Background and Objectives: Musculoskeletal (MSK) concerns constitute up to 40% of primary care outpatient visits. Despite Accreditation Council for Graduate Medical Education (ACGME) family medicine program requirements for musculoskeletal medicine and sports medicine training, previous studies have shown that family medicine residency graduates do not have adequate training to manage common musculoskeletal conditions. Factors for this may include deficiencies in education at both the undergraduate and graduate medical education training levels.
Methods: A Council of Academic Family Medicine Educational Research Alliance survey of 287 family medicine program directors assessed the current state of the delivery of musculoskeletal medicine education. Opinions were gathered on the scope and delivery of training requirements as well as potential areas for further curricular attention.
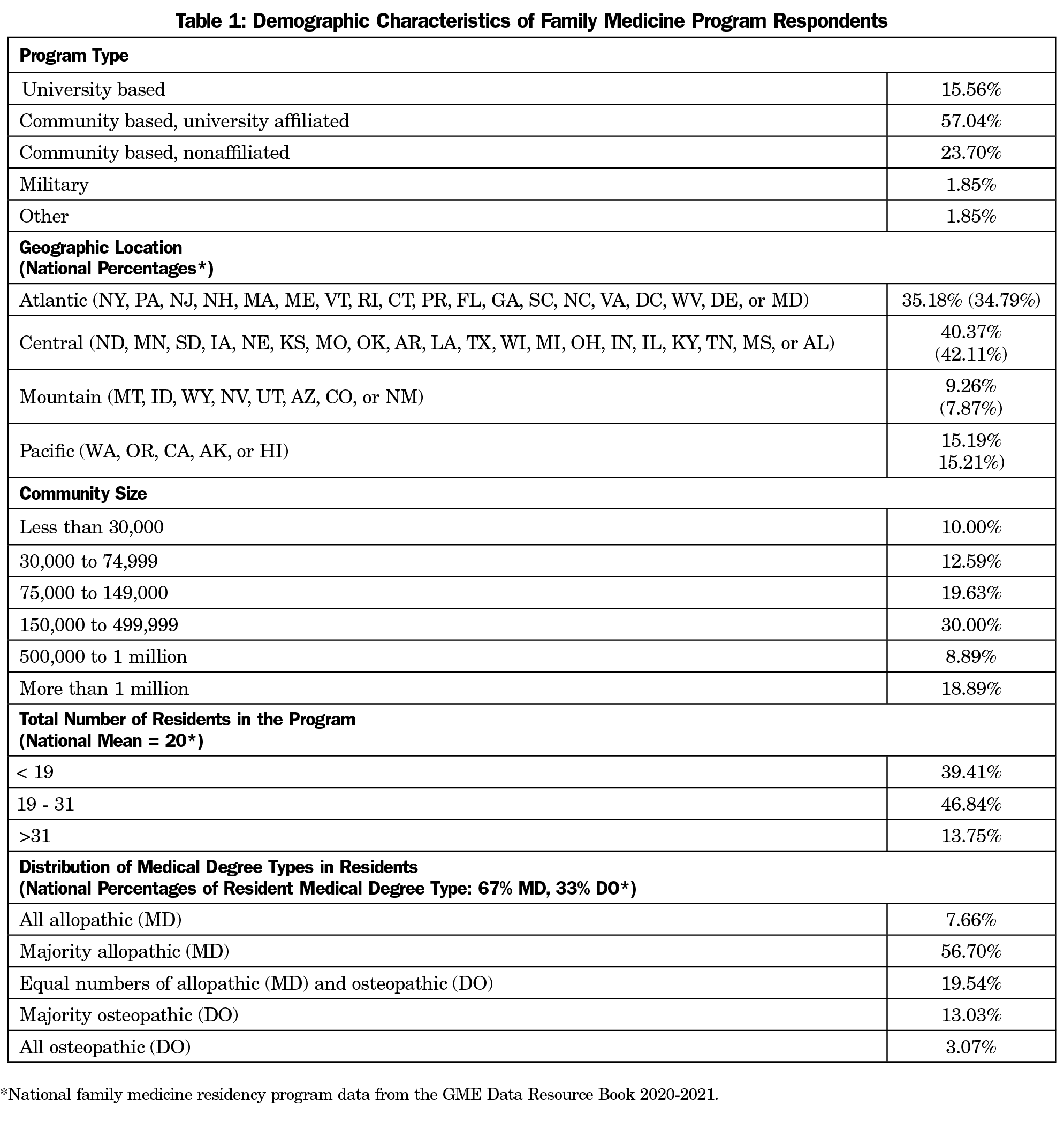
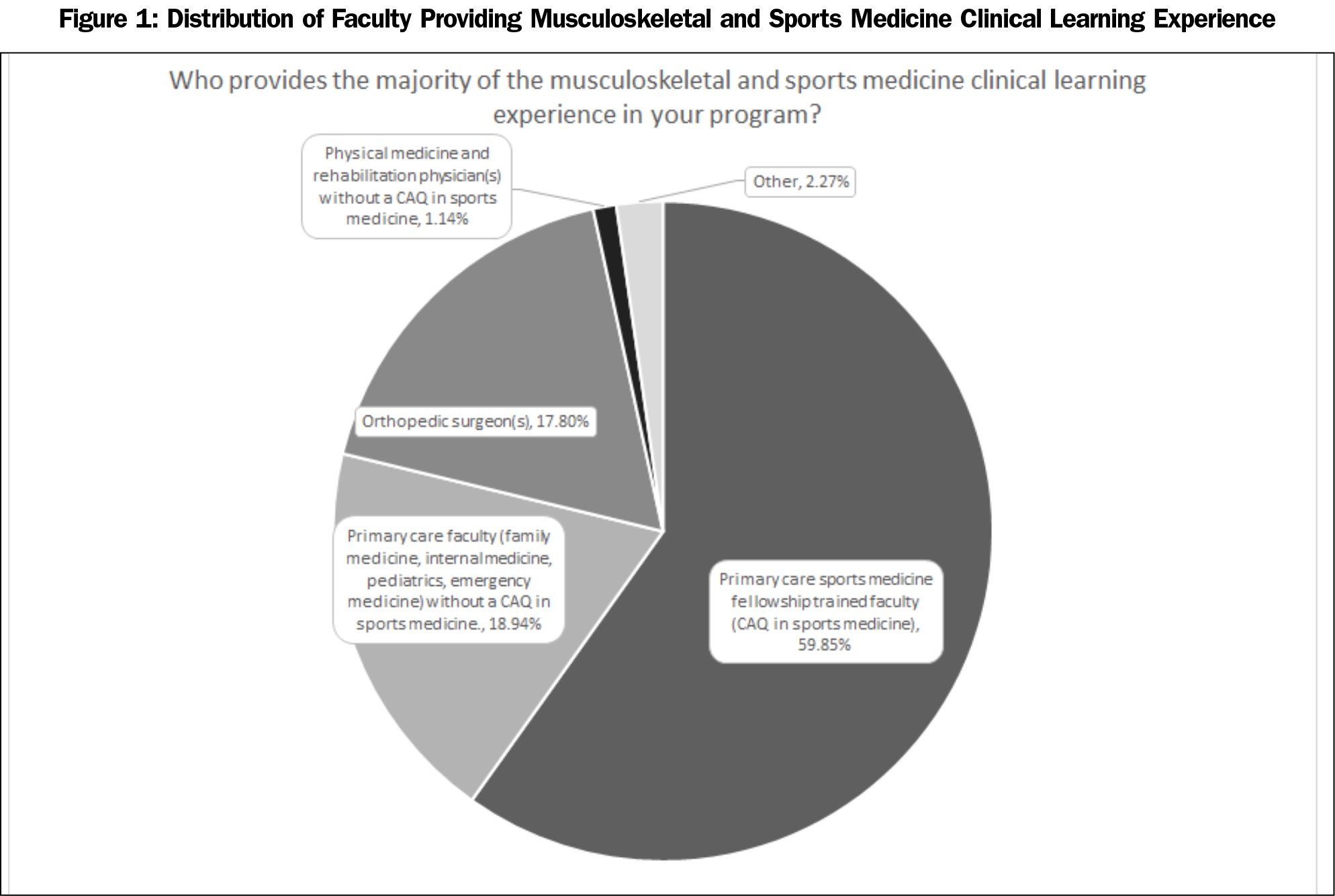
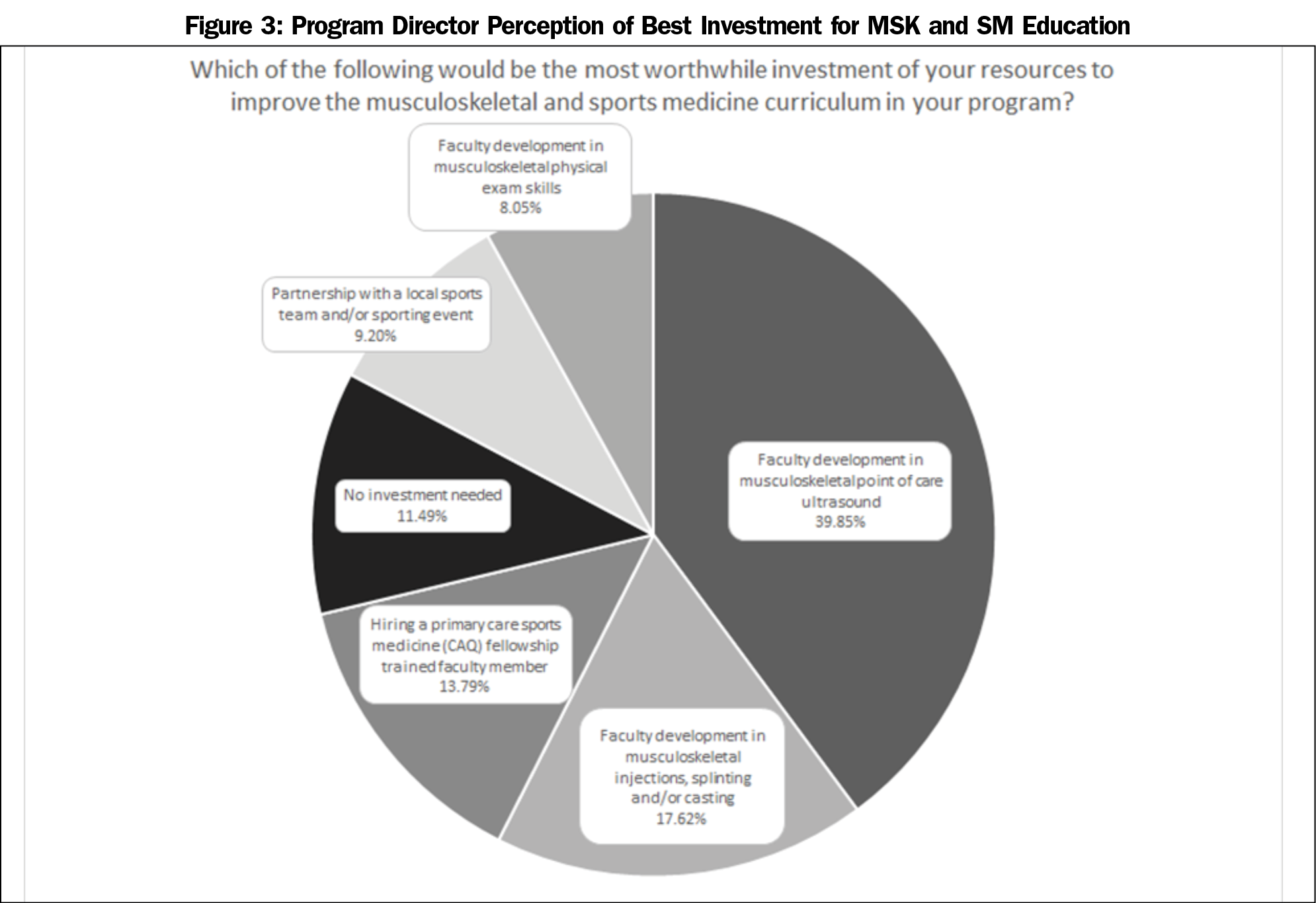
Results: Two hundred eighty-seven program directors responded to the survey (response rate 41.53%). Most (72.60%) were in university based or affiliated programs and had a fellowship-trained primary care sports medicine physician (59.85%) curricular lead. A majority (77.4%) did not feel that PGY-1 residents enter residency with the physical exam skills needed to evaluate common musculoskeletal (MSK) conditions , and most (81.15%) did not feel that there should be changes to the current ACGME requirements. An area highlighted for further investment is faculty development in point-of-care ultrasound (39.85%).
Conclusions: Although program directors believe that current ACGME MSK curricular requirements are likely appropriate, they do not feel residents arrive with the examination skills needed to evaluate common MSK conditions.Therefore, further attention can be given to medical student education in musculoskeletal exam skills prior to residency. Future research should develop objective measures using multiple assessors—students, residents, teaching faculty, and patients—to assess both the baseline and graduating competency in MSK medicine of our residents.
