Background and Objectives: There is an ongoing shortage of primary care physicians in the United States. Medical schools are under pressure to address this threat to the nation’s health by producing more primary care graduates, including family physicians. Our objective was to identify institutional characteristics associated with more medical students choosing primary care.
Methods: We conducted a systematic literature review with narrative synthesis to identify medical school characteristics associated with increased numbers or proportions of primary care graduates. We included peer-reviewed, published research from the United States, Canada, Australia, and New Zealand. The existing literature on characteristics, including institutional geography, funding and governance, mission, and research emphasis, was analyzed and synthesized into summary statements.
Results: Ensuring a strong standing of the specialty of family medicine and creating an atmosphere of acceptance of the pursuit of primary care as a career are likely to increase an institution’s percentage of medical students entering primary care. Training on regional campuses or providing primary care experiences in rural settings also correlates with a larger percentage of graduates entering primary care. A research-intensive culture is inversely correlated with primary care physician production among private, but not public, institutions. The literature on institutional financial incentives is not of high enough quality to make a firm statement about influence on specialty choice.
Conclusions: To produce more primary care providers, medical schools must create an environment where primary care is supported as a career choice. Medical schools should also consider educational models that incorporate regional campuses or rural educational settings.
There is an ongoing shortage of primary care physicians in the United States.1 Population growth, aging, and insurance expansion are all factors that will lead to an even greater shortage in the future.2 Limitations in access to primary care will result in more expensive, but less effective, health care at the population and individual patient levels.3-5
Efforts to increase the primary care physician workforce have occurred at many levels. In some states, legislation has been passed toward this end, including Medicaid payment rate increases and the opening of new medical schools with the intent to address workforce shortages.6 Nationally, eight family medicine organizations have adopted a collective goal of 25% of medical students entering family medicine by 2030.7
Medical school administrators and leaders have a social obligation to educate physicians to provide for the health care needs of the nation, including the provision of primary care to meet the public’s needs.8 This obligation is directly acknowledged and reflected in the mission statements of some medical schools.9
To positively impact the production of primary care physicians, it is important to identify institutional characteristics that are associated with increased percentages of medical students choosing to enter a career in primary care generally, and family medicine specifically, as students matching into family medicine are those most likely to enter the primary care workforce.10 These characteristics may be modifiable or fixed, and may include things like geographic location, funding source, governance structures, or institutional missions. Our goal was to review, synthesize, and summarize the existing literature pertaining to those medical schools’ attributes.
We conducted a systematic literature search with narrative synthesis to identify medical school characteristics that were associated with increased numbers or proportions of primary care graduates. This study was part of a larger study examining undergraduate medical education interventions associated with primary care specialty choice.11 The study was deemed to not be human subjects research by the Michigan State University Institutional Review Board.
Articles focused on medical school structures, and characteristics were obtained from a larger pool of articles that met inclusion criteria for the larger study. The scope of the study included peer-reviewed research studies conducted at medical schools in the United States, Canada, Australia and New Zealand. We utilized the definition of primary care of Phillips et al.11
Additional focused secondary searches were performed to identify relevant studies conducted using database-specific controlled vocabulary and free-text search terms developed through language mapping during the scoping review. The additional search strategy is detailed in Appendix 1 (https://journals.stfm.org/media/4921/appendix1-seehusen-july22.pdf). The supplementary searches were conducted February 27, 2020 in Medline (PubMed) and Education Resources Information Center (EBSCO), and no date limit was applied. Two medical librarians assisted with search strategy development and implementation and manuscript retrieval. We used citation chaining to ensure comprehensiveness and identify literature not captured by the database searches.
Initially, we planned to incorporate medical school admission processes and practices into the broader set of institutional factors. However, during the analysis and synthesis of the initial data set of articles, it became clear that those describing admissions processes offered a qualitatively distinct content area and were thus analyzed and synthesized separately.12
First, we identified institutional characteristics that had been sufficiently studied to be included in this review. Next, we analyzed and synthesized the existing research on each institutional characteristic into summary statements reflecting the whole of the literature that met inclusion criteria for that characteristic. One author (D.S.) took the lead on extracting findings from individual studies and synthesizing generalized results from the included papers. A second author (M.R.) independently verified the conclusions of the first author and validated and edited the first draft of results. Other authors independently validated the summative statements against their own interpretation of the literature. Disagreement was adjudicated by collaborative discussion.
Finally, institutional characteristics associated with primary care specialty choice were classified by their relative mutability. This classification was based on both evidence of mutability in the literature and the reflections of the authors. The entire author team reviewed and edited the draft and contributed to the narrative synthesis and interpretation of the findings.
We identified a total of 73 included and related studies obtained from the primary scoping review as potentially eligible for the topic area of institutional admissions processes and other institutional characteristics. Additional focused searches for this topic resulted in retrieval of 1,153 additional articles. After review of the titles and abstracts, we evaluated the full text of 98 articles for inclusion. We also evaluated 16 articles discovered through citation chaining in full for possible inclusion. Of these 187 articles, 50 ultimately met our inclusion criteria specifically for institutional characteristics associated with primary care career choice. These articles explored seven distinct factors: institutional ownership, mission, stature of family medicine within the institution, acceptance of primary care as a career choice, financial factors, research, and location.
