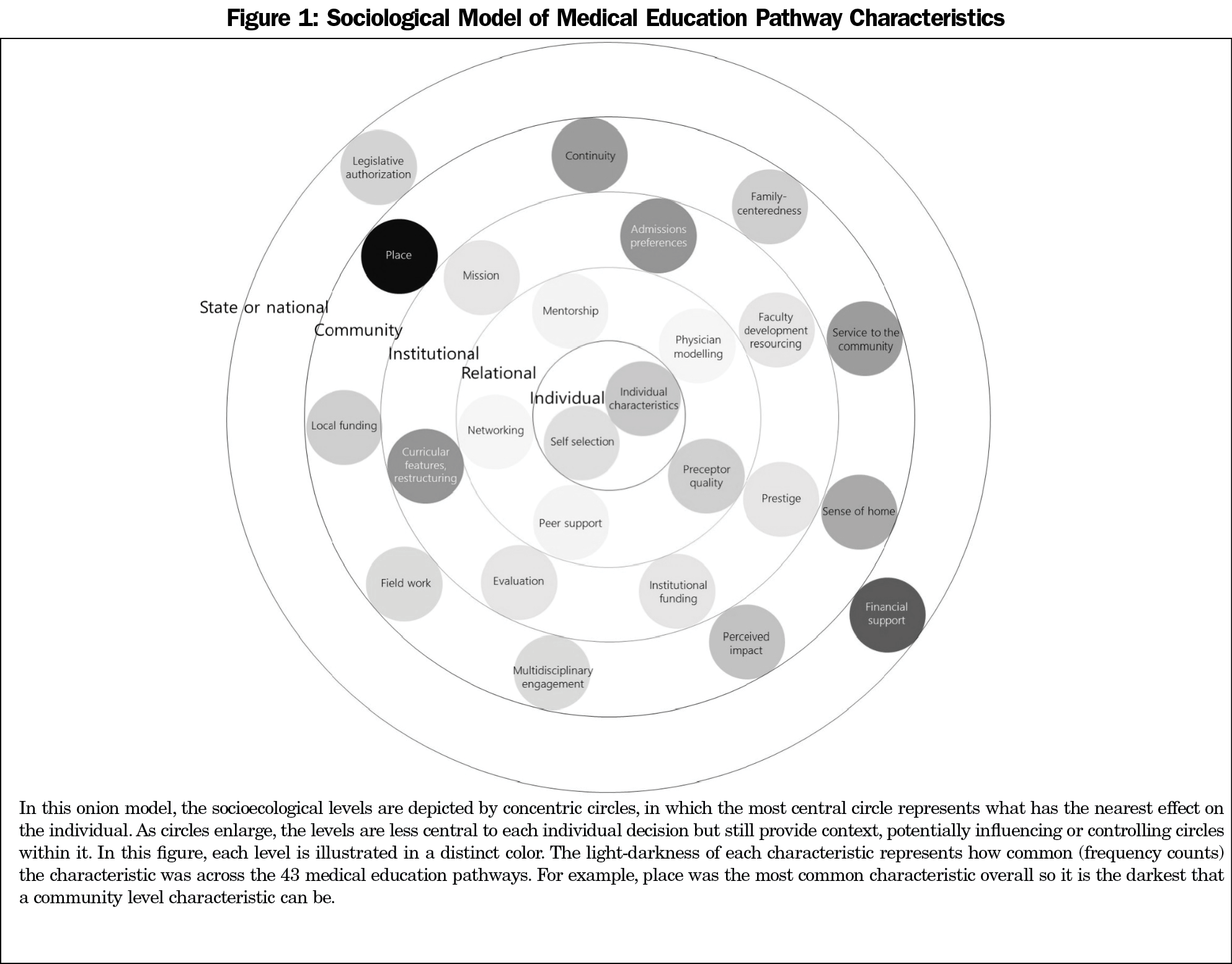
Results: Sixty-three papers described 43 medical education pathways; most studies used quantitative methods to describe outcomes. Program characteristics mapped onto five levels of an emerging socioecological model: state or national, community, institutional, relational, and individual.
Conclusions: Successful medical education pathway programs complement a medical school curriculum that supports a common goal, and demonstrate multiple levels of structural and institutional factors that develop community connectedness, relatedness, and longitudinal community engagement in students. Further work is needed to better understand how each of these levels influence career choice and to reassess how to measure and report medical education outcomes that will more accurately predict the student choice of primary care careers.
A primary care physician practices first-contact, comprehensive, and coordinated care within the context of long-term, person-focused relationships.1 The United States will require 52,000 additional primary care physicians by 2025 due to population growth and aging.2 In recognition of this need, the Family Medicine for America’s Health Workforce Education and Development Tactic Team created a shared aim to increase the percentage of US medical students choosing family medicine from 12% to 25% by the year 2030.3
Primary care specialty choice is a complex decision-making process influenced by student characteristics, medical school experience, lifestyle and financial considerations, perceived specialty characteristics, and the health care environment.4 Student characteristics consistently associated with primary care choice are female gender, rural background, planned rural practice, and lower income expectations.5-12 Medical schools can also influence specialty choice. Notably, a school’s primary care culture influences student intention to pursue a career in primary care.13 Medical schools have made repeated attempts to motivate primary care choice. Interventions associated with primary care choice are a required third-year primary care clerkship, longer family medicine clerkship, and longitudinal primary care experience.14 Longitudinal programs, or primary care tracks, are one mechanism medical schools have implemented to increase recruitment into primary care.15 The medical education pathway is a structured, longitudinal experience that exists separately from the main curricular scope of the undergraduate medical education experience and exposes the student to the continuity of primary care. During this extended time, students can project themselves into this hypothetical career and role.16
The goal of our study was to identify the shared characteristics of medical education pathway interventions that have successfully increased the number of medical students choosing primary care.