Knowledge of musculoskeletal (MSK) medicine is an important component of family medicine. The Accreditation Council for Graduate Medical Education (ACGME) requires family medicine residencies to provide training of either 200 hours or 2 months in duration for the care of MSK problems, including a structured sports medicine experience.1 Accordingly, the American Board of Family Medicine (ABFM) certification exam devotes 12% of the questions to MSK medicine, making it one of the three highest-tested subject areas along with the cardiovascular (12%) and respiratory (13%) systems.2 MSK complaints are the most common reason for outpatient appointments and constitute up to 40% of primary care visits.1,2
The American Medical Society for Sports Medicine (AMSSM) and American Academy for Family Physicians (AAFP) have developed curricular suggestions to develop competency in the diagnosis and management of MSK conditions during family medicine training.3,4 Other primary care specialties including pediatrics and internal medicine also have similar curricular recommendations.5,6 Specifically, the AMSSM recommends the education be longitudinal and training for the care of ambulatory MSK conditions be done primarily in the principal outpatient family medicine center. In 2021, subgroups from AMSSM published recommendations for MSK curricula for pediatric, internal medicine, and family medicine residents, agreeing that residents should demonstrate competence in MSK physical exam skills, interpretation of basic skeletal radiographs, joint aspiration and injection, and splinting and immobilization techniques at the time of graduation.3,5,6 Further details on the specifics joints and/or body areas to be covered are found in those manuscripts.
Despite these recommendations, many family medicine residency graduates do not feel comfortable evaluating and treating MSK conditions.6-8 Additionally, there are documented perceptions that primary care residents are not adequately trained to manage common musculoskeletal conditions.7-9 This is not unique to family medicine; a study in an internal medicine residency10 found that a majority of the examinees failed to demonstrate basic competency in MSK exam. Another study on pediatric residents also showed they had limited exposure to MSK training, and none of them passed a competency examination.7 Surveyed pediatric residents cite teaching of joint examinations and the preparticipation physical as the most poorly-taught components of physical examination.10 Interestingly, the presence of primary care sports medicine (PCSM) trained faculty within a program, the number of sports injuries a resident had been exposed to in the continuity clinic, and the presence of sports injury-specific clinics did not appear to influence trainees’ knowledge and comfort level in treating common sports injuries.11
Previous studies revealed that MSK medicine training is inadequate at both the undergraduate and graduate medical education level for nonorthopedic trainees.12 Many studies focused on medical student knowledge of MSK medicine have revealed that medical school graduates do not receive adequate MSK education, with fewer studies specifically examining the state of MSK education at the family medicine residency level.13-15
This study aimed to identify characteristics of MSK curricula within family medicine residency programs and identify any perceived gaps in ACGME recommendations for MSK curricula. We hope this information can be used to identify areas where MSK education can be improved for current and future trainees.
The survey questions were part of a larger omnibus survey conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA). The methodology of the CERA Program Director Survey has previously been described in detail.16 The CERA Steering Committee evaluated questions for consistency with the overall subproject aim, readability, and existing evidence of reliability and validity. Pretesting was done on family medicine educators who were not part of the target population. Questions were modified following pretesting for flow, timing, and readability. The American Academy of Family Physicians Institutional Review Board approved the project in April 2021. Data were collected from April 14 to May 17, 2021.
The sampling frame for the survey was all ACGME-accredited US family medicine residency program directors as identified by the Association of Family Medicine Residency Directors. Email invitations to participate were delivered with the survey utilizing the online program SurveyMonkey. Four follow-up emails to encourage nonrespondents to participate were sent weekly after the initial email invitation and a fifth reminder was sent 2 days before the survey closed. There were 699 program directors at the time of the survey; eight had previously opted out of SurveyMonkey surveys.
The final survey included questions about the current educational leads of musculoskeletal curriculum within programs, presence of musculoskeletal workshops in programs, and opinions on if current ACGME requirements for musculoskeletal medicine training are adequate. A 5-point Likert scale was used to survey perceptions of elements in musculoskeletal and procedural training, including the importance of longitudinal clinical experience, joint injections, MSK radiograph interpretation, fracture management, and event coverage. Program directors were also asked about needs for faculty development within their respective programs and the distribution of medical degree types in the residents of their program.
We calculated descriptive statistics using Microsoft Excel. We assessed bivariate tests of association via simple logistic regression using the software program R, version 4.0.5, and we estimated odds ratios from model beta coefficients. We set statistical significance at a=0.05.