Ownership
Public allopathic schools produce a higher percentage of primary care graduates than private allopathic schools,13 a finding that remains highly significant after controlling for multiple variables.14-16 This finding may not apply to osteopathic schools, most of which are private.16,17
Institutional Mission
An institution’s mission, in theory, influences what is considered important by institutional personnel. In the early 1990s, Martini reported that 35% of allopathic medical schools, and all osteopathic schools, had mission statements that included a comment about primary care. Among allopathic schools, private schools with such a mission produced significantly more primary care physicians; this was not the case among public schools.17 Schools that have a primary care mission and are perceived as being more encouraging of student interest in primary care also have a history of producing a larger percentage of generalists.18
Mullan et al created a social mission score that combined scores based upon the percentage of graduates who ultimately practice primary care, the percentage of graduates practicing in health professional shortage areas, and the percentage of graduates belonging to underrepresented in medicine groups. The 20 schools with the highest social mission scores produced significantly more primary care physicians than the 20 schools with the lowest scores.8 Morley et al expanded upon this idea, also creating a social mission scale, and determined that schools with a higher degree of social mission produced more family physicians and more physicians who ultimately provided care to underserved populations.9
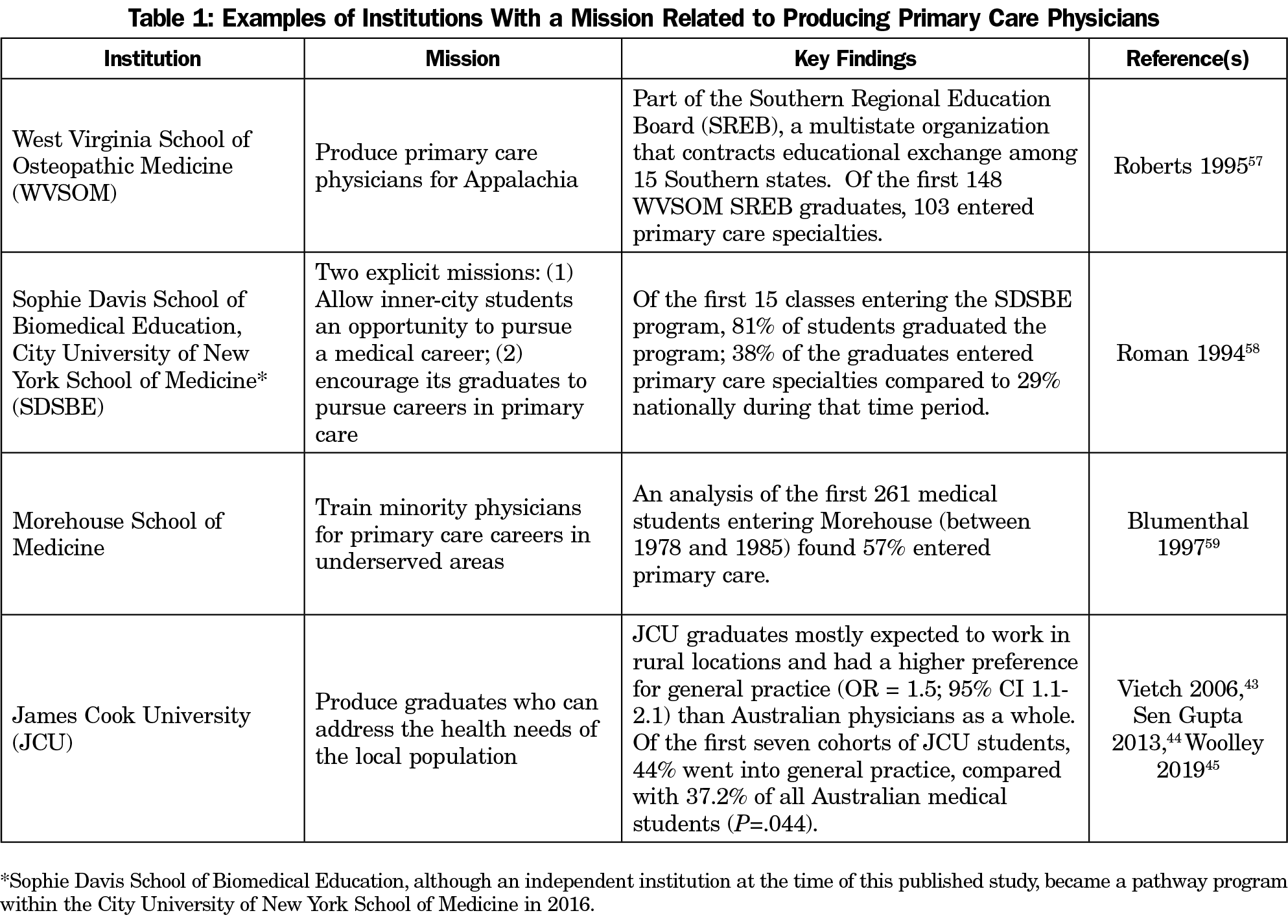
Besides these studies, the majority of the literature around institutional mission consists of descriptive reports of exemplar institutions that link successful production of primary care physicians to an institution’s broader mission (Table 1).