Our study is a qualitative content analysis17 of a subset of literature identified in a larger scoping review of interventions that influence primary care career choice.18 The subset—studies that investigate the implementation and evaluation of medical education pathways (MEPs) on primary care career choice—was identified by the authors in collaboration with the senior investigators on the scoping review. The authors defined MEPs as structured, longitudinal experiences that are explicitly separate from the main curricular scope of the undergraduate medical education experience. Students in MEPs follow a completely different path of study from their medical school peers for a substantial portion of their education. Inclusion criteria were research articles that evaluate the impact of medical education pathways on medical students’ choices of primary care careers. Studies from Australia, Canada, New Zealand, and the United States were included. For the outcome of interest, we included only MEPs designed to increase medical student choice of primary care, including programs with an even more specific focus, such as those designed to increase student choice of rural practice. We excluded articles that focused on graduate medical education or were not research.
To ensure the subset of articles identified through the scoping review was a complete representation of the existing literature, a medical librarian conducted an additional search with our keywords of interest (medical education pathway and training tracks) in July 2020. That search detected 10 additional articles that met inclusion criteria.
Our analysis applied a grounded theory method to the data.19 In the quality rating stage of the scoping review, the first (C.J.W.L.) and second (E.G.) author immersed themselves in the documents. Throughout this process, we met in person three times to discuss the papers. Guided by a quality rating rubric,20 these discussions focused on each paper’s purpose, theoretical framework, methods, context, and findings. During this process, we identified which papers described MEPs that successfully increased student choice and which did not (as determined and described by the authors of each study).
During the quality review process, we recognized that MEP characteristics could map onto a socioecological model21 that would provide a framework for understanding the multifaceted and interactive effects of personal and environmental factors that influence individual behavior.
