The Commonwealth Fund’s periodic report of the performance of 11 high-income countries’ health care systems has recently been released for 2021. Once again, despite spending far more than any other country in the world, the United States still ranks last in terms of access to care, equity, and outcomes of care.2 It is well known that we have long-standing racial and ethnic disparities and inequities, but it is useful now to reassess what is going on. This article has three goals: (1) to bring some historical perspective to these problems, (2) to assess their extent today, and (3) to consider what can be done, within today’s polarized and still-prejudiced political landscape, to redress this long-standing systemic problem.
SPECIAL ARTICLES
Disparities and Inequities in US Health Care:
Alive and Sick
John P. Geyman, MD
Fam Med. 2022;54(9):688-693.
DOI: 10.22454/FamMed.2022.576797
Disparities and inequities based on ethnic and racial differences have been a part of health care in America from the time of its founding. These disparities have persisted through recurrent efforts to reform our health care system. This article brings historical perspective to what has become a systemic part of US health care; examines the extent of disparities today as they impact access, quality, and outcomes of care; and considers what can be done within our polarized political environment to eliminate them. It is hoped that this can help to spark dialogue within our discipline on these matters of critical importance. A single-payer national health insurance program, whereby all Americans can access affordable care based on medical need instead of ability to pay, can help to move our current nonsystem toward health equity. This change can bring improved health care to all Americans with simplified administration, cost containment, and less bureaucracy. It can be financed through a progressive tax system whereby 95% of Americans pay less than they do now and receive more in return.
The past is never dead. It’s not even past.1
—William Faulkner
Racial disparities, of course, can be dated back some 4 centuries to the arrival of the slave ships from Africa, when Blacks were first brought here to be owned and worked by White plantation owners, mostly in the South. At the same time, however, racist laws were being enacted and implemented in the North. The plight of Blacks did not improve much for centuries thereafter. At the close of the Civil War in the mid 1860s, quarantine and vaccination were being used to prevent a smallpox outbreak from razing the Union Army, but were not extended to Blacks.3 As historian Jim Downs wrote in his 2012 book, Sick from Freedom, White leaders were afraid that free and healthy African Americans would upend the existent racial hierarchy. Although Congress later established the medical division of the Freedmen’s Bureau to address the health crisis across the war-torn south, few physicians were sent there, and their pleas for equipment and personnel were ignored.4
A 2020 publication from the Southern Poverty Law Center (SPLC), The Year in Hate and Extremism 2020, described “patriarchal violence” as the basis for centuries of oppression of enslaved Black people in this country. As one example of the cruelty of this violence, Dr James Marion Sims gained notoriety for carrying out many forced sterilizations through mass hysterectomies on enslaved Black women without consent or anesthesia and with high mortality rates.5 That is just one example of the many medical atrocities conducted on both slaves and freedmen that included experimental exploitation.6