We found no reports of a medical school successfully changing its mission to include producing more primary care physicians. On the contrary, Kuzel reported on a Virginia state legislative mandate that three of the state’s medical schools produce 50% generalists, resulting in student backlash against perceived pressure within the institution for students to choose primary care.19
Stature of Family Medicine Within the Institution
While most medical schools have departments of family medicine today, this was not always the case.20 Literature from the 1980s, when departments of family medicine were less common, described an association between having a family medicine department and higher production of family physicians.13,17,21 However, this association disappeared after controlling for other variables.14 More recently, Phillips et al reported that the few allopathic medical schools that do not have a department of family medicine produce fewer family physicians than those that do. This dichotomy is not found among osteopathic schools.16 Herold reported an interesting counterexample in which plans were developed to demote a department of family medicine to a division of internal medicine. Subsequently, the number of graduating students entering family medicine at that institution decreased.22
Campos-Outcalt found the proportion of family medicine faculty at an institution was a statistically significant predictor of the proportion of family medicine graduates.15 Using linear regression modelling, Wimsatt et al found that medical schools with at least one family medicine faculty member in a leadership position had a 3% higher match rate into family medicine residencies.23
The Acceptance of Primary Care as a Career Choice
The “hidden curriculum” in medical education was defined by Thomas Inui as the experiences of students outside their formal coursework, “what we actually do in our day-to-day work with patients and one another, not what we say should be done when we stand behind podiums and lecture halls.”24 This concept has been applied to describe the pressure within the culture of medical education that steers medical students towards specialty care and away from primary care careers. A significant amount of literature on this topic exists, although it is not always explicitly labeled hidden curriculum. Occasionally is it described as “badmouthing”25 or “bashing”26 primary care. More often, it is studied through the lens of an institutional culture that unconsciously emphasizes specialization over generalization.27
Multiple studies have found that a perceived lack of respect for primary care, or family medicine specifically, is associated with lower student enthusiasm for primary care.28-32 By contrast, institutional support to pursue family medicine as a career can influence students to choose family medicine.30
Negativity toward primary care is not always hidden. Campos-Outcalt demonstrated that medical students frequently hear negative comments about the specialty of family medicine, but in this study did not identify an association between these comments and eventual career choice.33 However, subsequent studies indicate that these comments are influential. In a qualitative study, Canadian medical students reported little exposure to family medicine in the preclinical years but did report hearing disparaging comments. These students reported these comments did have an impact on their opinion about family medicine as a career.34 Students who attend schools reporting high levels of badmouthing primary care are less likely to report an intention to go into primary care.35 Students who report being exposed to a higher ratio of negative-to-positive comments about primary care are less interested in a primary care career.36
Financial Factors
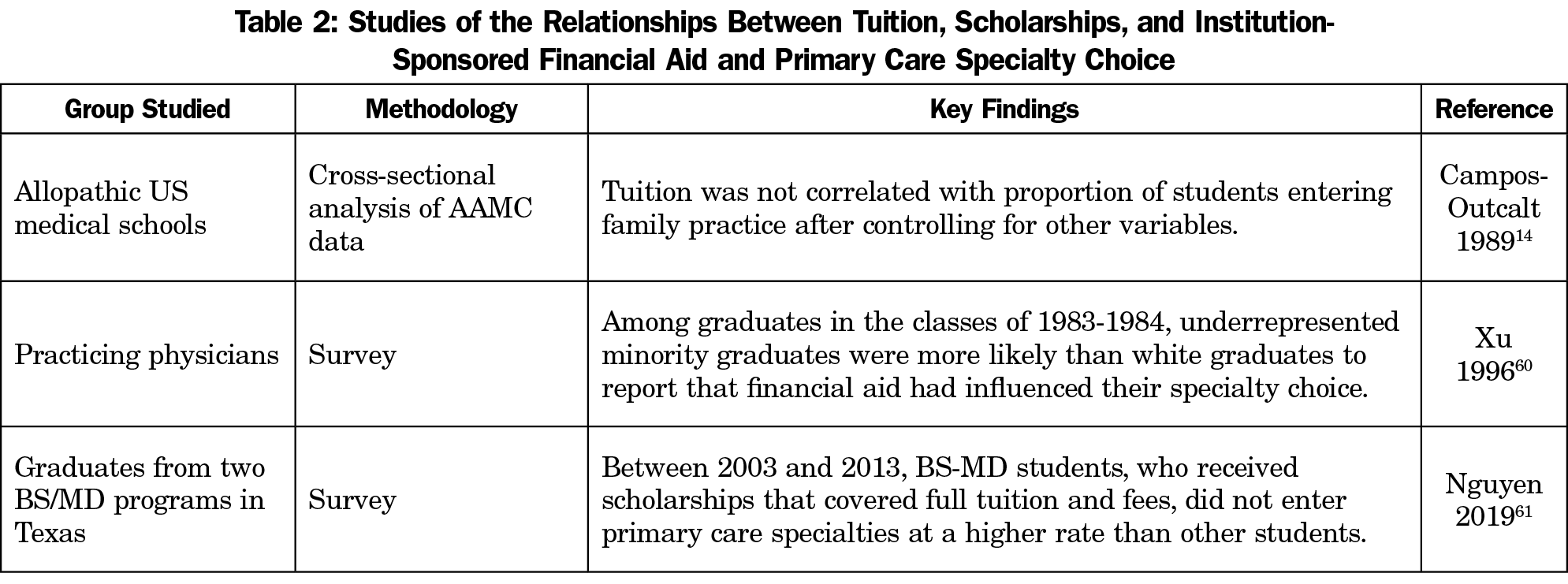
Although much literature has been published on medical student debt and student perception of specialty income, only three studies addressed financial issues that are directly controlled by institutions: tuition rates, scholarships, and other institution-sponsored financial aid (Table 2). Two of the three were single-institution studies. These studies have not clearly demonstrated that programs reducing the cost of medical education, either for all students or for individual students, influences students’ specialty choices.
