Background and Objectives: Our innovative, highly rated, interprofessional Primary Care Course (PCC) engaged learners in dentistry, medicine, nursing, physician assistants, pharmacy, public health, and social work. PCC used a low-resource, flexible classroom format, earned 99% high student ratings, and increased PC career plans in 56% of students. This study assessed changes in PC knowledge and attitudes and tracked PC career outcomes over 5 years.
Methods: We conducted before-and-after surveys of PCC students at baseline, 1-year, and 5-year follow-up, using anonymous online surveys. An additional controlled study compared PCC students with similar students from the course waitlist.
Results: Surveys yielded responses from 100% (84) at baseline, 81% (68) at 1 year, 57% (48) at 5 years, and 34% (28/83) among waitlist students at year 5. Before-and-after matched pairs analyses documented significant increases at year 1, sustained through year 5, in knowledge of PC training and referral patterns and attitudes toward PC value and role in future US health care. Precourse, 56% of students planned PC careers. At year 5, PCC graduates reported working in PC (74%, 29/39), delivering direct PC patient care (48%, 19/39), and working with underserved communities (74%, 29/39). The PC knowledge and attitudes of waitlist students at year 5 were similar to PCC student baseline scores and were significantly lower at year 5. Only 27% (7/26) of waitlist students reported working in PC at year 5.
Conclusions: PCC was associated with sustained increases in PC knowledge, attitudes, and careers across health professions. This low-resource, flexible format can contribute to building PC knowledge, attitudes, and workforce.
Personal and population health depends upon recruiting, training, and sustaining an adequate primary care (PC) workforce.1-3 Unfortunately, medical and other health professions students often choose careers in other specialties. Even those voicing early interest in PC often switch to other fields.4,5
Many programs aim to encourage students into PC. Although personal values and beliefs guide career choice, curricula can be influential.6 Some medical schools invest substantial resources in longitudinal mentorships and clinical experiences, but program evaluations typically measure short-term changes in attitudes; some track specialty choice at graduation.6-10
No published studies report longitudinal impact on PC knowledge, attitudes, and careers among learners in other health professions.
Our Primary Care Course (PCC) is a simple, flexible, low-cost classroom elective.11 Taught from a family medicine foundation, this interprofessional course engaged learners at all levels across seven health professional schools: dentistry, medicine, nursing, physician assistants, pharmacy, public health, and social work.
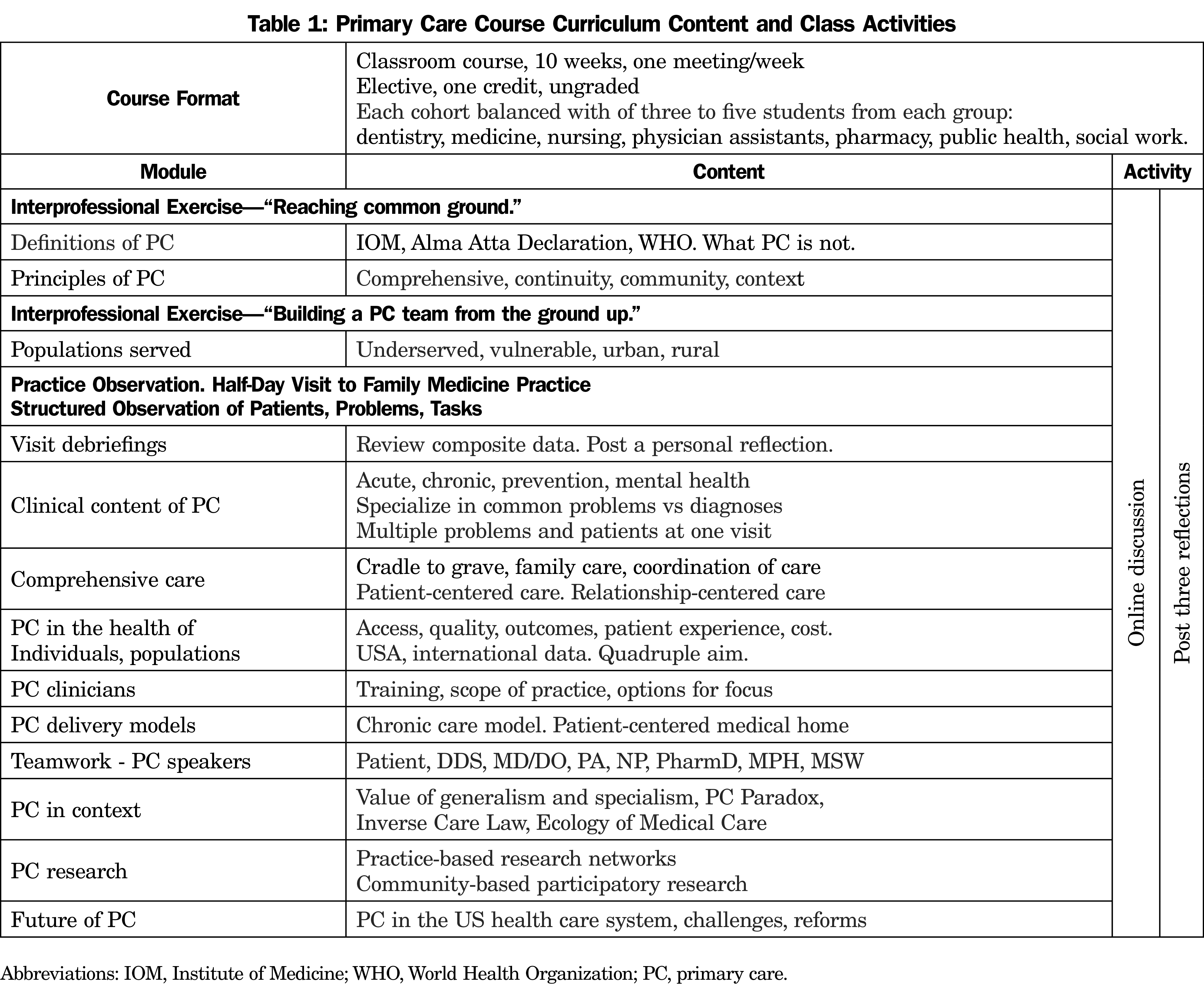