After the full quality review, authors C.J.W.L. and E.G. first separately coded half the documents. The unit of analysis was each individual characteristic of a medical education pathway. When multiple papers described the same MEP, we coded all papers to ensure that we captured characteristics that could have been described differently or uniquely across time and publication for one program. Characteristics were identified if they were described in any section of a paper (introduction, methods, results, or discussion).
We then separately categorized all characteristics by model level, labeling the characteristic by MEP and (un)success. Aligning with the qualitative approach of this study, characteristics were not weighted by importance or frequency. We then met two times in person to map all coded characteristics onto the five levels of the model. In this process, we discussed all characteristics’ placement to consensus. As characteristics were mapped onto the model, we grouped them into categories. Through this process, we sought to confirm these categories by reviewing the analysis conducted on the segmented text while also comparing and relating the codes to each other, referred to as axial coding, to define each category’s characteristics.
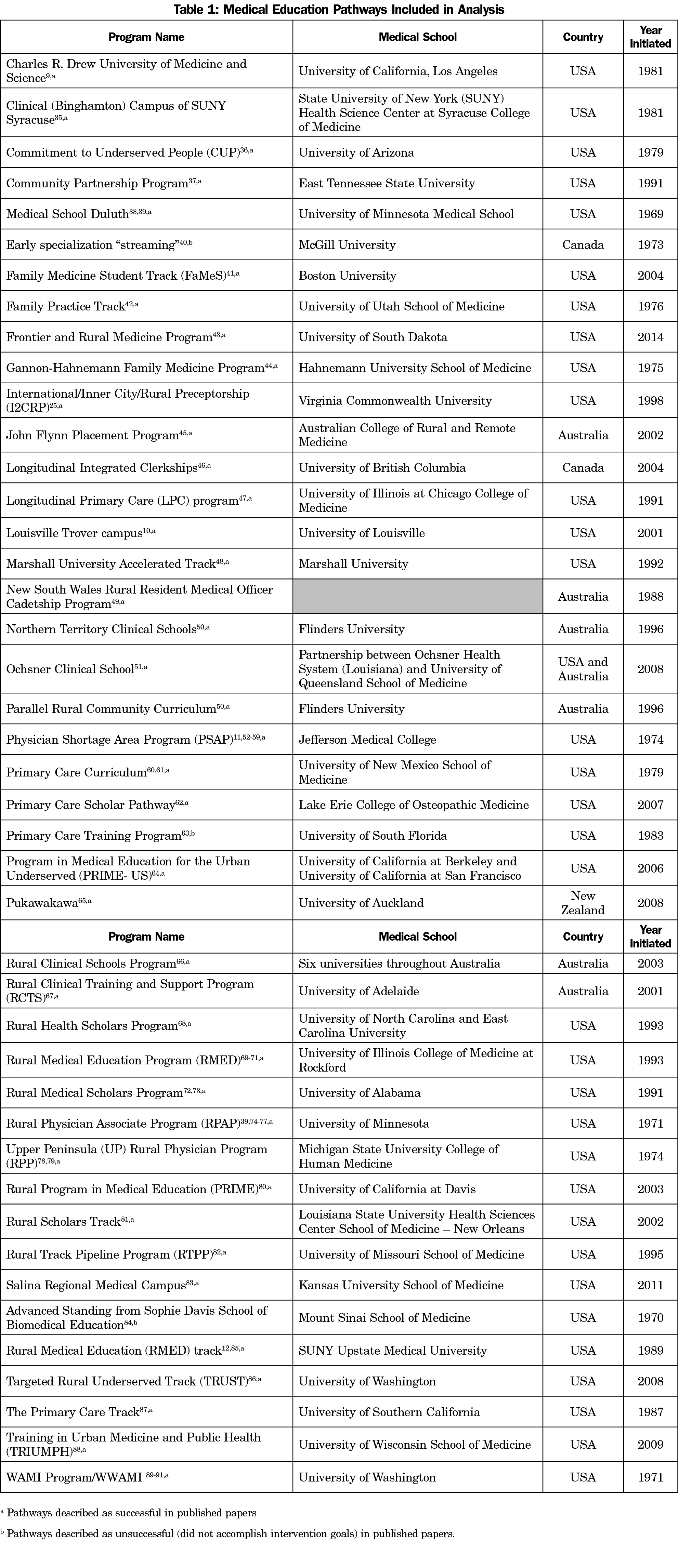
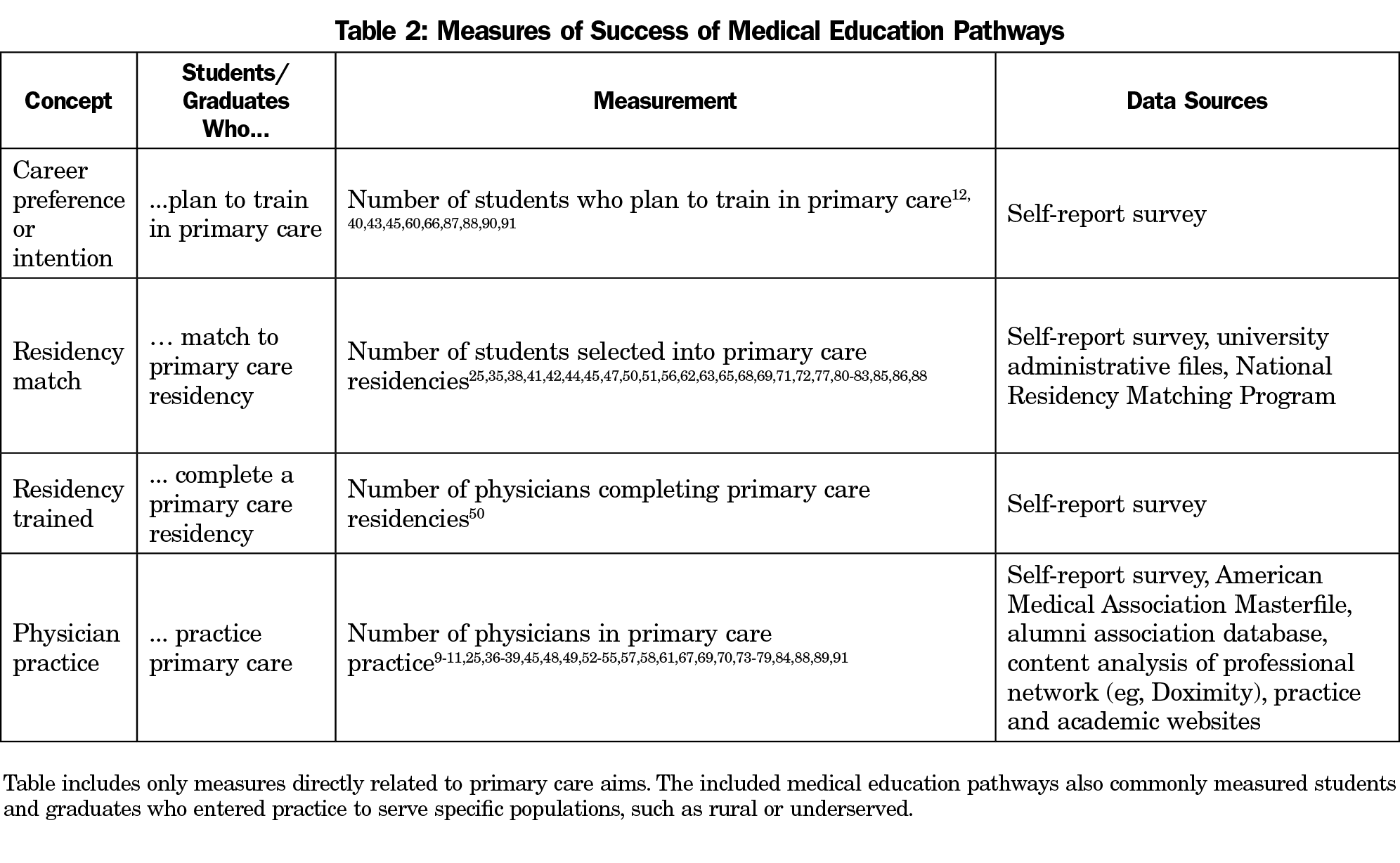
In this data set, 63 papers described 43 medical education pathways that were initiated between 1969 and 2014 (Table 1). Almost all MEPs were associated with allopathic medical schools, with only one osteopathic MEP. Of these pathways, authors described 40 MEPs as successful, whereas three MEPs did not accomplish their goals. Table 2 presents how success was operationalized in these programs. The majority (n=55, 87.3%) of studies focused on quantitative data to examine program outcomes (one study was qualitative only; seven described multimethod or mixed-methods approaches).
The coding process identified 206 characteristics of MEPs, within 31 categories across five levels of influence. Figure 1 presents the socioecological model of medical education pathway characteristics.
Model Mapping: State or National Level
At the state or national level, MEP characteristics mapped onto two categories: financial support and legislative authorization. Financial support was provided through a variety of mechanisms. Some MEPs funneled funding to individuals through state-funded scholarships, stipends, or community preceptor stipends. Others used state or national funding (federal or private foundation grants) to support the MEP more broadly. Separate from financial resources, some MEPs were created in response to a direct mandate from state legislatures.