Research Emphasis
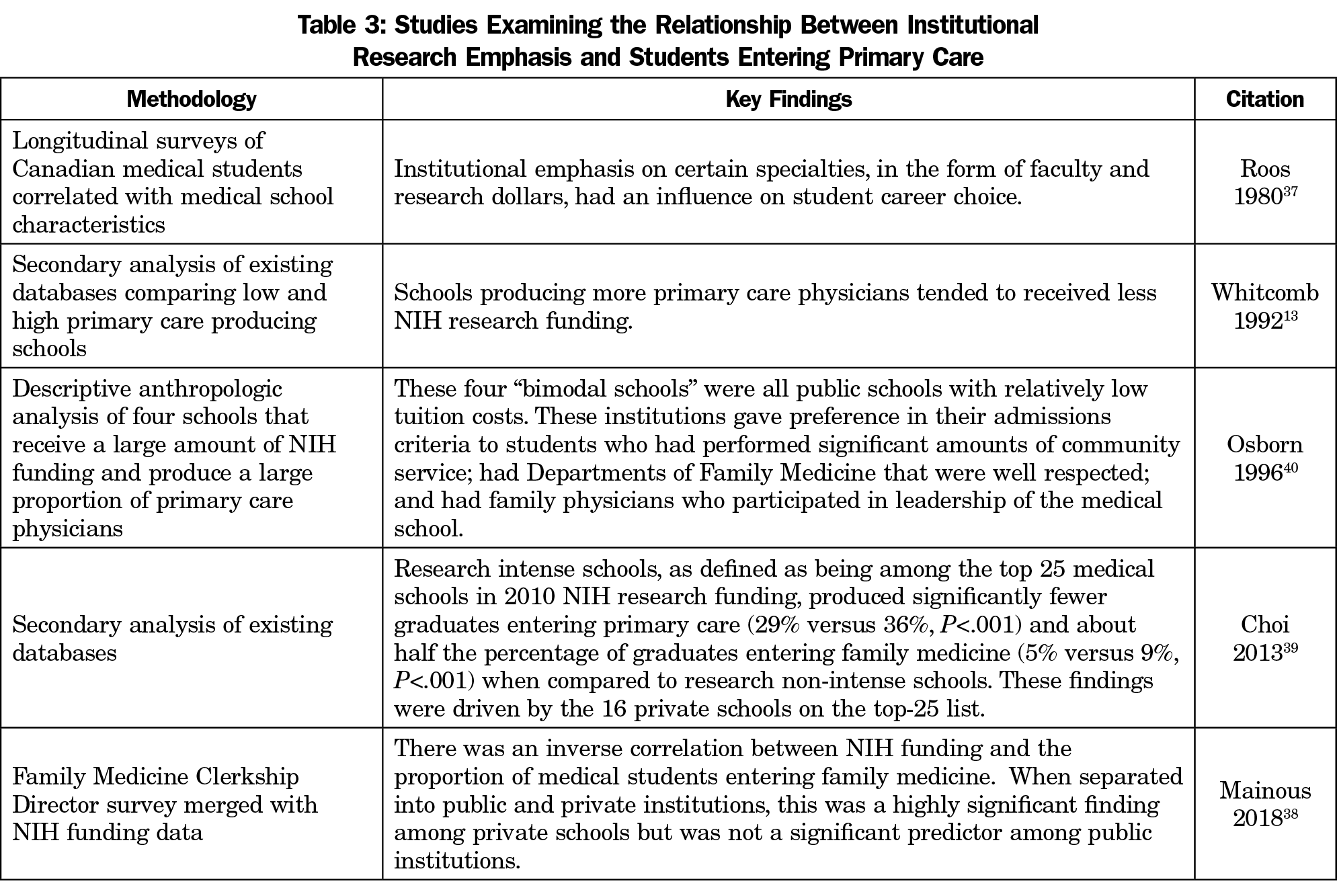
For over 5 decades, the literature has consistently shown that the rate of medical students going into primary care is inversely related to institutional research emphasis.8,13,37-39 Studies that have separated schools by public or private funding have found this association is most significant for private institutions, with public schools producing similar percentages of family medicine graduates among research intensive and nonresearch-intensive schools.38,39 A noteworthy qualitative study of four institutions with both a large proportion of primary care graduates, and high research productivity, found that each institution had strong primary care leadership and a commitment to service. All four were public, state-supported allopathic institutions.40 Table 3 summarizes key studies of institutional research emphasis and production of primary care physicians.
Location
Medical schools tend to admit more applicants from their state and region, sometimes because of a legislative or institutional mandate. Graduates, in turn, tend to practice close to where they train.20,41 In 2012, 45% of medical students entered residency in the state in which they attended medical school.20
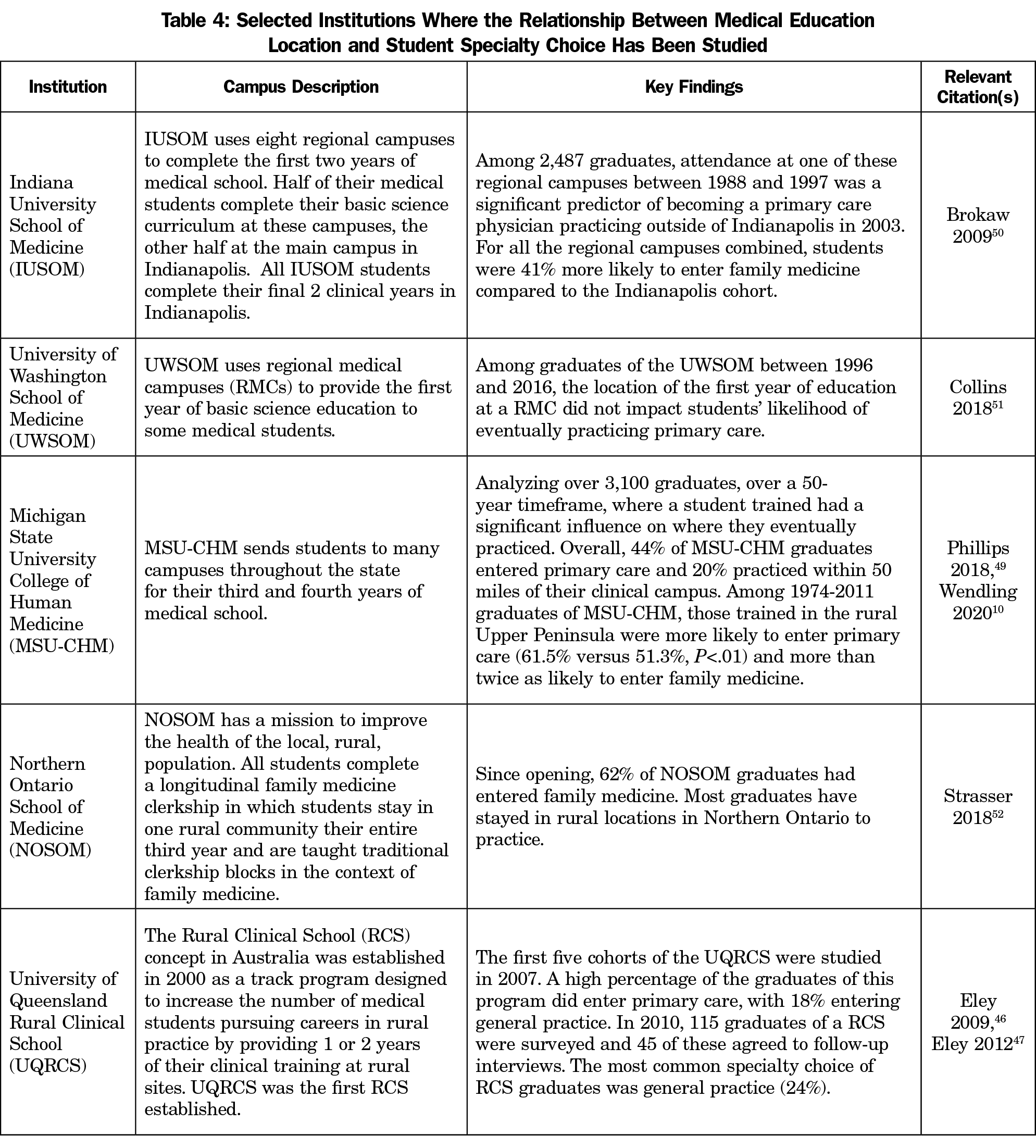
