Running-related injuries (RRI) remain a bane to all runners. Defined as running-related lower limb musculoskeletal pain causing restriction on or stoppage of running for at least 7 days or three consecutive training sessions or that requires health professional consultation,1 incidence is estimated as high as 79% for recreational and competitive runners.2 Several biomechanical variables have been associated with increased RRI risk.3,4 Studies suggest improvements in pain and RRI reduction with interventions, known as running gait retraining, targeting one or more of these variables.5-16 Most previous gait retraining studies are difficult to translate to the family physician’s clinical practice, as studies involved specialized equipment to analyze and modify gait and multiple in-office sessions,4,5,8,10,12-15 which would be impractical to implement in a busy primary care clinic. It is unclear how gait retraining is currently being taught to and utilized by family physicians. Because family physicians are likely to evaluate and treat many of these injuries,17,18 it is important to close this knowledge gap to guide graduate and continuing medical education training on this topic, as well as inform studies designed to develop more practical methods to deliver gait retraining. This study is the first seeking to close the aforementioned gap by surveying family physicians to assess the frequency of gait retraining discussions with their injured patients, the barriers to these discussions, and physician confidence and perceived value in engaging in these discussions.
BRIEF REPORTS
Running Gait Retraining: A Sports Medicine Training Gap in Family Medicine
Alexander C. Knobloch, MD, CAQSM
Fam Med. 2022;54(5):384-388.
DOI: 10.22454/FamMed.2022.405151
Background and Objectives: Emerging evidence suggests that running gait retraining plays an important role in the treatment and prevention of running-related injury, yet it remains unclear how gait retraining is being utilized by family physicians with their patients. By surveying family physicians and residents, this study is the first to investigate the frequency of gait retraining discussions with patients with running-related injuries, barriers to these discussions, and physician confidence and perceived value in engaging in these discussions, so as to better inform family physician training on this subject.