Slow forward to the 1930s, when Congress and the administration of President Franklin D. Roosevelt passed a range of New Deal programs, including Social Security, labor laws, and the GI bill. Blacks, however, were marginalized and left out when the programs were administered locally in states and communities, where those administering them were usually White. Ira Katznelson, professor of political science and history at Columbia University, described how this happened in his 2005 book, When Affirmative Action Was White: An Untold History of Racial Inequality in Twentieth Century America. As he noted about the GI bill:
The GI bill did create a more middle-class society, but almost exclusively for whites. Written under southern auspices [southern Democrats were the dominant force in Congress], the law was deliberately designed to accommodate Jim Crow. Its administration widened the racial gap.7
The story was no better within organized medicine. The American Medical Association (AMA) barred Black doctors, medical schools excluded Black students, and most hospitals and clinics segregated Black patients. As a result, they were sicker and died earlier than their White counterparts. In response, Black communities created their own health systems and professional organizations, including the National Medical Association (NMA), which pushed health care as a human right and a national health plan in direct opposition to the AMA.8
The Tuskegee experiment involving syphilis was a shameful part of the history of race in America from 1932 to 1972. It started by enrolling 600 African-American men in Macon County, Georgia into a study of the full progression of the disease. Most were sharecroppers and many had never visited a doctor. The US Public Health Service conducted the study, informing those with latent syphilis that they were being treated for “bad blood,” but instead were only given placebos, even after penicillin became the recommended treatment in 1947. By the time the “study” was shut down in 1972, 28 participants had died from syphilis, and more than 100 others had passed away from related complications.9
The January 6, 2021 insurrection at the US capitol ignited renewed attention to White supremacy as a persistent sickness in our society, which is far more common and cross-generational than many think, even including Black indigenous people of color, some of whom align with Whiteness in order to gain access and opportunities.10
Systemic racism, based on long-standing views of White supremacy among many Whites, has persisted through the years to contemporary society. Today, these views are continued through institutional policies, including residential segregation, voter suppression, mass incarceration, and social norms that involve using Whites as the reference group to which others are compared.11 Racial and ethnic minority groups are more vulnerable than Whites to the COVID-19 economic downturn by having lower-wage jobs, higher unemployment rates, to be uninsured, and to be living in poverty.12 The median household net worth of White households is about 10 times higher than that of Black households ($171,000 vs $17,500), and is a major cause of health inequities.13