Model Mapping: Community Level
The community level encompassed two different functions of community: community practice and community connectedness. MEP characteristics mapped onto three community practice categories: place, continuity, and family-centeredness. Place describes the location of practice, where students learn in community practices. Papers often described these settings as rural, underserved, or small communities. Place enabled students to learn in context. Continuity was also a repeated characteristic. Some MEPs facilitated repeated exposure to communities, either through longitudinal, episodic exposure or through a single, extended (4 months or longer) exposure to clinical practice in the community. This continuity can provide students with the opportunity to experience patient continuity. Within the community practice, some pathways engaged students in family-centered practice, through which they provided clinical care for multiple members of a family.
MEP characteristics mapped onto six community connectedness categories: local funding, service to the community, field work, multidisciplinary engagement, sense of home, and perceived impact. Four of these categories were action-oriented. First, some MEPs received local funding that provided stipends to students and/or preceptors. Second, some MEPs required a community service project that included both community-informed clinical questions and methods and resulted in community-oriented answers and interventions. Third, some MEPs pushed students to engage in field work outside clinic walls, such as health fairs or agricultural field trips. Fourth, some MEPs provided an opportunity for students to see multidisciplinary care. For example, students engaged in care collaborations with dentistry, nursing homes, and clergy members.
The fifth and sixth characteristics of community connectedness described MEP characteristics that were designed to affect student perceptions. When MEPs enabled students to live in communities, they developed a sense of home. These MEPs were generally designed for students to live in communities for more than 1 year of their education. Some rotations were long enough that students relocated with their families to live in the community. Lastly, some MEPs enabled students to fully immerse in the community, which enabled them to recognize how clinical practice was impacting the local population. Some MEPs sometimes emphasized impact on specific populations, such as underserved populations.
Model Mapping: Institutional Level
At the institutional level, MEP characteristics mapped onto eight categories: mission, prestige, admissions preferences, student funding, curricular features and restructuring, evaluation, and faculty development resourcing. Institutional-level characteristics describe medical school communication, values, policies, and actions.
Communicatively, the medical school’s stated mission was cited as important to the development and continuation of many MEPs. Similarly, how a medical school valued primary care (prestige) was often an important characteristic. This value was connected to an MEP’s credibility and students’ overall perception of the value of the MEP within the medical school. Policy primarily centered on a program’s admissions preferences, which were connected to evidence-based applicant characteristics. Admissions preferences were categorized as institutional-level characteristics when the pathway included a defined admissions policy (in contrast to individual-level student characteristics described in the next section).
Institutions enacted four types of actions as part of MEPs. First, some medical schools provided student funding through scholarships, tuition exemptions, and financial aid. Second, some medical schools designed curricula or restructured curriculum scope and sequence. Curricular components were widely variable, including broader content such as behavioral medicine, telemedicine, or patient advocacy. Most modifications to the standard medical school curriculum were connected to timing and pedagogical framework. MEPs often introduced students to clinical topics earlier and more consistently across their education. Some also introduced problem-based and self-directed learning models. Third, some MEPs provided faculty development in the regions and communities where students were completing clinical rotations, away from the academic medical center. Fourth, medical schools evaluated the MEPs, measuring their success against stated objectives.
Model Mapping: Relational Level
At the relational level, MEP characteristics mapped onto five categories: mentorship, networking, physician modelling, peer support, and preceptor quality (personal, continuity, trusted). At this level, interpersonal relationships were key features of MEPs. Programs actively sought ways to foster relationships between students and practicing primary care physicians.
Four categories at this level described the purpose of the relationships: modelling, mentorship, networking, and peer support. Some schools recognized that students needed to see physicians modelling the life of a primary care physician. Modeling did not solely focus on clinical practice. Physicians can model leadership, work-life balance, team collaboration, and teaching. In addition to modelling, some MEPs programmed intentional mentorship for students. Mentorship was available from both academic and community physicians. The third purpose, networking, described not only networking for students with primary care physicians but also with other students. This inclusion of peers was extended in the peer support category. Some MEPs provided peer teaching, peer support groups (both before matriculation and throughout medical school), and/or peer social events, which included student family members.
In addition to these purpose-oriented characteristics, preceptor quality was a repeated characteristic at the relational level. Some schools focused on the critical role of the clinical preceptor in medical education and how this role influences student choice. Papers described three broad characteristics of preceptor quality: personal, continuous, and trustworthiness. MEPs sought preceptors who would work one on one with students. This relationship was amplified when preceptors could work with students across clinical years, creating longitudinal relationships with students. Trustworthiness not only described how a student could trust the preceptor but also that the MEP could trust the preceptor. This trustworthiness was sometimes derived from previous relationships. Two common mechanisms were recruiting medical school alumni to act as preceptors or recruiting preceptors who practiced in the student’s hometown where the student was clinically embedded.
Model Mapping: Individual Level
Characteristics at the individual level are not characteristics of the MEPs themselves, but characteristics of students that MEPs identified as evidence-based populations of interest to recruit. In this sample of papers, MEPs described two categories: self-selection and student characteristics. First, most MEPs recognized that students must self-select into pathways for them to effectively reinforce students’ career interests. Second, four types of students were often recruited because they were likely to choose primary care: students from rural areas, women, students older than 31 years, and racial and ethnic minorities.
This qualitative content analysis demonstrates that medical education pathways can increase primary care specialty choice. The emerging socioecological model of medical education pathway characteristics describes the complex landscape of medical education pathways and provides a framework for medical schools to consider as they develop and refine efforts to increase primary care specialty choice.