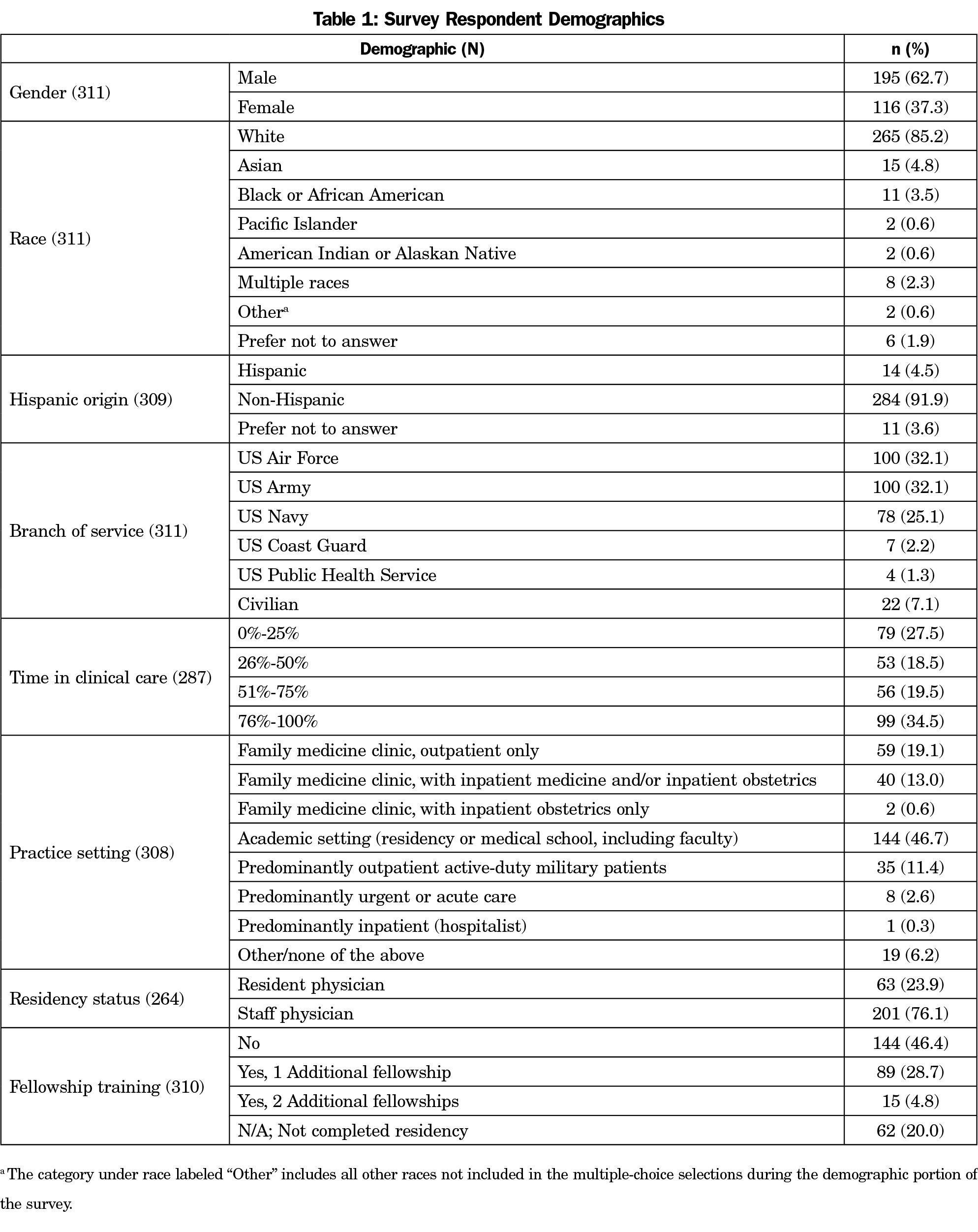
Methods: This study investigated family physician attitudes toward gait retraining though a cross-sectional survey administered to 532 military family physicians and residents at the 2019 Uniformed Services Academy of Family Physicians Annual Meeting. Main outcome measures included frequency of, confidence in, and value of discussions of running gait retraining with patients with running-related injuries. Obstacles to discussing gait retraining, knowledge on the topic, and previous training on the topic were also assessed.
Results: With a 72.2% response rate, the majority of respondents (82%) felt discussions on the topic are at least somewhat valuable. However, 63% of respondents infrequently discuss the topic with patients, while 71% lack confidence in engaging in these discussions. The most frequently reported obstacles were lack of knowledge (55%) and time (24%).
Conclusions: Family physicians find value in discussions of running gait retraining with their patients, but discussion frequency and physician confidence are low. Educational interventions increasing physician knowledge and the development of non-time-intensive approaches would be best suited for improving confidence and discussion frequency for this valued skill.
Family physicians and residents participating in the 2019 Uniformed Services Academy of Family Physicians (USAFP) Annual Meeting were invited to answer survey questions electronically regarding their attitudes toward running gait retraining. Likert-type scale and best-answer response questions queried participants’ value and confidence in, frequency of, and barriers to discussing gait retraining in patients with RRI. General knowledge of gait retraining clinical applications was assessed with a multiple-choice question. Demographic data were collected, to include previous participation in sports medicine fellowship or additional training on this topic. We analyzed categorical variables using descriptive statistics, and we used independent t tests for bivariate analyses. We analyzed data using STATA/SE 14.2 for Windows (StataCorp, LLC, College Station, TX). The Uniformed Services University of the Health Sciences Institutional Review Board, approved the project, with local approval granted by the David Grant USAF Medical Center Clinical Investigation Facility.