Health inequities based on race stand as barriers to access to essential health care. A recent national study found markedly lower rates for outpatient visits for Black, Hispanic and Asian/Pacific islander patients to most specialists in the majority of 29 states.14 A 2020 survey found that Black Americans, compared to their high-risk, non-Hispanic White counterparts, were 42% more likely to be at risk for COVID-19 and 51% more likely to have inadequate health insurance coverage.15 A 2021 study found that 29% of Black adults did not seek treatment for a health problem in the last year due to cost, and perhaps lack of trust, compared to 16% of Whites.16
Predictably, outcomes of care for Black and Hispanic Americans are worse than for Whites, in large part because of limited access to timely care. Even within the same hospitals, Black patients have higher rates of complications from surgical procedures compared to Whites.17 Compared to Whites, life expectancy for Black and Hispanic Americans declined by 3.25 years and 3.88 years, respectively, the largest decline since World War II.18 Blacks’ overall mortality rate for COVID-19 is 2.3 times higher than for Whites, and in some states up to four times higher.19 Maternal mortality rates are more than three times higher for Black women than Whites, together with a more than double infant mortality rate.20
Evelynn Hammonds, PhD, dean of Harvard College and professor of the history of science and of African and African-American studies at Harvard University, sums up this tragic story on the long history of racial disparities and inequities in the United States in these words:
There has never been any period in American history where the health of Blacks was equal to that of Whites. Disparity is built into the system. Medicare, Medicaid and the Affordable Care Act have helped to shrink those disparities. But no federal health policy yet has eradicated them.21
For many years there has been a bias within much of the medical literature against covering these unacceptable markers of systemic racism in US health care.22,23 It is a welcome change, however, that some medical journals are righting that wrong, such as the New England Journal of Medicine with its new section of “Race and Medicine.” This journal has already moved toward more coverage of systemic racism, as demonstrated by its collaborative statement in January 2021 with other editors of family medicine journals.24
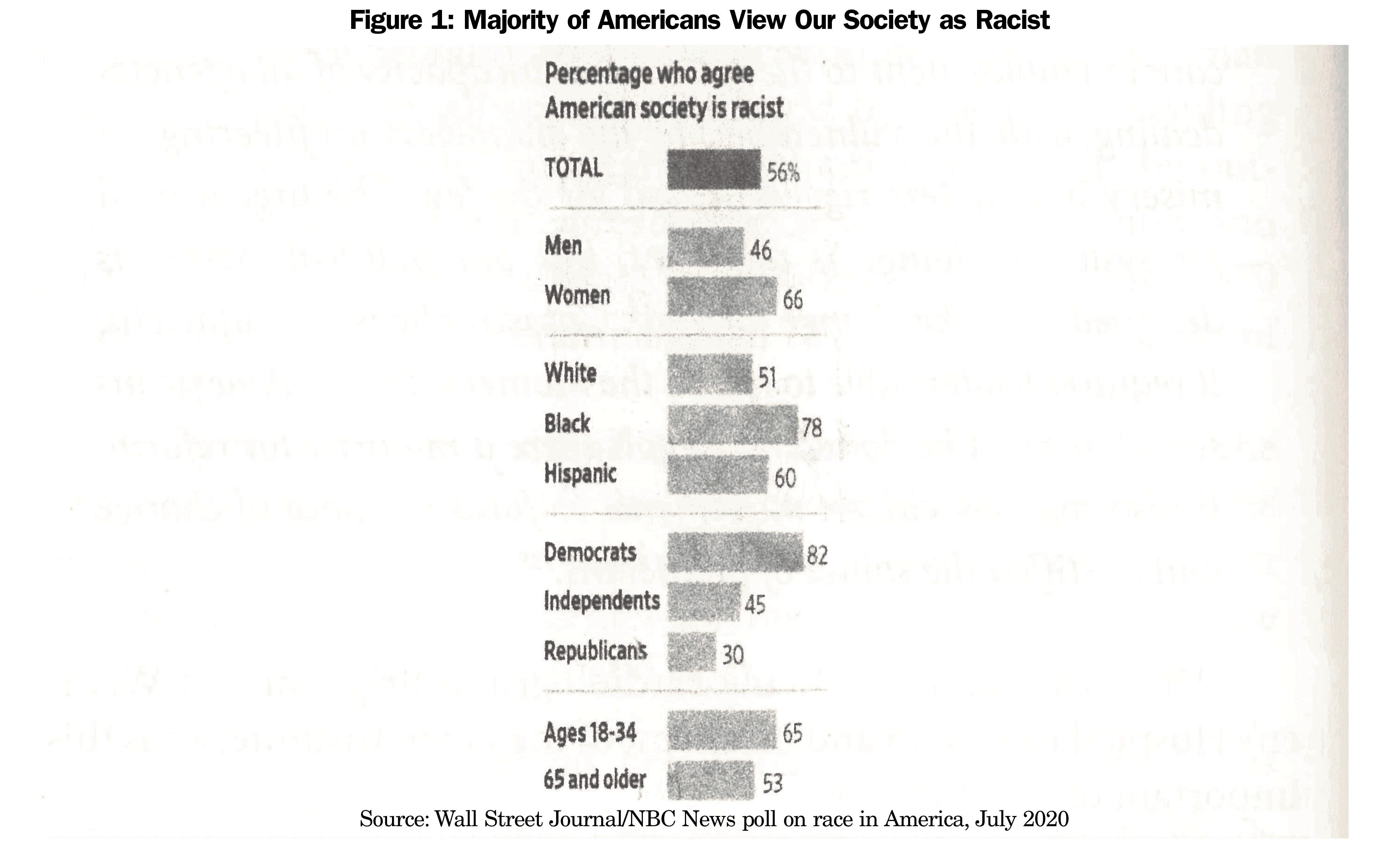
A majority of Americans view racism as a long-standing problem, with predictable differences along party lines, as shown in Figure 1.25
This observation helps us to understand the impacts of systemic racism on our health care system:
A health care system which neglects the poor and disenfranchised impoverishes the social order of which we are constituted. In a real (and not just hortatory) sense, a health care system is no better than the least well-served of its members.26
—Larry Churchill, PhD, ethicist at the University of Notre Dame and author of Rationing Health Care in America: Perceptions and Principles of Justice.
Difficult as it has been over so many decades to bring lasting reform to America’s increasingly dysfunctional system, it is rapidly becoming more urgent than ever as the racial divide widens. New census population projections predict that White people will represent a minority of voters by 2045.27 As we go through this transition, we can expect increasing cultural and political wars between Republicans, with many outspoken White supremacists in their midst, and Democrats split between moderates and progressives.