Results echo previous findings of a 1995 meta-analysis identifying practice rotation factors, relational factors, and individual factors associated with primary care career choice.8 However, our results demonstrate that we cannot select or leverage single proven characteristics from this list. What differentiated successful MEPs from the three unsuccessful MEPs was not individual characteristics but a complex approach to specialty choice that crossed levels. We must design pathways that recognize both personal and environmental influences on individual behavior. Rabinowitz made a similar argument when he outlined the five essential elements of rural tracks (recruiting, training at site, regional teachers, financial and relational support, and evaluation).11 All five of the elements are essential: they are not a menu from which to pick and choose what is existing or convenient. Zuckerman similarly specified three factors of specialty choice: sociodemographics, personality, and structural/institutional factors.22 Our results describe multiple levels of these structural/institutional factors in successful MEPs.
The model of multilevel influence also proposes a nuanced, but important difference in how students are introduced to and engaged in communities. Our findings demonstrate that medical students need to not only experience community practice but also community connectedness. Community-oriented care is care in which clinicians aim to be aware of, and oriented to, the health needs of a community.23 A community-engaged clinician lives in and understands the community of patients; this engagement enables clinicians to understand the context of community factors such as food insecurity, housing instability, and limited income. By immersing students in community-oriented care, MEPs offer students a realistic preview24 of primary care that showcases the power of community orientation in affecting patient and family outcomes.
In their application of self-determination theory, Park and colleagues explain that student perception of relatedness—feeling like a member of a community—increased their motivation to learn.25 This may create a virtuous cycle of immersion, relatedness, motivation, immersion, and so forth. By developing pathway models that support these virtues, schools can use resources to facilitate a sustained commitment to primary care26 that feeds that cycle.
This longitudinal engagement also introduces students to the principle of continuity of care.27,28 First described by Hennen,29 continuity of care incorporates four domains: longitudinal (the use of repeated patient observations over time as a diagnostic and management tool); informational (the availability of accurate information from one health care encounter to another); geographic (care of the patient in a variety of locations); and interpersonal (the clinician-patient relationship). Since its first description, the concept has expanded to include the dimensions of interdisciplinary (the management of several body systems and diseases at the same time) and family (knowledge about and understanding of the patient and his or her family) continuity of care.30 For a student to experience and understand these domains of continuity, the MEP must provide longitudinal community engagement.
Limitations
This study relied on each author’s description of the medical education pathway and its evidence of success. It is possible that some existing characteristics were not described or were misrepresented.
Notably, this study provides evidence from allopathic (MD) programs: only one osteopathic (DO) program emerged in the sample of 43 programs. Compared to allopathic school graduates, a larger number of osteopathic school graduates entered primary care specialties.31 The recent Osteopathic Profession Report from 2019 shows that 56.9% of all osteopathic physicians practice primary care.32 In both American Osteopathic Association and Accreditation Council for Graduate Medical Education programs, osteopathic resident physicians are in primary care specialties at higher rates (40.6% of all DO residents and 34.8% MD residents).31 Based on our present study, it is not known whether osteopathic schools create fewer pathway programs or publish fewer outcome studies of those programs.
Future Research
Although this narrative review includes qualitative, quantitative, and multi- or mixed-methods approaches, the evidence is overwhelmingly quantitative. To develop a rich understanding of how each of these levels influence student choice, more qualitative and mixed-methods work, both observational and interventional, is needed. Crump recommended larger-scale interviews or focus groups “to provide insight into the variance not yet explained by traditional demographic measures (nature) or educational exposure (nurture).”10 We also need to reassess how we measure workforce targets. Many of these programs used student intention or residency match numbers as surrogates for primary care workforce outcomes. Studies show that residency match overpredicts the size of our primary care workforce.33 We need clearer, more valid measures, such as the “rural workforce year,”34 to understand the success of workforce development strategies such as MEPs.
Acknowledgments
The authors thank Molly Polverento, Iris Kovar-Gough, Shelby Walker, and Virginia Young for their substantial contributions to the literature search, literature retrieval, literature review, and data organization.
Funding Statement: This work is supported by a grant from the American Board of Family Medicine Foundation. This project was partially supported by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) under grant number D54HP23297, Academic Administrative Units.
Disclaimer: This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by Health Resources and Services Administration, Department of Health and Human Services, US Air Force, Department of Defense, or the US Government.
References
- Starfield B, Oliver T. Primary care in the United States and its precarious future. Health Soc Care Community. 1999;7(5):315-323. doi:10.1046/j.1365-2524.1999.00193.x
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. doi:10.1370/afm.1431
- Kelly C, Coutinho AJ, Goldgar C, et al. Collaborating to achieve the optimal family medicine workforce. Fam Med. 2019;51(2):149-158. doi:10.22454/FamMed.2019.926312
- Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85(10)(suppl):S81-S88. doi:10.1097/ACM.0b013e3181ed4bae
- McDonald C, Henderson A, Barlow P, Keith J. Assessing factors for choosing a primary care specialty in medical students: a longitudinal study. Med Educ Online. 2021;26(1):1890901. doi:10.1080/10872981.2021.1890901
- Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997-2006. Acad Med. 2010;85(6):947-958. doi:10.1097/ACM.0b013e3181dbe77d
- Teitelbaum HS, Ehrlich N, Travis L. Factors affecting specialty choice among osteopathic medical students. Acad Med. 2009;84(6):718-723. doi:10.1097/ACM.0b013e3181a43c60
- Bland CJ, Meurer LN, Maldonado G. Determinants of primary care specialty choice: a non-statistical meta-analysis of the literature. Acad Med. 1995;70(7):620-641. doi:10.1097/00001888-199507000-00013
- Barnhart J, Shekelle P, Lewis C. The effect of a medical school’s admission and curriculum policies on increasing the number of physicians in primary care specialties. Acad Med. 1996;71(3):293-295. doi:10.1097/00001888-199603000-00025
- Crump WJ, Fricker RS, Ziegler CH, Wiegman DL. Increasing the rural physician workforce: A Potential Role for Small Rural Medical School Campuses. J Rural Health. 2016;32(3):254-259. doi:10.1111/jrh.12156
- Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA. 2001;286(9):1041-1048. doi:10.1001/jama.286.9.1041
- Roseamelia C, Greenwald JL, Bush T, Pratte M, Wilcox J, Morley CP. A qualitative study of medical students in a rural track: views on eventual rural practice. Fam Med. 2014;46(4):259-266.
- Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med. 2013;88(12):1919-1926. doi:10.1097/ACM.0000000000000038
- Pfarrwaller E, Sommer J, Chung C, et al. Impact of interventions to increase the proportion of medical students choosing a primary care career: a systematic review. J Gen Intern Med. 2015;30(9):1349-1358. doi:10.1007/s11606-015-3372-9
- Williams MP, Agana DF, Rooks BJ, et al. Primary care tracks in medical schools. PRiMER Peer-Rev Rep Med Educ Res. 2019;3:3. doi:10.22454/PRiMER.2019.799272
- Burack JH, Irby DM, Carline JD, Ambrozy DM, Ellsbury KE, Stritter FT. A study of medical students’ specialty-choice pathways: trying on possible selves. Acad Med. 1997;72(6):534-541. doi:10.1097/00001888-199706000-00021
- Lune H, Berg BL. Qualitative research methods for the social sciences. 9th ed. Boston: Pearson; 2018.
- Phillips J. Systematic Review of Medical School Interventions to Promote Primary Care Specialty Choice. In progress.
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage; 1998.
- Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18(4):746-752. doi:10.1111/j.1365-2753.2011.01662.x
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. Health behavior and health education: Theory, research, and practice. 2008;4:465-485.
- Zuckerman HS. Structural factors as determinants of career patterns in medicine. J Med Educ. 1978;53(6):453-463. doi:10.1097/00001888-197806000-00001
- Stevens GD, Shi L, Vane C, Nie X, Peters AL. Primary care medical home experience and health-related quality of life among adult medicaid patients with type 2 diabetes. J Gen Intern Med. 2015;30(2):161-168. doi:10.1007/s11606-014-3033-4
- Hom PW, Griffeth RW, Palich LE, Bracker JS. An exploratory investigation into theoretical mechanisms underlying realistic job previews. Person Psychol. 1998;51(2):421-451. doi:10.1111/j.1744-6570.1998.tb00732.x
- Park Y, Ryan MH, Santen SA, Sabo R, Blondino C, Magee ML. Nurturing the student, sustaining the mission: 20 years of the International/Inner-City/Rural Preceptorship Program. Fam Med. 2019;51(10):823-829. doi:10.22454/FamMed.2019.358223
- Campbell KM, Infante Linares JL, Tumin D, Faison K, Heath MN. The role of North Carolina medical schools in producing primary care physicians for the state. J Prim Care Community Health. 2020;11:2150132720924263. doi:10.1177/2150132720924263
- Wall EM. Continuity of care and family medicine: definition, determinants, and relationship to outcome. J Fam Pract. 1981;13(5):655-664.
- Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1(3):134-143. doi:10.1370/afm.23
- Hennen BK. Continuity of care in family practice. Part 1: dimensions of continuity. J Fam Pract. 1975;2(5):371-372.
- Kerr JR, Schultz K, Delva D. Two new aspects of continuity of care. Can Fam Physician. 2012;58(8):e442-e449.
- Jolly P, Lischka T, Sondheimer H. Numbers of MD and DO graduates in graduate medical education programs accredited by the Accreditation Council for Graduate Medical Education and the American Osteopathic Association. Acad Med. 2015;90(7):970-974. doi:10.1097/ACM.0000000000000649
- OMP 2019: Osteopathic Medical Profession Report. Chicago, IL: American Osteopathic Association; 2020.
- Deutchman M, Macaluso F, Chao J, et al. Contributions of US medical schools to primary care (2003-2014): determining and predicting who really goes into primary care. Fam Med. 2020;52(7):483-490. doi:10.22454/FamMed.2020.785068
- Meyers P, Wilkinson E, Petterson S, et al. Rural workforce years: quantifying the rural workforce contribution of family medicine residency graduates. J Grad Med Educ. 2020;12(6):717-726. doi:10.4300/JGME-D-20-00122.1
- Erney SL, Allen DL, Siska KF. Effect of a year-long primary care clerkship on graduates’ selection of family practice residencies. Acad Med. 1991;66(4):234-236. doi:10.1097/00001888-199104000-00014
- Campos-Outcalt D, Chang S, Pust R, Johnson L. Commitment to the underserved: evaluating the effect of an extracurricular medical student program on career choice. Teach Learn Med. 1997;9(4):276-281. doi:10.1207/s15328015tlm0904_6
- Florence JA, Goodrow B, Wachs J, Grover S, Olive KE. Rural health professions education at East Tennessee State University: survey of graduates from the first decade of the community partnership program. J Rural Health. 2007;23(1):77-83. doi:10.1111/j.1748-0361.2006.00071.x
- Fuglestad A, Prunuske J, Regal R, Hunter C, Boulger J, Prunuske A. Rural family medicine outcomes at the University of Minnesota Medical School Duluth. Fam Med. 2017;49(5):388-393.
- Zink T, Center B, Finstad D, et al. Efforts to graduate more primary care physicians and physicians who will practice in rural areas: examining outcomes from the University of Minnesota-Duluth and the Rural Physician Associate program. Acad Med. 2010;85(4):599-604. doi:10.1097/ACM.0b013e3181d2b537
- Dauphinee WD, Patel VL. Early career choice: an unsuccessful program. J Med Educ. 1983;58(9):695-702.