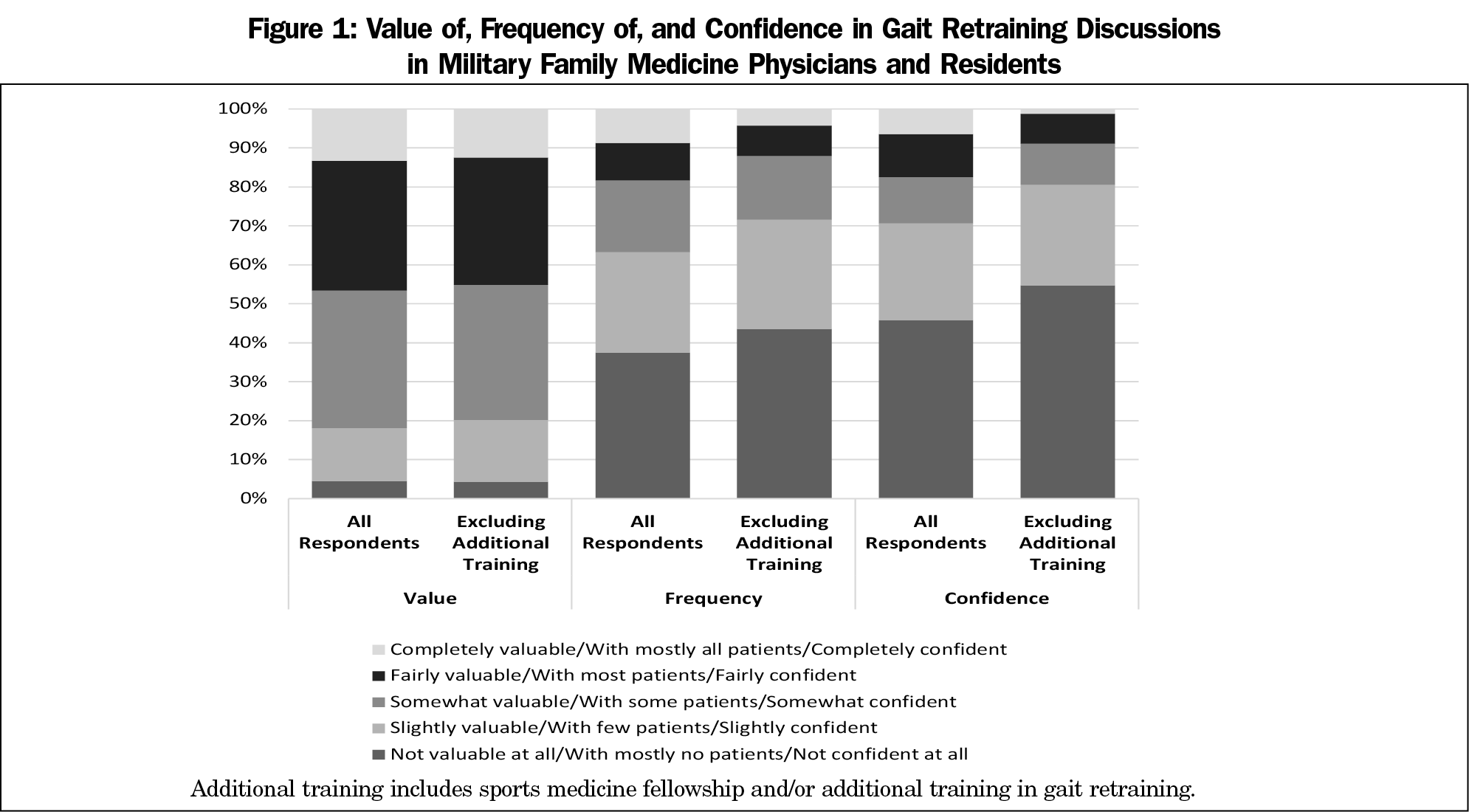
A total of 387 eligible registered attendees of the 2019 USAFP Annual Meeting responded to the survey (72.7% response rate; Table 1). Medical students and those who did not indicate training status (n=25) were excluded. The majority of respondents (82%) felt gait retraining discussions with patients are at least somewhat valuable (Figure 1). However, 63% of respondents speak with few to mostly no patients about this modality, while 71% of respondents felt only slightly confident or not confident at all in engaging in these discussions. The most frequently reported obstacles were lack of knowledge (55%) and lack of time (24%).