Completing at least part of undergraduate medical education in a rural area is associated with a higher likelihood of primary care career choice. The impact of training location can be difficult to isolate because students are generally given a choice about where they want to train, and this regional education is often in the context of an educational pathway program.10,20,21,42-47 However, most studies of career choice of students training on regional campuses have demonstrated that distributed models lead to higher numbers of primary care physicians, 10,41,48-50 with one exception.51 In some studies, this association was present even in the absence of a distinct curricular pathway.50,52 Table 4 summarizes studies examining the associations between regionally distributed educational models and eventual primary care specialty choice.
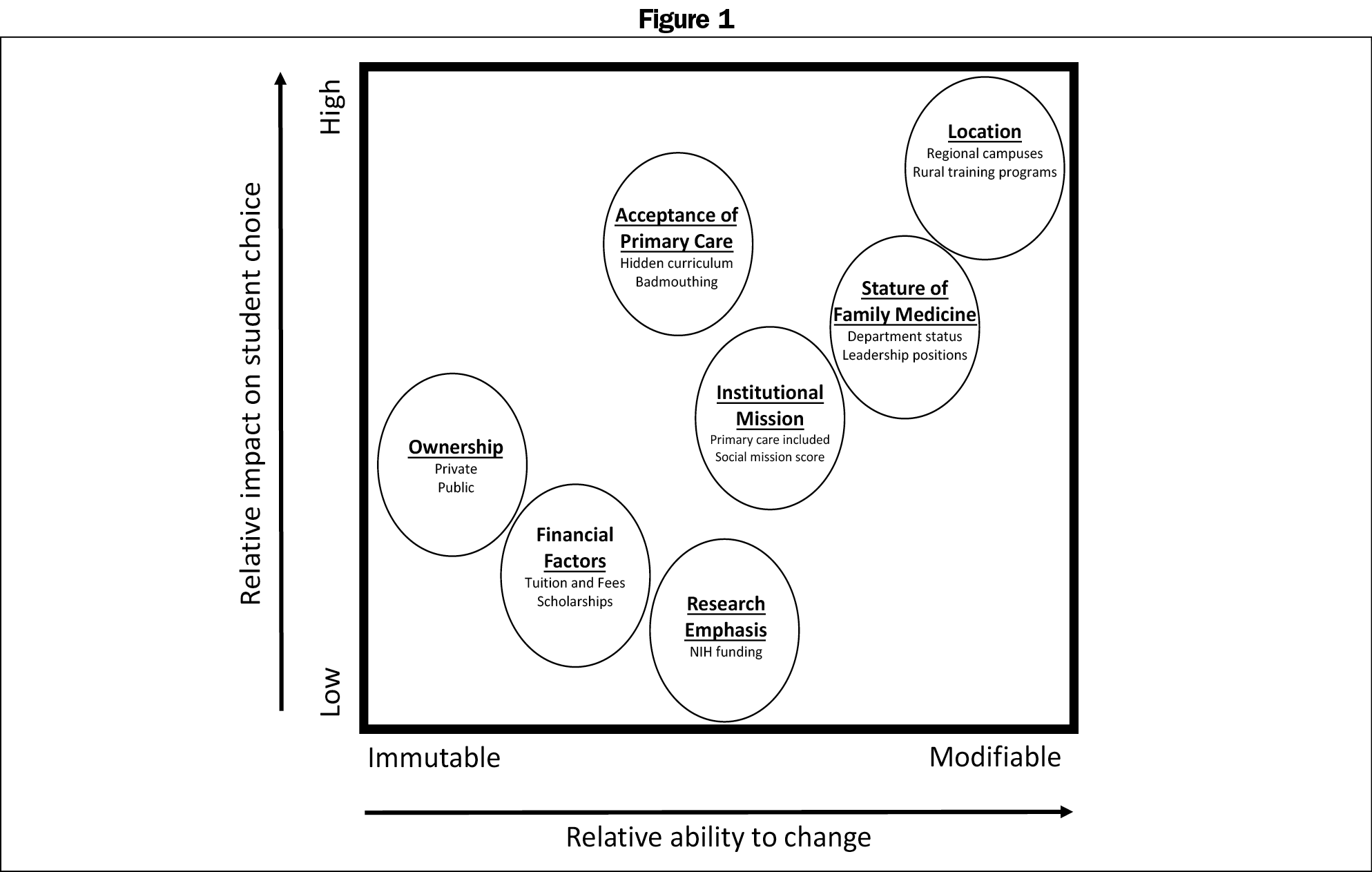
Our findings show that several institutional factors may impact primary care choice, including an institution’s climate surrounding primary care, the presence of regional campuses or rural training experiences, or a school’s ownership structure or research emphasis. Some of these characteristics are more easily mutable, or have a higher impact, than others. Figure 1 depicts the relative mutability and impact of each of the institutional factors.