- Wilkinson JE, Hoffman M, Pierce E, Wiecha J. FaMeS: an innovative pipeline program to foster student interest in family medicine. Fam Med. 2010;42(1):28-34.
- Harris DL, Coleman M, Mallea M. Impact of participation in a family practice track program on student career decisions. J Med Educ. 1982;57(8):609-614. doi:10.1097/00001888-198208000-00005
- Jensen B, Anderson SM, Simanton E. The impact of a rural training track on medical students specialty choice. S D Med. 2017;70(6):263-265.
- Bloom FJ, Vatavuk MK, Kaliszewski SE. Evaluation of Gannon-Hahnemann Program to provide family physicians for underserved area. J Med Educ. 1988;63(1):7-10. doi:10.1097/00001888-198801000-00002
- Young L, Kent L, Walters L. The John Flynn Placement Program: evidence for repeated rural exposure for medical students. Aust J Rural Health. 2011;19(3):147-153. doi:10.1111/j.1440-1584.2011.01201.x
- Cuncic C, Regehr G, Frost H, Bates J. It’s all about relationships : A qualitative study of family physicians’ teaching experiences in rural longitudinal clerkships. Perspect Med Educ. 2018;7(2):100-109. doi:10.1007/s40037-018-0416-y
- Tekian A, Foley R. Initial results of a longitudinal primary care program’s influence on specialty choice. Teach Learn Med. 1997;9(2):151-154. doi:10.1080/10401339709539830
- Petrany SM, Crespo R. The accelerated residency program: the Marshall University family practice 9-year experience. Fam Med. 2002;34(9):669-672.
- Lewis MJ, Ellis R, Adusumilli SK, Cameron I. Twenty-five years on: outcomes of a longitudinal evaluation of the NSW Rural Resident Medical Officer Cadetship Program. Rural Remote Health. 2016;16(3):3846. doi:10.22605/RRH3846
- Worley P, Martin A, Prideaux D, Woodman R, Worley E, Lowe M. Vocational career paths of graduate entry medical students at Flinders University: a comparison of rural, remote and tertiary tracks. Med J Aust. 2008;188(3):177-178. doi:10.5694/j.1326-5377.2008.tb01567.x
- Deichmann RE, Alder L, Seoane L, Pinsky WW, Denton GD. Initial Match rates of an innovative international partnership: the Ochsner Clinical School Experience. Ochsner J. 2016;16(1):27-31.
- Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. Increasing the supply of rural family physicians: recent outcomes from Jefferson Medical College’s Physician Shortage Area Program (PSAP). Acad Med. 2011;86(2):264-269. doi:10.1097/ACM.0b013e31820469d6
- Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. Increasing the supply of women physicians in rural areas: outcomes of a medical school rural program. J Am Board Fam Med. 2011;24(6):740-744. doi:10.3122/jabfm.2011.06.110037
- Rabinowitz HK, Petterson S, Boulger JG, et al. Medical school rural programs: a comparison with international medical graduates in addressing state-level rural family physician and primary care supply. Acad Med. 2012;87(4):488-492. doi:10.1097/ACM.0b013e3182488b19
- Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA. 1999;281(3):255-260. doi:10.1001/jama.281.3.255
- Rabinowitz HK. A program to recruit and educate medical students to practice family medicine in underserved areas. JAMA. 1983;249(8):1038-1041. doi:10.1001/jama.1983.03330320036028
- Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. Retention of rural family physicians after 20-25 years: outcomes of a comprehensive medical school rural program. J Am Board Fam Med. 2013;26(1):24-27. doi:10.3122/jabfm.2013.01.120122
- Rabinowitz HK, Paynter NP. The role of the medical school in rural graduate medical education: pipeline or control valve? J Rural Health. 2000;16(3):249-253. doi:10.1111/j.1748-0361.2000.tb00468.x
- Rabinowitz HK, Diamond JJ, Markham FW, Rabinowitz C. Long-term retention of graduates from a program to increase the supply of rural family physicians. Acad Med. 2005;80(8):728-732. doi:10.1097/00001888-200508000-00004
- Kaufman A, Mennin S, Waterman R, et al. The New Mexico experiment: educational innovation and institutional change. Acad Med. 1989;64(6):285-294. doi:10.1097/00001888-198906000-00001
- Mennin SP, Kalishman S, Friedman M, Pathak D, Snyder J. A survey of graduates in practice from the University of New Mexico’s conventional and community-oriented, problem-based tracks. Acad Med. 1996;71(10):1079-1089. doi:10.1097/00001888-199610000-00015
- Raymond RM, Madden MM, Ferretti SM, Ferretti JM, Ortoski RA. Preliminary outcomes of the Lake Erie College of Osteopathic Medicine’s 3-year Primary Care Scholar Pathway in osteopathic predoctoral education. J Am Osteopath Assoc. 2014;114(4):238-241.
- Herold AH, Woodard LJ, Pamies RJ, Roetzheim RG, Van Durme DJ, Micceri T. Influence of longitudinal primary care training on medical students’ specialty choices. Acad Med. 1993;68(4):281-284. doi:10.1097/00001888-199304000-00015
- Sokal-Gutierrez K, Ivey SL, Garcia RM, Azzam A. Evaluation of the program in medical education for the urban underserved (PRIME-US) at the UC Berkeley-UCSF Joint Medical Program (JMP): the first 4 years. Teach Learn Med. 2015;27(2):189-196. doi:10.1080/10401334.2015.1011650
- Matthews C, Bagg W, Yielder J, Mogol V, Poole P. Does Pukawakawa (the regional-rural programme at the University of Auckland) influence workforce choice? N Z Med J. 2015;128(1409):35-43.