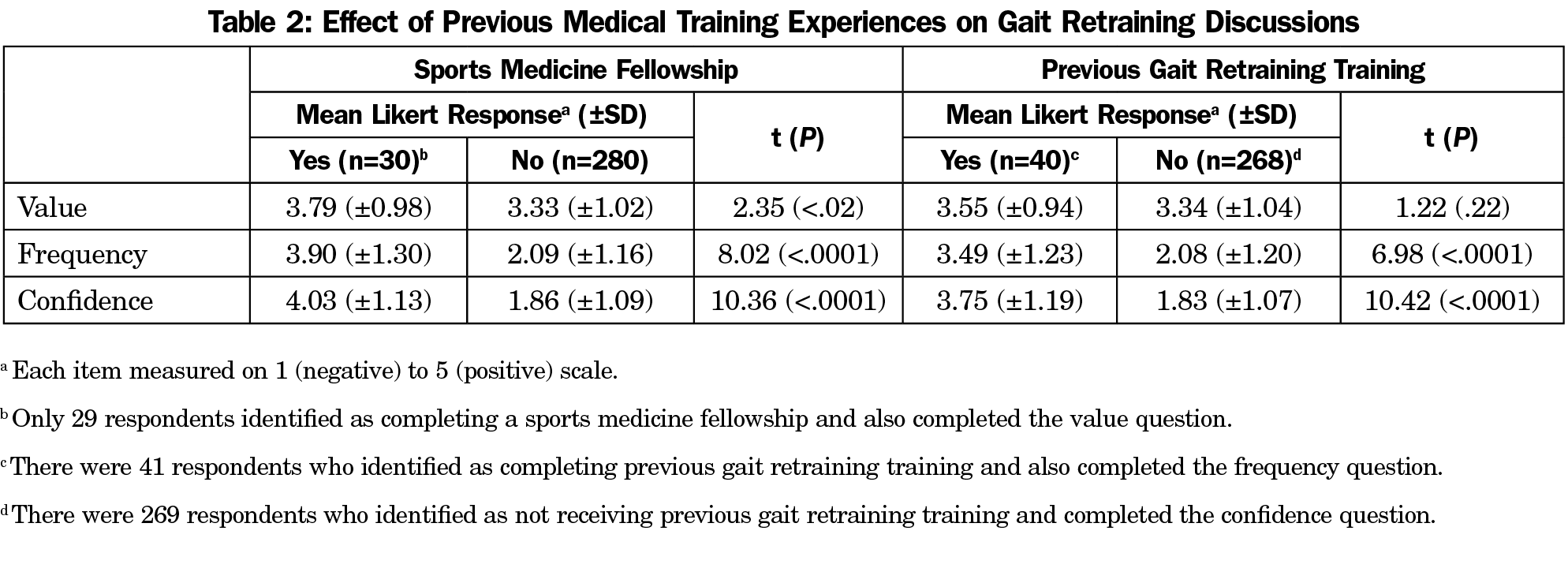
Of note, respondents with previous sports medicine fellowship experience reported significantly more value (t[307]=2.35; P<.02) and confidence (t[308]=10.36; P<.0001) in discussing gait retraining, as well as a significantly higher frequency of discussion (t[308]=8.02; P<.0001). Similarly, respondents who received previous instruction in gait retraining reported significantly more confidence (t[307]=10.42; P<.0001) and higher discussion frequency (t[307]=6.98; P<.0001), though there was no difference in value of gait retraining discussions (t(306)=1.22; P=.22; Table 2). Given these relationships, when respondents with previous training experiences were excluded, 80% of remaining respondents felt gait retraining discussions with patients are at least somewhat valuable, while 72% speak with few to mostly no patients and 81% felt only slightly confident or not confident at all in engaging in these discussions (Figure 1).
Only 24% of respondents (72/304) correctly identified that a metatarsal stress fracture was the only listed injury that did not have biomechanical or clinical evidence that suggests benefit of treatment with gait retraining, as compared to chronic exertional compartment syndrome, medial tibial stress syndrome, or patellofemoral pain syndrome.6,9-10,12-16
Most military family physician respondents find value in discussing running gait retraining with their patients, consistent with the emerging evidence that gait retraining plays an important role in RRI care.4-16 However, discussion frequency and physician confidence on the topic were low. Less than one quarter of respondents identified the correct answer to a clinical application question on the topic. While the lack of formal question validation limits the degree of interpretation of the number of correct responses, 55% of respondents still identified lack of knowledge as their largest obstacle, and the 76% of respondents with incorrect answers suggests lack of knowledge may still be an important barrier for those identifying other obstacles as their primary concern.