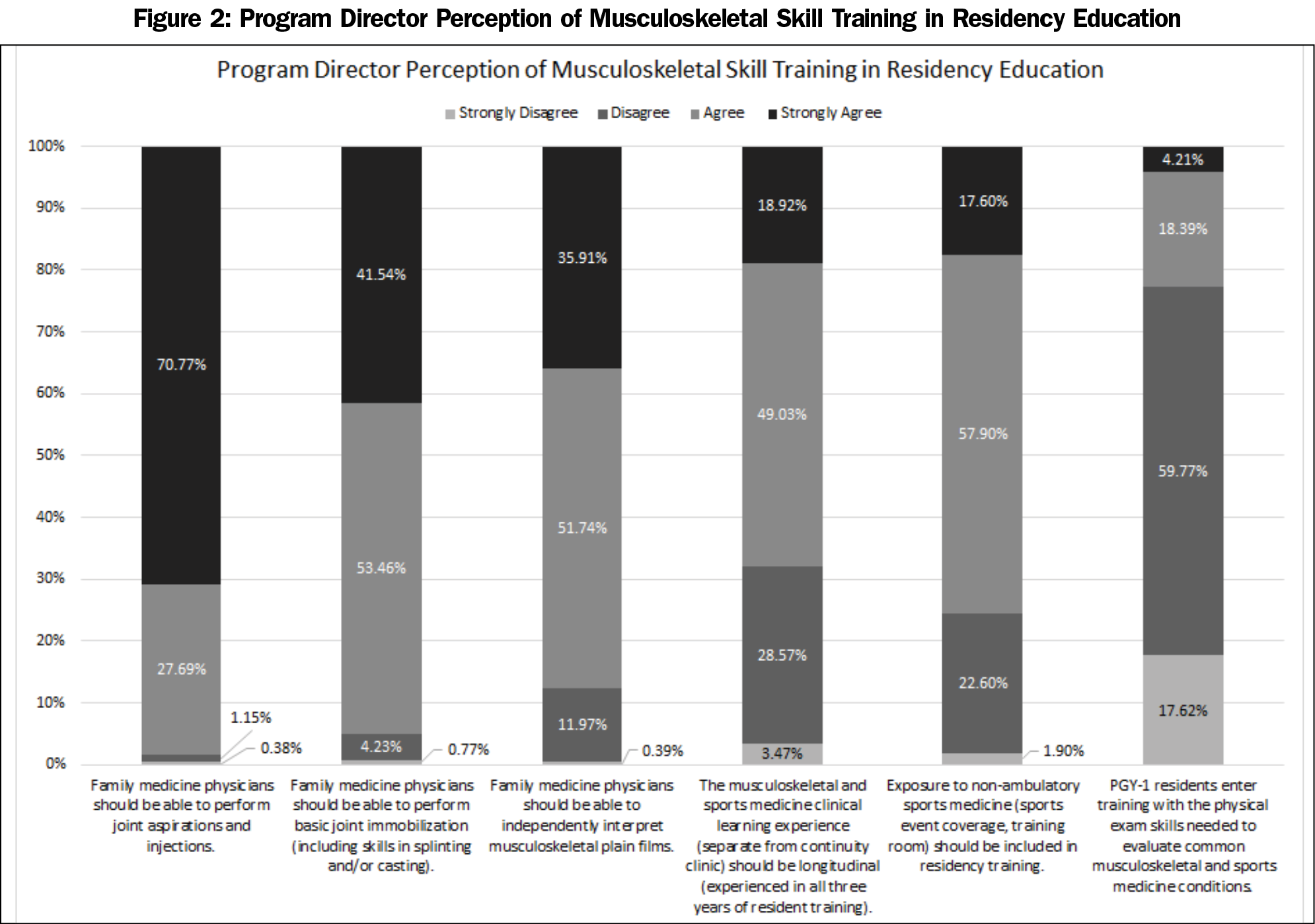
The overall response rate from FM program directors was 41.53% (287/691). A majority of the programs that responded were associated with a university (72.60%), whether university based (15.56%) or university affiliated (57.04%). Most of the remaining programs were community based (23.7%, Table 1); 59.85% of the programs stated that their MSK and SM education is led by a fellowship trained PCSM physician, with 18.94% of programs having their curriculum led by a non-certificate of added qualifications (CAQ) certified primary care faculty (Figure 1). Almost all (98.84%) of the directors responded affirmatively to having longitudinal curricular components for MSK workshops within the residency curriculum. There were no associations between who provides the majority of MSK curriculum (CAQ vs non-CAQ lead) and use of longitudinal curriculum, hours devoted to didactic teaching each year, or perceived scope of practice. Additionally, a majority of program directors (81.15%) responded that no change to the current ACGME requirements for MSK residency training requirements are needed, with 6.54% advocating for more required time and 12.31% wanting less.