- Walker JH, Dewitt DE, Pallant JF, Cunningham CE. Rural origin plus a rural clinical school placement is a significant predictor of medical students’ intentions to practice rurally: a multi-university study. Rural Remote Health. 2012;12:1908. doi:10.22605/RRH1908
- Jamar E, Newbury J, Mills D. Early career location of University of Adelaide rural cohort medical students. Rural Remote Health. 2014;14:2592. doi:10.22605/RRH2592
- Lynch DC, Teplin SE, Willis SE, et al. Interim evaluation of the Rural Health Scholars Program. Teach Learn Med. 2001;13(1):36-42. doi:10.1207/S15328015TLM1301_7
- Glasser M, Hunsaker M, Sweet K, MacDowell M, Meurer M. A comprehensive medical education program response to rural primary care needs. Acad Med. 2008;83(10):952-961. doi:10.1097/ACM.0b013e3181850a02
- MacDowell M, Glasser M, Hunsaker M. A decade of rural physician workforce outcomes for the Rockford Rural Medical Education (RMED) Program, University of Illinois. Acad Med. 2013;88(12):1941-1947. doi:10.1097/ACM.0000000000000031
- Stearns JA, Stearns MA, Glasser M, Londo RA. Illinois RMED: a comprehensive program to improve the supply of rural family physicians. Fam Med. 2000;32(1):17-21.
- Wheat JR, Leeper JD, Brandon JE, Guin SM, Jackson JR. The rural medical scholars program study: data to inform rural health policy. J Am Board Fam Med. 2011;24(1):93-101. doi:10.3122/jabfm.2011.01.100013
- Wheat JR, Brandon JE, Leeper JD, Jackson JR, Boulware DW. Rural health leaders pipeline, 1990-2005: case study of a second-generation rural medical education program. J Agromed. 2007;12(4):51-61. doi:10.1080/10599240801985951
- Halaas GW, Zink T, Finstad D, Bolin K, Center B. Recruitment and retention of rural physicians: outcomes from the rural physician associate program of Minnesota. J Rural Health. 2008;24(4):345-352. doi:10.1111/j.1748-0361.2008.00180.x
- Verby JE, Newell JP, Andresen SA, Swentko WM. Changing the medical school curriculum to improve patient access to primary care. JAMA. 1991;266(1):110-113. doi:10.1001/jama.1991.03470010114041
- Verby JE. The Minnesota Rural Physician Associate Program for medical students. J Med Educ. 1988;63(6):427-437. doi:10.1097/00001888-198806000-00001
- Verby JE. The Minnesota Rural Physician Redistribution Plan, 1971 to 1976. JAMA. 1977;238(9):960-964. doi:10.1001/jama.1977.03280100044021
- Sesney JW, Kreher NE, Potts MJ. Graduates’ reflections on their rural medical education: the Upper Peninsula campus experience. J Rural Health. 1994;10(4):279-285. doi:10.1111/j.1748-0361.1994.tb00242.x
- Wendling AL, Phillips J, Short W, Fahey C, Mavis B. Thirty years training rural physicians: outcomes from the Michigan State University College of Human Medicine Rural Physician Program. Acad Med. 2016;91(1):113-119. doi:10.1097/ACM.0000000000000885
- Eidson-Ton WS, Rainwater J, Hilty D, et al. Training medical students for rural, underserved areas: a rural medical education program in California. J Health Care Poor Underserved. 2016;27(4):1674-1688. doi:10.1353/hpu.2016.0155
- LeBlanc KE. Fostering rural physicians: the early success of the rural scholars track at Louisiana State University Health Sciences Center School of Medicine--New Orleans. J LA State Med Soc. 2008;160(3):142, 144-146, 148.
- Quinn KJ, Kane KY, Stevermer JJ, et al. Influencing residency choice and practice location through a longitudinal rural pipeline program. Acad Med. 2011;86(11):1397-1406. doi:10.1097/ACM.0b013e318230653f
- Cathcart-Rake W, Robinson M, Paolo A. From infancy to adolescence: the Kansas University School of Medicine-Salina: a rural medical campus story. Acad Med. 2017;92(5):622-627. doi:10.1097/ACM.0000000000001455
- Stimmel B, Serber M. The role of curriculum in influencing students to select generalist training: a 21-year longitudinal study. J Urban Health. 1999;76(1):117-126. doi:10.1007/BF02344466
- Wei McIntosh E, Morley CP. Family medicine or primary care residency selection: effects of family medicine interest groups, MD/MPH dual degrees, and rural medical education. Fam Med. 2016;48(5):385-388.
- Greer T, Kost A, Evans DV, et al. The WWAMI Targeted Rural Underserved Track (TRUST) Program: an innovative response to rural physician workforce shortages. Acad Med. 2016;91(1):65-69. doi:10.1097/ACM.0000000000000807
- Radecki SE, Abbott AV, Girard RA. An elective primary care track in the preclinical years. Fam Med. 1994;26(10):638-644.
- Haq C, Stearns M, Brill J, et al. Training in Urban Medicine and Public Health: TRIUMPH. Acad Med. 2013;88(3):352-363. doi:10.1097/ACM.0b013e3182811a75
- Adkins RJ, Anderson GR, Cullen TJ, Myers WW, Newman FS, Schwarz MR. Geographic and specialty distributions of WAMI Program participants and nonparticipants. J Med Educ. 1987;62(10):810-817. doi:10.1097/00001888-198710000-00004
- Schwarz MR. The WAMI program: a progress report. West J Med. 1979;130(4):384-390.
- Phillips TJ, Rosenblatt RA, Schaad DC, Cullen TJ. The long-term effect of an innovative family physician curricular pathway on the specialty and location of graduates of the University of Washington. Acad Med. 1999;74(3):285-288. doi:10.1097/00001888-199903000-00021



There are no comments for this article.