In the course of reviewing and synthesizing the literature, the authors were struck by the consistency of the findings, and also the limited evidence of institutional efforts to change structural characteristics. It would be difficult to change a medical school’s geographic location, and we found no reports of institutions that have changed from public to private governance (or vice versa). There was also very limited change over time between a 2015 study of medical school mission statements53 and a 2019 network analysis of mission statements.54 However, changes in National Institutes of Health funding disbursement to researchers based at medical schools demonstrate that research intensity is clustered in fewer and fewer schools over time.55 One interpretation of this finding could be that institutions do change their functional missions, including a change in focus toward–or away from–research intensity. Similarly, regional campuses are becoming an increasingly commonplace feature of medical schools.56 Medical education researchers should consider ways to take advantage of these natural experiments, not only to document the effects of these changes on the future primary care workforce, but to help medical schools consider the potential unintended consequences of changes.
The climate surrounding primary care at an institution, including an institution’s mission, overall number and leadership strength of family medicine faculty, and positivity or negativity toward primary care, impacts the proportion of graduates who ultimately choose primary care careers. Although the literature supports this association, organizational culture is also notoriously difficult to change, and we found no successful examples of an institution deliberately changing their mission or culture to produce more primary care physicians. Still, it seems logical for institutions hoping to produce more primary care graduates to add this goal to their mission statement and to actively promote a culture that celebrates primary care as a career choice.
However, we did find limited published evidence that some schools made changes that increased the visibility and stature of primary care. Incremental changes made to influence climate, such as family medicine faculty taking on more visible leadership roles or consciously promoting positive messages regarding primary care, are early strategies that institutions could adopt. This is not work that can be undertaken by family medicine departments alone, but work that needs to be shared among the entire institutional leadership. We encourage future medical education researchers in all disciplines to focus on innovative strategies to build a more positive culture toward primary care in US medical schools.
Once established, it is difficult to change the location or ownership of a medical school, but incorporating a regional campus or expanding education in rural settings may be feasible for institutions hoping to bolster the primary care physician workforce. Medical schools that have invested in these educational models have seen higher overall proportions of graduates enter primary care fields. States and medical schools should consider adding rural or regional campuses as a deliberate strategy to augment the primary care physician workforce.
This literature supported an inverse association between research intensity and the proportion of primary care graduates among private schools, which may be a reflection of the culture of these institutions. In other words, high research intensity may be a surrogate marker for the hidden curriculum of low respect for primary care. The exceptions to this rule demonstrate that institutions can foster a culture of positive regard for primary care while also maintaining a highly productive research culture.40 For this reason, we suggest departments of family medicine should continue to engage in research, particularly in research-intensive institutions, not only for the benefits of the work itself, but also because students with research interests need family physician clinician-scientist role models. Future studies could prospectively explore this relationship by tracking primary care graduate output after significant changes in institutional research funding, both globally and within departments of family medicine. Funders and policy makers could create additional granting mechanism targeted toward primary care. This would make primary care more attractive to students with research interests.
Our study has several limitations. First, the definition of primary care varies in the literature. Sometimes studies used a narrow definition while others a more expansive definition. Second, the influence of some factors has shifted over time and is likely to continue to shift. Lastly, limiting our search to just four countries may also limit the generalizability of our findings.
Changing either the culture or the foundational structure of an institution is challenging, but the foundational goal of medical education is to promote the health of our communities. Strong evidence supports that the shortage of primary care physicians in the United States has negative downstream patient and public health consequences. We encourage all medical schools to consider investment in institutional changes to support student choice of primary care careers.
Acknowledgments
The authors thank Shelby Walker, MD, Virginia Young, MLS, and Morgan Pratte, MPH, for their substantial contributions to the literature search, literature retrieval, and data organization.
Funding Statement: This project was partially supported by a grant from the American Board of Family Medicine (ABFM) Foundation (Dr Julie Phillips, PI), and also partially by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) under grant number D54HP23297, Academic Administrative Units (Dr Chris Morley, PI). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the ABFM, HRSA, HHS, or the US Government.
Disclaimer: This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by Health Resources and Services Administration, Department of Health and Human Services, US Air Force, Department of Defense, or the US Government.
References
- The Complexities of Physician Supply Projections From 2019 to 2034. Washington, DC: American Association of Medical Colleges, June 2021. Accessed March 4, 2022. https://www.aamc.org/media/54681/download
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. doi:10.1370/afm.1431
- Phillips RL Jr, Bazemore AW. Primary care and why it matters for U.S. health system reform. Health Aff (Millwood). 2010;29(5):806-810. doi:10.1377/hlthaff.2010.0020
- Sabety AH, Jena AB, Barnett ML. Changes in health care use and outcomes after turnover in primary care. JAMA Intern Med. 2021;181(2):186-194. doi:10.1001/jamainternmed.2020.6288
- Phillips RL Jr, McCauley LA, Koller CF. Implementing high-quality primary care: a report from the National Academies of Sciences, Engineering, and Medicine. JAMA. 2021;325(24):2437-2438; Epub ahead of print. doi:10.1001/jama.2021.7430
- Friedberg MW, Martsolf GR, White C, et al. Evaluation of policy options for increasing the availability of primary care services in rural Washington State. Rand Health Q. 2017;6(4):8.