Figure 2 outlines the responses from program directors regarding specific skills in MSK medicine that family physicians should have. A majority of program directors agree that family physicians should be able to perform joint aspirations and injections (98.46% agree/strongly agree), perform basic joint immobilization (95.00%), and independently interpret MSK plain films (87.65%). Additionally, there was agreement that MSK and sports medicine learning experiences should be longitudinal across resident training (67.95%) and exposure to nonambulatory sports medicine experiences, such as event coverage or training room experience, should be included in residency training (75.5%). Regarding PGY-1 residents’ prior training, 77.39% of program directors disagreed or strongly disagreed that PGY-1 residents enter training with the physical exam skills needed to evaluate common MSK and sports medicine conditions.
When asked which curricular components would be the best investment for improving an MSK curriculum, the most popular response was faculty development in MSK point-of-care ultrasound (POCUS, 39.85%) followed by faculty development in MSK procedural skills, including injections, splinting, and/or casting (17.62%, Figure 3).
Residents were perceived to enter residency training with insufficient skills and knowledge to manage common MSK conditions (Figure 2). A bivariate analysis demonstrated that program directors with an osteopathic medical degree (vs allopathic) had a strong correlation with the perception of adequate musculoskeletal exam skills of the residents entering their program (OR 5.51, P<.001). Program directors with osteopathic medical degrees (52.3%) perceived incoming interns as more prepared than program directors with allopathic medical degrees (16.6%) did. Additionally, the directors of programs with more osteopathic residents were more likely to perceive their incoming interns as adequately trained in musculoskeletal exam skills (OR 2.33, P<.001). While programs with a larger proportion of osteopathic residents are more likely to have an osteopathic program director (OR 5.78, P<.001), when controlling for the degree of the program director, having a greater proportion of osteopathic residents was still associated with a perception that PGY-1 residents enter training with the physical exam skills needed to evaluate common MSK and sports medicine conditions (adjusted odds ratio 1.86, P=.002). Though when adjusting for distribution of resident degree types in the program, compared to allopathic program directors, osteopathic program directors still overall perceived that incoming PGY-1 residents were better prepared (OR 2.48, P=.035).
Residency Curriculum
This survey of program directors suggests that overall, the current time recommendations for MSK curriculum are perceived as appropriate and that no significant changes in the amount of dedicated curriculum time are needed. Additionally, there are no reported differences in the hours devoted to didactic teaching per year, use of a longitudinal curriculum or perceived scope of practice, regardless of whether a non-PCSM physician was the lead of a program’s musculoskeletal curriculum. There is a general agreement among PDs that the skills of performing joint aspirations and injections, performing basic joint immobilization, and interpretation of MSK plain films should be in the toolbox of all family physicians. Also, longitudinal MSK experiences and event coverage should continue to be included in residency education. However, there remain opportunities to enhance the delivery of MSK education in all levels of medical training. While the surveyed program directors do not think changes to the current MSK curriculum time requirements are appropriate in the context of the overall training requirements, we cannot directly extrapolate this to mean that they think the current requirements are sufficient to produce proficiency in MSK medicine.