Previous participation in sports medicine fellowship and instruction in running gait retraining had the potential to confound our results, but they did not dramatically affect the high physician value, low discussion frequency, and low physician confidence observed in our respondent population despite inclusion of the responses of those with additional training in our analysis.
Our study was not designed to address the effects of the unique patient population cared for by military family physicians, where a high burden of musculoskeletal injury is seen in relatively young and physically active patients.19 However, given the high aforementioned incidence of running-related injuries in the general population2 and that up to 57% of runners will seek care for these injuries from a family physician,3,4 further studies evaluating civilian family physician attitudes on the topic are needed. If lack of knowledge is an important obstacle in the military family physician population, where a high burden of these injuries is seen, one may hypothesize that civilian family physicians may receive less training on the topic compared to their military counterparts, and thus also experience lack of knowledge as a substantial obstacle.
Additionally, the cross-sectional, self-reported nature of our data limits our ability to make causal inferences, as such studies are vulnerable to potential self-selection bias and social desirability bias, among others. With the low frequency and confidence reported by respondents in our study, we have a lower suspicion that social desirability bias confounded results, as one would expect values more in line with the more desirable outcomes of higher frequency and confidence.
This study is the first investigation seeking to assess family physician attitudes toward running gait retraining. The major barrier preventing more widespread implementation of this beneficial treatment modality seems to be lack of physician knowledge on how to educate patients on where gait retraining is best clinically applied. In light of this, both graduate and continuing medical education programs in family medicine may consider incorporation of training on gait retraining for RRI patients in their sports medicine curricula. This will not only improve the counseling provided to patients on the subject, but it will also empower family physicians to better identify which injury patterns would most benefit. Additionally, given lack of time as another important obstacle identified by respondents, investigations to develop simple and brief approaches to gait retraining that treat and prevent RRI would assist family physicians in practically incorporating gait retraining counseling in time- and resource-limited settings at the point of care. While patients seek and receive care from other medical providers for these injuries, particularly physical therapists,3,4 brief and simple interventions by family physicians could reduce the number of health care visits and providers needed to treat these common maladies.
Acknowledgments
The author thanks Dr Robert Oh for his mentorship in refining the survey questions, Dr Jennifer Thornton for invaluable assistance in data analysis, and the members of the USAFP Clinical Investigations Committee for the opportunity to participate in the 2019 USAFP Omnibus Survey project. The author thanks the Military Primary Care Research Network and their Fall 2019 Writing Round participants, as well as Dr Glynnis Knobloch, for their help in manuscript editing.
Presentations: This project was presented at the 2020 Uniformed Services Academy of Family Physicians Annual Meeting as a virtual podium presentation.
Disclaimer: The views expressed in this material are those of the author and do not reflect the official policy or position of the US Government, the Department of Defense, the Department of the Air Force, or the Uniformed Services University. The work reported herein was performed under United States Air Force Surgeon General-approved Clinical Investigation Number FDG20190014N.