We have only to look at the last election to see how intense the battle over voting by minorities has already become. The Federal Communications Commission, as one example, has recently proposed a $5 million fine for right-wing operatives who made more than 85,000 robocalls targeting Black neighborhoods during the 2020 election. These calls falsely warned that mail-in voting carried the risk that voters’ personal information could be “used by police departments to track down old warrants and be used by credit card companies to collect outstanding debts.”28
In her 2020 book, The End of White Politics: How to Heal Our Liberal Divide, Zerlina Maxwell observes:
The change is already happening. This is the end of politics as we’ve known it in America. We’ve been doing white identity politics since America’s founding. We just called it politics. The white men booing in that room represent the past. They need to understand where we are going, so they don’t get left behind. The women and people of color are already getting in formation, and we aren’t going to be thrown off course.29
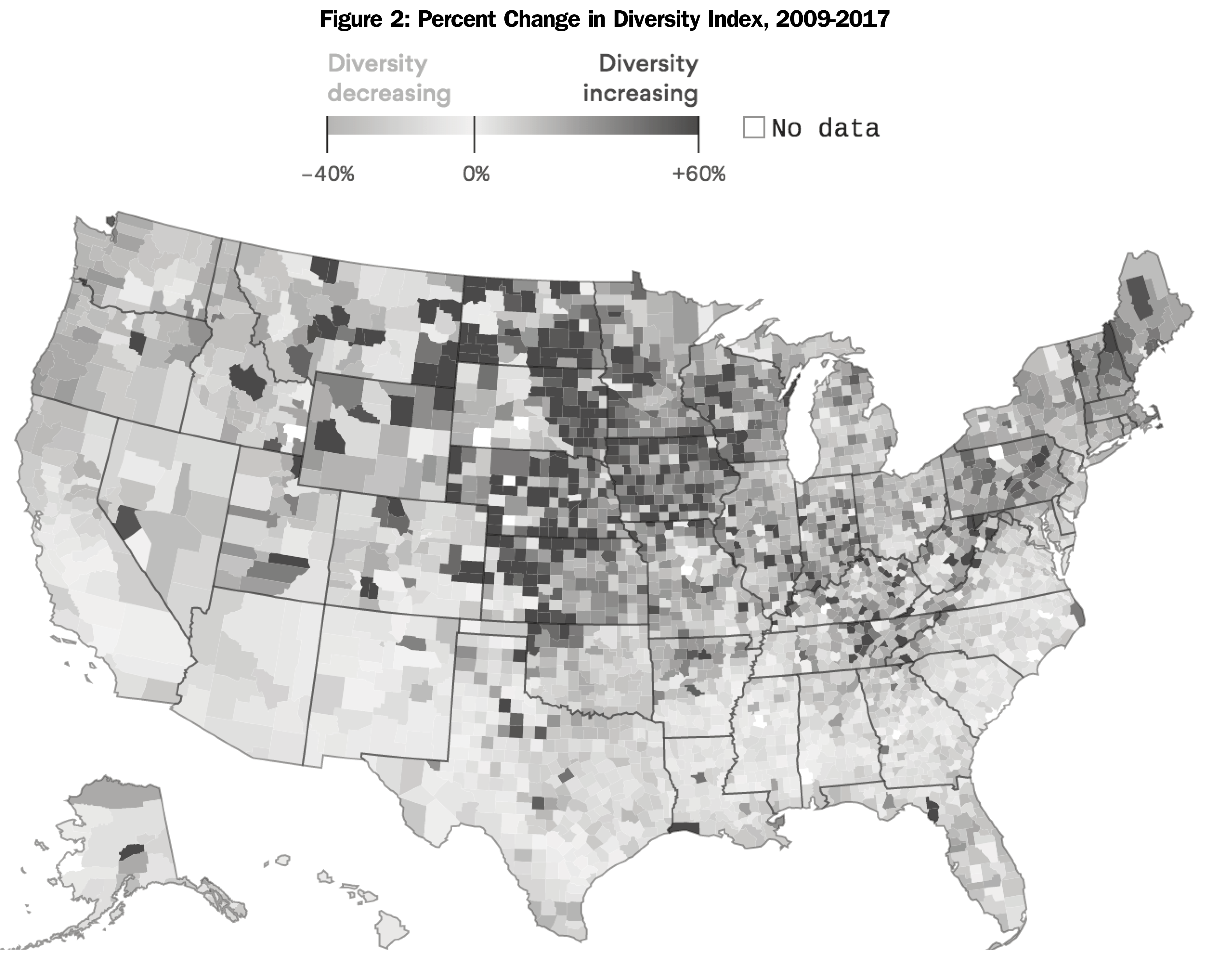
The 2020 census report found that the non-Hispanic White population declined for the first time in our nation’s history as racial diversity grew across the country, at the fastest pace in the Midwest. Figure 2 illustrates how this wave of change from 2010 to 2020 varies from one part of the country to another, based on a diversity index developed by the Wall Street Journal that measures the chance that two randomly selected people in the country’s more than 3,000 counties have different races and ethnicities.30
Thus, it comes as no surprise that voter suppression and gerrymandering have taken center stage in preparation for the 2022 and 2024 election cycles. In the Senate, Majority Leader Chuck Schumer observes:
Republican state legislators across the country are engaged in the most sweeping voter suppression in 80 years . . . Both major parties are vying to change who votes in America and how they cast ballots . . . Republicans often seek a more limited franchise. Democrats are seeking the opposite.”31
The new America First caucus started in the House of Representatives “to respect Anglo-Saxon political traditions” is blatantly racist, meaning White supremacy.32 The 2020 report from the Southern Poverty Law Center states that almost 40% of all active hate groups in the United States can be described as being rooted in White supremacy, and that they have disseminated sustained narratives of disinformation and conspiracy theories across the hard right for decades.33 Of further concern is the extent to which small states put the Republicans at an enormous advantage, with 52% of the country’s senators elected from small states with just 18% of the US population.34
Taking the longest view of inequality among people in his 2017 book, Great Leveler: Violence and the History of Inequality From the Stone Age to the Twenty-First Century, Walter Scheidel, professor of classics and history at Stanford University, offers these recommendations:
- “Income should be taxed in a more progressive manner, including capital gains as ordinary income and elimination of regressive payroll taxes, so that people with higher wealth pay more in taxes.
- Wealth should be taxed directly and in ways designed to curtail its transmission across generations.
- Corporations should be taxed on their global profits and hidden subsidies ended.
- Public policy should aim to boost intergenerational mobility by equalizing access to, and the quality of, schooling.
- Universal health care would protect lower-income groups from shocks in the costs of health care.”35
After decades of failing to deal effectively with the excesses, disparities, and inequities of our health care nonsystem, it is obvious that a larger role of government will be required in order to serve the needs of all Americans for affordable health care. Universal coverage to health care should become the foundation of needed reforms in the public interest. All Americans deserve to gain access to affordable care, based on medical need, not ability to pay. A reformed health care system should be based on the common good, not the profit-maximizing goals of our corporate stakeholders in our medical-industrial complex.
Traditional Medicare (not its privatized version Medicare Advantage) is a good model to build on. It has already demonstrated its ability to reduce racial and ethnic disparities in access to care and health.36 Another foundation to build upon is single-payer Medicare for All, as currently represented in the House of Representatives as HR 1976, with more than 112 cosponsors. When enacted, this would bring a new system of national health insurance for all US residents, with comprehensive benefits, and full choice of physicians and hospitals anywhere in the country. Its advantages include simplified administration, cost containment by negotiated fee schedules and global annual budgets for hospitals and other facilities, bulk purchasing of drugs and medical devices, elimination of cost sharing at the point of care, and sharing of risk for the costs of illness and accidents across our entire population of 330 million Americans.37
As documented above, racial and ethnic disparities and inequities have been a persistent pattern in this country with negative impacts on the health of individuals, families, and our population’s health. We remain an outlier among high-income countries around the world in not having a policy of universal coverage based on health care as a human right, and continue as last in international rankings of access to care, equity, and outcomes of care. Reform in the United States is long overdue, but it can be done if we gather the political will. As a lead specialty in primary care, family medicine and its organizations can play an important role in addressing the still-too-common racism in this country.
References
- Faulkner W. Requiem for a Nun. Random House; 1951:73.