Medical School Graduate Preparedness
Our survey shows that 77.39% of program directors surveyed felt that PGY-1 residents enter postgraduate training with inadequate MSK physical exam skills. A study by Freedman and Bernstein has suggested that 80% of graduates from even the best medical schools were deficient in basic MSK medicine.13 Despite prior efforts in MSK curriculum reform in medical schools, further mandatory training and validated assessment of competence is needed. Prior efforts have clarified what MSK exam skills to teach but more efforts are needed to understand how to teach these skills for better retention.3,5,6
The survey results also show a possible gap between allopathic and osteopathic medical school graduates in perceived preparedness to perform the MSK physical exam techniques necessary to evaluate common musculoskeletal and sports medicine issues. Program directors with more osteopathic residents in their programs were more likely to agree that their residents entered training with adequate skills to evaluate MSK problems, regardless of the program director’s degree type. However, osteopathic program directors were more likely to agree that their incoming residents were better prepared regardless of the distribution of medical degree types in the program. Previous literature has outlined differences in allopathic versus osteopathic MSK training, with osteopathic students stating that their MSK curriculum better prepared them than their allopathic counterparts.17 One of the largest factors that may contribute to this are osteopathic curricula’s inclusion of manipulative techniques within their undergraduate curricula. However, previous studies have also indicated that both osteopathic and allopathic students fare only marginally differently in basic competencies of MSK medicine when given a standardized exam.12
Faculty Development
Our study also highlights the need for more faculty development. The two faculty development areas in which PDs would most like to invest resources are MSK POCUS (39.85%) and MSK injections, splinting, and casting (17.62%). It is interesting that the most common area where programs would like to make investment is in MSK POCUS, an area not currently included in the ACGME program requirements. Furthermore, while POCUS is an emerging clinical tool in teaching clinics, use in clinical settings remains limited with significant barriers being a lack of trained faculty, access to equipment, and comfort independently interpreting images without radiology review.18 As more faculty attend training in POCUS, some of these barriers should decrease. A POCUS curriculum is also not included in all family medicine residency programs. A potential solution to meet this curricular gap may be through a dedicated MSK ultrasound curriculum, similar to what the American Medical Society for Sports Medicine has created for sports medicine fellows19 and following the AAFP recommendations for a POCUS curriculum.20 It should be noted, however, that in the absence of faculty with good baseline knowledge of anatomy and musculoskeletal exam and procedural skills, MSK POCUS is likely to be difficult to teach or utilize in a clinical setting.
Limitations
Our study has several limitations. First, this is a cross-sectional survey of family medicine program directors from primarily academic institutions regarding their perception of the current state of MSK education in their respective residency program. This survey does not assess the specific skills developed or adequacy of the common program requirements to develop family medicine providers who are competent in providing appropriate care for MSK conditions after graduation. Our survey also does not provide outcome data or gauge resident comfort or ability in caring for common outpatient MSK conditions.
Future Directions
One strength of our study is the large number of program directors surveyed, from different geographic areas and program sizes, on the current state of MSK curriculum within family medicine residency programs. Further research should be conducted to understand if the current models of MSK curriculum consistently result in clinical competency to provide this important component of primary care. Specifically, looking at what factors are associated with a higher level of competence upon graduation, such as MSK faculty program role, presence of other MSK focused training programs, and curricular structure for longitudinal experiences. Another opportunity for further research is understanding the difference between allopathic and osteopathic MSK education at the medical school level in preparing students for practice in residency. Steps to answer this question could include looking at what measures are used by programs to assess the preparation of incoming PGY-1 residents and how residents are assessed over time. Additionally, curriculum development focusing on the development of specific competencies related to MSK medicine, as opposed to time-based strategies, may allow for consistent skill development and address needed competencies for family medicine graduates. Surveys of core FM faculty, MSK faculty, and residents could be performed to gain a better understanding of perceived adequacy of current MSK curricula and competence in MSK medicine. This could then be compared to objective measures of competency, such as performance on MSK exam questions on board exams or MSK observed simulated clinical exams prior to graduation. Further delineation of the specific joints and body areas that program directors think are core to the practice of MSK procedures would also be beneficial to tailor the components of this part of the curriculum. Faculty could also be directly asked about their perceived needs for training in MSK medicine to help them better prepare residents for practice after graduation.
Our study is the first survey study assessing program director perspectives on the state of MSK education in family medicine residency programs. Despite the high prevalence of MSK disorders in primary care, physicians continue to receive inadequate education during their training years on this topic. Overall, family medicine residency program directors agree that PGY-1 residents do not enter residency with the physical exam skills needed to manage common MSK conditions, and perceive that current ACGME recommendations for MSK education are adequate and that no significant changes to current recommendations are needed. Program directors agree that certain skills in MSK medicine, such as joint aspirations, injections, and immobilization and MSK plain film interpretation should continue to be emphasized. Survey responses also showed program directors of programs with more osteopathic residents perceived their incoming trainees to be more prepared to manage MSK conditions than those with more allopathic residents. Areas for further attention include faculty development in the training and use of MSK POCUS and development of objective measures to assess both the baseline and graduating competency in MSK medicine of our residents. Given the volume of MSK issues that a family physician may encounter in daily practice, it is important that curricular outcomes be assessed at all levels of medical education, from undergraduate through graduate medical education to ensure provider competency in providing high-quality MSK care.