References
- Yamato TP, Saragiotto BT, Lopes AD. A consensus definition of running-related injury in recreational runners: a modified Delphi approach. J Orthop Sports Phys Ther. 2015;45(5):375-380. doi:10.2519/jospt.2015.5741
- van Gent RN, Siem D, van Middelkoop M, et al. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41(8):469-480. doi:10.1136/bjsm.2006.033548
- Napier C, Cochrane CK, Taunton JE, Hunt MA. Gait modifications to change lower extremity gait biomechanics in runners: a systematic review. Br J Sports Med. 2015;49(21):1382-1388. doi:10.1136/bjsports-2014-094393
- Davis IS, Futrell E. Gait retraining: altering the fingerprint of gait. Phys Med Rehabil Clin N Am. 2016;27(1):339-355. doi:10.1016/j.pmr.2015.09.002
- Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011;45(9):691-696. doi:10.1136/bjsm.2009.069112
- Diebal AR, Gregory R, Alitz C, Gerber JP. Forefoot running improves pain and disability associated with chronic exertional compartment syndrome. Am J Sports Med. 2012;40(5):1060-1067. doi:10.1177/0363546512439182
- Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech (Bristol, Avon). 2012;27(10):1045-1051. doi:10.1016/j.clinbiomech.2012.07.011
- Allen DJ. Treatment of distal iliotibial band syndrome in a long distance runner with gait re-training emphasizing step rate manipulation. Int J Sports Phys Ther. 2014;9(2):222-231.
- Breen DT, Foster J, Falvey E, Franklyn-Miller A. Gait re-training to alleviate the symptoms of anterior exertional lower leg pain: a case series. Int J Sports Phys Ther. 2015;10(1):85-94.
- Barton CJ, Bonanno DR, Carr J, et al. Running retraining to treat lower limb injuries: a mixed-methods study of current evidence synthesised with expert opinion. Br J Sports Med. 2016;50(9):513-526. doi:10.1136/bjsports-2015-095278
- Roper JL, Harding EM, Doerfler D, et al. The effects of gait retraining in runners with patellofemoral pain: A randomized trial. Clin Biomech (Bristol, Avon). 2016;35:14-22. doi:10.1016/j.clinbiomech.2016.03.010
- Zimmermann WO, Linschoten CW, Beutler A. Gait retraining as part of the treatment programme for soldiers with exercise-related leg pain: preliminary clinical experiences and retention. S Afr J Sports Med. 2017;29(1):1-6. doi:10.17159/2078-516X/2017/v29i0a1923
- Bonacci J, Hall M, Saunders N, Vicenzino B. Gait retraining versus foot orthoses for patellofemoral pain: a pilot randomised clinical trial. J Sci Med Sport. 2018;21(5):457-461. doi:10.1016/j.jsams.2017.09.187
- Chan ZYS, Zhang JH, Au IPH, et al. Gait retraining for the reduction of injury occurrence in novice distance runners: 1-year follow-up of a randomized controlled trial. Am J Sports Med. 2018;46(2):388-395. doi:10.1177/0363546517736277
- Bramah C, Preece SJ, Gill N, Herrington L. A 10% increase in step rate improves running kinematics and clinical outcomes in runners with patellofemoral pain at 4 weeks and 3 months. Am J Sports Med. 2019;47(14):3406-3413. doi:10.1177/0363546519879693
- Davis IS, Tenforde AS, Neal BS, Roper JL, Willy RW. Gait retraining as an intervention for patellofemoral pain. Curr Rev Musculoskelet Med. 2020;13(1):103-114. doi:10.1007/s12178-020-09605-3
- Rendall EO, Mohtadi NG. Survey of competitive distance runners in Alberta: satisfaction with health care services with respect to running injuries. Clin J Sport Med. 1997;7(2):104-112. doi:10.1097/00042752-199704000-00006
- Smits DW, Huisstede B, Verhagen E, et al. Short-term absenteeism and health care utilization due to lower extremity injuries among novice runners: a prospective cohort study. Clin J Sport Med. 2016;26(6):502-509. doi:10.1097/JSM.0000000000000287
- Grimm PD, Mauntel TC, Potter BK. Combat and noncombat musculoskeletal injuries in the US military. Sports Med Arthrosc Rev. 2019;27(3):84-91. doi:10.1097/JSA.0000000000000246
Lead Author
Alexander C. Knobloch, MD, CAQSM
Affiliations: David Grant Medical Center Family Medicine Residency, Travis AFB, CA
Corresponding Author
Alexander C. Knobloch, MD, CAQSM
Correspondence: Family Medicine Residency Clinic, 60th Medical Group, 101 Bodin Circle, Travis AFB, CA 94535. 707-423-7339. Fax: 707-423-3501.
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.