- Schneider EC, Shah A, Doty MM et al. Mirror, Mirror 2021: Reflecting Poorly: Health Care in the U.S. Compared to Other High-Income Countries. Commonwealth Fund; August 4, 2021. Accessed June 22, 2022. https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly
- Interlandi J. Why doesn’t the United States have universal health care? The answer has everything to do with race. New York Times. August 14, 2019. Accessed June 22, 2022. https://www.nytimes.com/interactive/2019/08/14/magazine/universal-health-care-racism.html
- Downs J. Sick from Freedom. Oxford University Press; 2012:78-88. doi:10.1093/acprof:osobl/9780199758722.001.0001
- Bates L. Misogyny from the far right to the mainstream. In: Hankes K, Janik R. The Year in Hate and Extremism 2020. Southern Poverty Law Center; 2021:15.
- Washington HA. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. Penguin Random House; 2008.
- Katznelson I. When Affirmative Action Was White: An Untold History of Racial Inequality in Twentieth Century America. W. W. Norton & Company Inc; 2005:114.
- Interlandi J. Why doesn’t the United States have universal health care? The answer has everything to do with race. New York Times. August 14, 2019. Accessed June 22, 2022. https://www.nytimes.com/interactive/2019/08/14/magazine/universal-health-care-racism.html
- Nix E. Tuskegee experiment: the infamous syphilis study. National Archives. December 15, 2020. Accessed June 22, 2022. https://www.history.com/news/the-infamous-40-year-tuskegee-study
- Asare JG. 4 myths about white supremacy that allow it to continue. Forbes. January 14, 2021. Accessed June 22, 2022. https://www.forbes.com/sites/janicegassam/2021/01/14/4-myths-about-white-supremacy-that-allow-it-to-continue/?sh=399fa6277aac
- Gee GC, Ford CL. Structural racism and health inequities. Du Bois Rev. 2011;8(1):115-132. doi:10.1017/S1742058X11000130
- Radley DC, McCArth D, Hayes SL. Scorecard on State Health System Performance. The Commonwealth Fund; 2018. Accessed June 22, 2022. https://www.commonwealthfund.org/publications/scorecard/2018/may/2018-scorecard-state-health-system-performance
- McIntosh, K, Moss, E, Nunn, R et al. Examining the Black-White wealth gap. Brookings, February 27, 2020. Accessed June 22, 2022. https://www.brookings.edu/blog/up-front/2020/02/27/examining-the-black-white-wealth-gap/
- Cai C, Gaffney A, McGregor A, Woolhandler S, Himmelstein DU, McCormick D, Dickman SL. Racial and ethnic disparities in outpatient visit rates across 29 specialties. JAMA Intern Med. 2021 Nov 1;181(11):1525-1527. doi: 10.1001/jamainternmed.2021.3771
- Gaffney AW, Hawks L, Bor DH, Woolhandler S, Himmelstein DU, McCormick D. 18.2 million individuals at increased risk of severe COVID-19 illness are un- or underinsured. J Gen Intern Med. 2020;35(8):2487-2489. doi:10.1007/s11606-020-05899-8
- Witters D. In U.S., an estimated 46 million cannot afford needed care. Gallup. March 31, 2021. Accessed June 22, 2022. https://news.gallup.com/poll/342095/estimated-million-cannot-afford-needed-care.aspx
- Reyes EA. Same hospitals but worse outcomes for Black patients than for white ones. Los Angeles Times. July 20, 2021. Accessed June 22, 2022. https://www.latimes.com/world-nation/story/2021-07-20/black-patients-injuries-illness-surgery-same-hospitals
- Szabo, L. Black and Hispanic Americans suffer most in biggest U. S. decline in life expectancy since WW II. Kaiser Health News, June 24, 2021. Accessed June 22, 2022. https://khn.org/news/article/the-pandemic-will-undermine-american-health-for-years/
- Gawthrop E. The Color of Coronavirus. COVID deaths by race and ethnicity in the U.S. APM Research Lab. July 8, 2020. Accessed June 22, 2022. https://www.apmresearchlab.org/covid/deaths-by-race
- Artiga, S, Pham, O, Orgera, K et al. Racial disparities in maternal and infant health: An overview. Issue Brief. Kaiser Family Foundation. November 10, 2020. Accessed June 22, 2022. https://www.kff.org/report-section/racial-disparities-in-maternal-and-infant-health-an-overview-issue-brief/