- Kelly C, Coutinho AJ, Goldgar C, et al. Collaborating to achieve the optimal family medicine workforce. Fam Med. 2019;51(2):149-158. doi:10.22454/FamMed.2019.926312
- Mullan F, Chen C, Petterson S, Kolsky G, Spagnola M. The social mission of medical education: ranking the schools. Ann Intern Med. 2010;152(12):804-811. doi:10.7326/0003-4819-152-12-201006150-00009
- Morley CP, Mader EM, Smilnak T, et al. The social mission in medical school mission statements: associations with graduate outcomes. Fam Med. 2015;47(6):427-434.
- Wendling AL, Short A, Hetzel F, Phillips JP, Short W. Trends in subspecialization: a comparative analysis of rural and urban clinical education. Fam Med. 2020;52(5):332-338. doi:10.22454/FamMed.2020.182557
- Phillips JP, Wendling AL, Prunuske J, et al. Medical school characteristics, policies, and practices that support primary care specialty choice: a scoping review of five decades of research. Fam Med. 2022;54(7):542-554.
- Raleigh MF, Seehusen D, Phillips JP, et al. Influences of medical school admissions practices on primary care career choice. Fam Med. 2022;54(7):536-541.
- Whitcomb ME, Cullen TJ, Hart LG, Lishner DM, Rosenblatt RA. Comparing the characteristics of schools that produce high percentages and low percentages of primary care physicians. Acad Med. 1992;67(9):587-591. doi:10.1097/00001888-199209000-00009
- Campos-Outcalt D, Senf JH. Characteristics of medical schools related to the choice of family medicine as a specialty. Acad Med. 1989;64(10):610-615.
- Campos-Outcalt D, Senf J. Medical school financial support, faculty composition, and selection of family practice by medical students. Fam Med. 1992;24(8):596-601.
- Phillips JP, Wendling A, Bentley A, Marsee R, Morley CP. Trends in US medical school contributions to the family physician workforce: 2018 update from the American Academy of Family Physicians. Fam Med. 2019;51(3):241-250. doi:10.22454/FamMed.2019.395617
- Martini CJM, Veloski JJ, Barzansky B, Xu G, Fields SK. Medical school and student characteristics that influence choosing a generalist career. JAMA. 1994;272(9):661-668. doi:10.1001/jama.1994.03520090025014
- Block SD, Clark-Chiarelli N, Singer JD. Mixed messages about primary care in the culture of U.S. medical schools. Acad Med. 1998;73(10):1087-1094. doi:10.1097/00001888-199810000-00020
- Kuzel AJ, Moore SS, Choosing A. Choosing a specialty during a generalist initiative: a focus group study. Fam Med. 1999;31(9):641-646.
- Biggs WS, Crosley PW, Kozakowski SM. Entry of US medical school graduates into family medicine residencies: 2012--2013. Fam Med. 2013;45(9):642-646.
- Rosenblatt RA, Whitcomb ME, Cullen TJ, Lishner DM, Hart LG. The effect of federal grants on medical schools’ production of primary care physicians. Am J Public Health. 1993;83(3):322-328. PMID:8438966 doi:10.2105/AJPH.83.3.322
- Herold AH, Woodard LJ, Roetzheim RG, Van Durme DJ, Pamies RJ. Influence of uncertainty about a specialty’s administrative status on students’ specialty choices at a Florida medical school. Acad Med. 1991;66(5):295-297. doi:10.1097/00001888-199105000-00016
- Wimsatt LA, Cooke JM, Biggs WS, Heidelbaugh JJ. Institution-specific factors associated with family medicine residency match rates. Teach Learn Med. 2016;28(3):269-278. doi:10.1080/10401334.2016.1159565
- Inui TS. A Flag. In: The Wind: Educating For Professionalism In Medicine. Washington, DC: Association of American Medical Colleges; 2003.
- Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med. 2013;88(12):1919-1926. doi:10.1097/ACM.0000000000000038
- Holmes D, Tumiel-Berhalter LM, Zayas LE, Watkins R. “Bashing” of medical specialties: students’ experiences and recommendations. Fam Med. 2008;40(6):400-406.
- Carlin E, Alberti H, Davies K. Denigration of general practice as a career choice: the students' perspective. a qualitative study. BJGP Open. 2021 Feb 23;5(1):bjgpopen20X101132. doi:10.3399/bjgpopen20X101132
- Kost A, Kardonsky K, Cawse-Lucas J, Sairenji T. Association of family medicine interest at matriculation to medical school and FMIG participation with eventual practice as a family physician. Fam Med. 2019;51(8):682-686. doi:10.22454/FamMed.2019.239373
- Rodríguez C, Tellier PP, Bélanger E. Exploring professional identification and reputation of family medicine among medical students: a Canadian case study. Educ Prim Care. 2012;23(3):158-168. doi:10.1080/14739879.2012.11494099
- Alavi M, Ho T, Stisher C, et al. Factors that influence student choice in family medicine: a national focus group. Fam Med. 2019;51(2):143-148. doi:10.22454/FamMed.2019.927833
- Weiland G, Cox K, Sweeney MK, et al. What attracts medical students to primary care? a nominal group evaluation. South Med J. 2019;112(2):76-82. doi:10.14423/SMJ.0000000000000933
- LI J. Zhang Y, Shen Y, Yao J, and Grinspan Z. Selection or education? Medical school ranking and medical students’ specialty choice preferences in the United States. Educ Prim Care. 2019;30(4):202-211. doi:10.1080/14739879.2019.1603083
- Campos-Outcalt D, Senf J, Kutob R. Comments heard by US medical students about family practice. Fam Med. 2003;35(8):573-578.
- Scott I, Wright B, Brenneis F, Brett-MacLean P, McCaffrey L. Why would I choose a career in family medicine? Can Fam Phys. 2007;53:1956-1957.
- Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med. 2013;88(12):1919-1926. doi:10.1097/ACM.0000000000000038
- Wendling AL, Wudyka AE, Phillips JP, et al. RU4PC? Texting to quantify feedback about primary care and its relationship with student career interest. Fam Med. 2016;48(1):21-29. PMID:26950662
- Roos NP, Roos LL Jr. Medical school impact on student career choice: a longitudinal study. Eval Health Prof. 1980;3(1):3-19. doi:10.1177/016327878000300101
- Mainous AG III, Porter M, Agana DF, Chessman AW. Institutional NIH research funding and a culture of support for family medicine-their relationship to family medicine specialty choice. Fam Med. 2018;50(5):369-371. doi:10.22454/FamMed.2018.913629
- Choi PA, Xu S, Ayanian JZ. Primary care careers among recent graduates of research-intensive private and public medical schools. J Gen Intern Med. 2013;28(6):787-792. doi:10.1007/s11606-012-2286-z
- Osborn EHS, O’Neil EH. “Bimodal” medical schools: excelling in research and primary care. Acad Med. 1996;71(9):941-949. doi:10.1097/00001888-199609000-00007
- Baker HH, Pathman DE, Nemitz JW, Boisvert CS, Schwartz RJ, Ridpath LC. Which U.S. medical schools are providing the most physicians for the Appalachian region of the United States? Acad Med. 2012;87(4):498-505. doi:10.1097/ACM.0b013e318248f3be
- Ledford CJW, Guard EL, Phillips J, Morle CP, Prunuske J, Wendling AL. How Medical Education Pathways Influence Primary Care Specialty Choice. Fam Med. 2021;xx(x):xxx-xx.
- Veitch C, Underhill A, Hays RB. The career aspirations and location intentions of James Cook University’s first cohort of medical students: a longitudinal study at course entry and graduation. Rural Remote Health. 2006;6(1):537. doi:10.22605/RRH537
- Sen Gupta T, Murray R, Hays R, Woolley T. James Cook University MBBS graduate intentions and intern destinations: a comparative study with other Queensland and Australian medical schools. Rural Remote Health. 2013;13(2):2313. doi:10.22605/RRH2313
- Woolley T, Larkins S, Sen Gupta T. Career choices of the first seven cohorts of JCU MBBS graduates: producing generalists for regional, rural and remote northern Australia. Rural Remote Health. 2019;19(2):4438. doi:10.22605/RRH4438
- Eley D, Baker P, Chater B. The Rural Clinical School Tracking Project: more IS better--confirming factors that influence early career entry into the rural medical workforce. Med Teach. 2009;31(10):e454-e459. doi:10.3109/01421590902850857
- Eley DS, Synnott R, Baker PG, Chater AB. A decade of Australian Rural Clinical School graduates--where are they and why? Rural Remote Health. 2012;12:1937. doi:10.22605/RRH1937
- Liaw W, Cheifetz C, Luangkhot S, Sheridan M, Bazemore A, Phillips RL. Match rates into family medicine among regional medical campus graduates, 2007-2009. J Am Board Fam Med. 2012;25(6):894-907. doi:10.3122/jabfm.2012.06.110336
- Phillips JP, Wendling AL, Fahey CA, Mavis BE. The effect of a community-based medical school on the state and local physician workforce. Acad Med. 2018;93(2):306-313. doi:10.1097/ACM.0000000000001823
- Brokaw JJ, Mandzuk CA, Wade ME, et al. The influence of regional basic science campuses on medical students’ choice of specialty and practice location: a historical cohort study. BMC Med Educ. 2009;9(9):29. PMID:19500392 doi:10.1186/1472-6920-9-29
- Collins CP, McCarthy JF. Effect of regional medical campus education on student pursuit of primary care specialties. JRMC. 2018;1(1). doi:10.24926/jrmc.v1i1.1002
- Strasser R, Cheu H. Needs of the many: northern Ontario School of Medicine students’ experience of generalism and rural practice. Can Fam Physician. 2018;64(6):449-455.
- Valsangkar B, Chen C, Wohltjen H, Mullan F. Do medical school mission statements align with the nation’s health care needs? Acad Med. 2014;89(6):892-895. doi:10.1097/ACM.0000000000000241
- Hafferty FW, Grbic D, Hafferty PK. Mapping the mission statements of U.S. LCME-accredited medical schools: an exploration of organizational communalities. Acad Med. 2019;94(5):723-730. doi:10.1097/ACM.0000000000002626
- Noble P, Ten Eyck P, Roskoski R Jr, Jackson JB. NIH funding trends to US medical schools from 2009 to 2018. PLoS One. 2020;15(6):e0233367. doi:10.1371/journal.pone.0233367
- Kanter SL. A snapshot of medical student education in the United States and Canada: reports from 128 schools. Foreword. Acad Med. 2010;85(9)(suppl):S1. PMID:20736523 doi:10.1097/ACM.0b013e3181f13321
- Roberts A, Creech AH, Blue W. A multistate program to educate physicians: successful, economical, but endangered. Acad Med. 1995;70(7):578-582. doi:10.1097/00001888-199507000-00008
- Roman SA Jr, McGanney ML. The Sophie Davis School of Biomedical Education: the first 20 years of a unique BS-MD program. Acad Med. 1994;69(3):224-230. doi:10.1097/00001888-199403000-00018
- Blumenthal D, William M, Pederson L, Okuyemi K. Sixteen-year longitudinal evaluation of a community-oriented primary care curriculum. Educ Health. 1997;10(2):213-220.
- Xu G, Hojat M, Veloski JJ, Brose J. A national study of factors influencing primary care career choices among underrepresented-minority, white, and Asian American physicians. Acad Med. 1996;71(10)(suppl):S10-S12. doi:10.1097/00001888-199610000-00029
- Nguyen BM, Bounds G. Factors affecting specialty choice among doctors who received tuition scholarships. Fam Med. 2019;51(3):276-281. doi:10.22454/FamMed.2019.772315



There are no comments for this article.