References
- ACGME Program Requirements for Graduate Medical Education in Family Medicine. Accreditation Council for Graduate Medical Education. Accessed August 23, 2021.https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_FamilyMedicine_2020.pdf
- American Board of Family Medicine Exam Blueprint. American Board of Family Medicine. Accessed August 23, 2021. https://www.theabfm.org/sites/default/files/inline-files/2020FMCOneDayExamBlueprint.pdf
- Brennan FH Jr, Rao AL, Myers RA, et al. Suggested curricular guidelines for Musculoskeletal and sports medicine in family medicine residency training. Curr Sports Med Rep. 2020;19(5):180-188. doi:10.1249/JSR.0000000000000713
- Recommended Curriculum Guidelines for Family Medicine Residents Musculoskeletal and Sports Medicine. AAFP Reprint No. 265. American Academy of Family Physicians. Accessed August 23, 2021. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint265_Musculo.pdf
- Coleman N, Beasley M, Briskin S, et al. Musculoskeletal and sports medicine curriculum guidelines for pediatric residents. Curr Sports Med Rep. 2021;20(4):218-228. doi:10.1249/JSR.0000000000000830
- Liddle DG, Changstrom B, Senter C, et al. Recommended musculoskeletal and sports medicine curriculum for internal medicine residency training. Curr Sports Med Rep. 2021;20(2):113-123. doi:10.1249/JSR.0000000000000811
- Haywood BL, Porter SL, Grana WA. Assessment of musculoskeletal knowledge in primary care residents. Am J Orthop. 2006;35(6):273-275.
- Matheny JM, Brinker MR, Elliott MN, Blake R, Rowane MP. Confidence of graduating family practice residents in their management of musculoskeletal conditions. Am J Orthop. 2000;29(12):945-952.
- Bonds DE, Mychaleckyj JC, Watkins R, Palla S, Extrom P. Ambulatory care skills: do residents feel prepared? Med Educ Online. 2002;7(1):4536. doi:10.3402/meo.v7i.4536
- Demorest RA, Bernhardt DT, Best TM, Landry GL. Pediatric residency education: is sports medicine getting its fair share? Pediatrics. 2005;115(1):28-33. doi:10.1542/peds.2004-0266
- Amoako AO, Amoako AB, Pujalte GG. Family medicine residents’ perceived level of comfort in treating common sports injuries across residency programs in the United States. Open Access J Sports Med. 2015;6:81-86. doi:10.2147/OAJSM.S71457
- Stockard AR, Allen TW. Competence levels in musculoskeletal medicine: comparison of osteopathic and allopathic medical graduates. J Am Osteopath Assoc. 2006;106(6):350-355.
- Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84(4):604-608. doi:10.2106/00004623-200204000-00015
- Watts SA, Zhang Z. Competency in musculoskeletal and sports medicine: evaluating a PGY-1 curriculum. Fam Med. 2011;43(9):659-663.
- Day CS, Yeh AC. Evidence of educational inadequacies in region-specific musculoskeletal medicine. Clin Orthop Relat Res. 2008;466(10):2542-2547. doi:10.1007/s11999-008-0379-0
- Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med. 2018;16(3):257-260. doi:10.1370/afm.2228
- Sabesan VJ, Schrotenboer A, Habeck J, et al. Musculoskeletal education in medical schools: a survey of allopathic and osteopathic medical students. J Am Acad Orthop Surg Glob Res Rev. 2018;2(6):e019. doi:10.5435/JAAOSGlobal-D-18-00019
- Hall JWW, Holman H, Barreto TW, et al. Point-of-care ultrasound in family medicine residencies 5-year update: a CERA study. Fam Med. 2020;52(7):505-511. doi:10.22454/FamMed.2020.223648
- Hall MM, Bernhardt DT, Finnoff JT, et al. American Medical Society for Sports Medicine sports ultrasound curriculum for sports medicine fellowships. Clin J Sport Med. 2021;31(4):e176-e187. doi:10.1097/JSM.0000000000000944
- Family medicine residency curriculum guidelines. Point-of-care ultrasound. American Academy of Family Physicians. Accessed March 4, 2022. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf
- ACGME Data Resource Book Academic Year 2020-2021. Accreditation Council for Graduate Medical Education. Accessed March 4, 2022. https://www.acgme.org/about-us/publications-and-resources/graduate-medical-education-data-resource-book/



There are no comments for this article.