- Schneider EC, Shah A, Doty MM et al. Mirror, Mirror 2021: Reflecting Poorly: Health Care in the U.S. Compared to Other High-Income Countries. Commonwealth Fund; August 4, 2021. Accessed June 22, 2022. https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly
- Krieger N, Boyd RW, De Maio F, Maybank A. Medicine’s privileged gatekeepers: Producing harmful ignorance about racism and health. Health Affairs Blog. April 20, 2021. Accessed June 22, 2022. https://www.healthaffairs.org/do/10.1377/forefront.20210415.305480/full/
- Wyatt R. The health-care industry doesn’t want to talk about this single word. The Washington Post. April 6, 2021. Accessed June 22, 2022. https://www.washingtonpost.com/opinions/2021/04/05/health-care-racism-medicine/
- Sexton SM, Richardson CR, Schrager SB, et al. Systemic racism and health disparities: A statement from editors of family medicine journals. Fam Med. 2021;53(1):5-6. doi:10.22454/FamMed.2020.805215
- Siddiqui S. Majority of Americans view society as racist, poll finds. The Wall Street Journal. July 21, 2020. Accessed June 22, 2022. https://www.wsj.com/articles/majority-of-voters-say-u-s-society-is-racist-as-support-grows-for-black-lives-matter-11595304062
- Churchill LR. Rationing Health Care in America: Perceptions and Principles of Justice. University of Notre Dame Press; 1987:103.
- Frey WH. The U.S. will become ‘minority white’ in 2045, Census projects. Brookings, March 14, 2018. Accessed June 22, 2022. https://www.brookings.edu/blog/the-avenue/2018/03/14/the-us-will-become-minority-white-in-2045-census-projects/
- Murdock S. FCC proposes $5 million fine for right-wing operatives Jacob Wohl and Jack Burkman. HuffPostst. August 24, 2021. Accessed June 22, 2022. https://www.huffpost.com/entry/fcc-fine-jacob-wohl-jack-burkman_n_6125607de4b0231e3695d1ad
- Maxwell Z. The End of White Politics: How to Heal Our Liberal Divide. Hachette Books; 2020:13.
- McCormick J, Overberg P. Where is America diversifying the fastest? Small midwestern towns. The Wall Street Journal. August 14, 2021. Accessed June 22, 2022. https://www.wsj.com/articles/where-is-america-diversifying-the-fastest-small-midwestern-towns-11628860161
- Rosenfield S. GOP threatens American democracy as Trumpers press for voter suppression. The Progressive Populist. August 1, 2021. Accessed June 23, 2022.
- Easley, J. House Republicans start white supremacy caucus as they aren’t even trying to hide their racism. Politicus USA, April 16, 2021. http://www.populist.com/27.13.Rosenfeld.html
- Bates L. Misogyny from the far right to the mainstream. In: Hankes K, Janik R. The Year in Hate and Extremism 2020. Southern Poverty Law Center; 2021:40.
- Thomas J. Analysis: 18% of the U.S. population elects 52% of the country’s senators. The Intellectualist. February 6, 2020. Accessed June 23, 2022. https://mavenroundtable.io/theintellectualist/news/analysis-18-of-the-u-s-population-elects-52-of-the-country-s-senators
- Scheidel W. Great Leveler: Violence and the History of Inequality from the Stone Age to the Twenty-First Century. Princeton University Press; 2017:432-433. doi:10.1515/9781400884605
- Wallace J, Jiang K, Goldsmith-Pinkham P, Song Z. Changes in racial and ethnic disparities in access to care and health among U. S. adults at age 65 years. JAMA Intern Med. 2021;181(9):1207-1215. doi:10.1001/jamainternmed.2021.3922
- Rogers S. Introducing the new (and improved) Medicare for All Act of 2021. Press release. Physicians for a National Health Program. Chicago, IL. March 17, 2021. Accessed June 23, 2022. https://pnhp.org/the-medicare-for-all-act-of-2021/
Lead Author
John P. Geyman, MD
Affiliations: Department of Family Medicine, University of Washington, Seattle, WA
Corresponding Author
John P. Geyman, MD
Correspondence: University of Washington - Family Medicine, 34 Oak Hill Drive , Seattle, WA 98250
Email: jgeyman@uw.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.