We described the PCC curriculum and evaluation in an earlier report (Table 1).11 Our end-of-course evaluation was positive: 99% of students rated it high value, 93% recommended it to others, and 41% advocated it be required for all students. Participants called the course “a life-changing experience,” and 56% reported it influenced them to plan PC careers.11
Three questions remain:
- Was the PCC associated with positive changes in PC knowledge and attitudes?
- Were observed changes sustained through training and into professional careers?
- Did early self-reported plans become PC careers?
We studied changes in PC knowledge, attitudes, and practice placements among PCC learners over 5 years into their professional careers.
We conducted a before-and-after study of the 84 students enrolled in the PCC over 3 years, 2013-2015, surveying each three times: at baseline (Y0), at 1 year following the course (year 1), and 5 years (year 5). Using Catalyst online survey software (Catalyst, University of Washington, Seattle), we contacted students by email with one reminder at 2 weeks and an incentive chance to win a $50 gift card. Responses were voluntary, anonymous, and required informed consent.
Questions based on the course outline addressed PC knowledge and attitudes. Students responded on 7-point Likert scales. We also asked about PC career plans and practice.
We compared each student’s responses in matched pairs across survey stages. For before-and-after change, we compared baseline to year 1; for sustained change, we compared baseline to year 5.
We tested for differences in paired categorical data with the Wilcoxon matched-pairs signed-rank test, a nonparametric test appropriate for nonequidistant Likert scales and non-Gaussian distributions. We tested for differences in paired analyses of continuous data with paired t tests. Based on matched-pairs design and positive course evaluations,11 we report P values and confidence intervals (CIs) without adjustment for multiple comparisons.
To confirm findings and address limitations of before-and-after design, we also conducted a separate controlled study, using these same methods, that compared PCC students with similar students who signed up and were waitlisted but never enrolled. We surveyed waitlist students just once at 5 years following the course. We tested differences between the waitlist and other groups with nonpaired analyses, using t tests for continuous data and Fisher’s exact test or χ2 test for categorical data.
To limit the popular class to a maximum of 35 students and balance participation across professional groups, we admitted students from a registration waitlist stratified by group. The mechanism was not statistically random; it differed slightly across groups and years to meet diversity goals. Course popularity led some students to reserve a spot early but later withdrew as their academic schedules finalized. Thus, there was no clear preference for early registration, but students in the course may have represented those with more persistent interest in PC.
This research was exempted by the University of Washington Human Subjects Division.
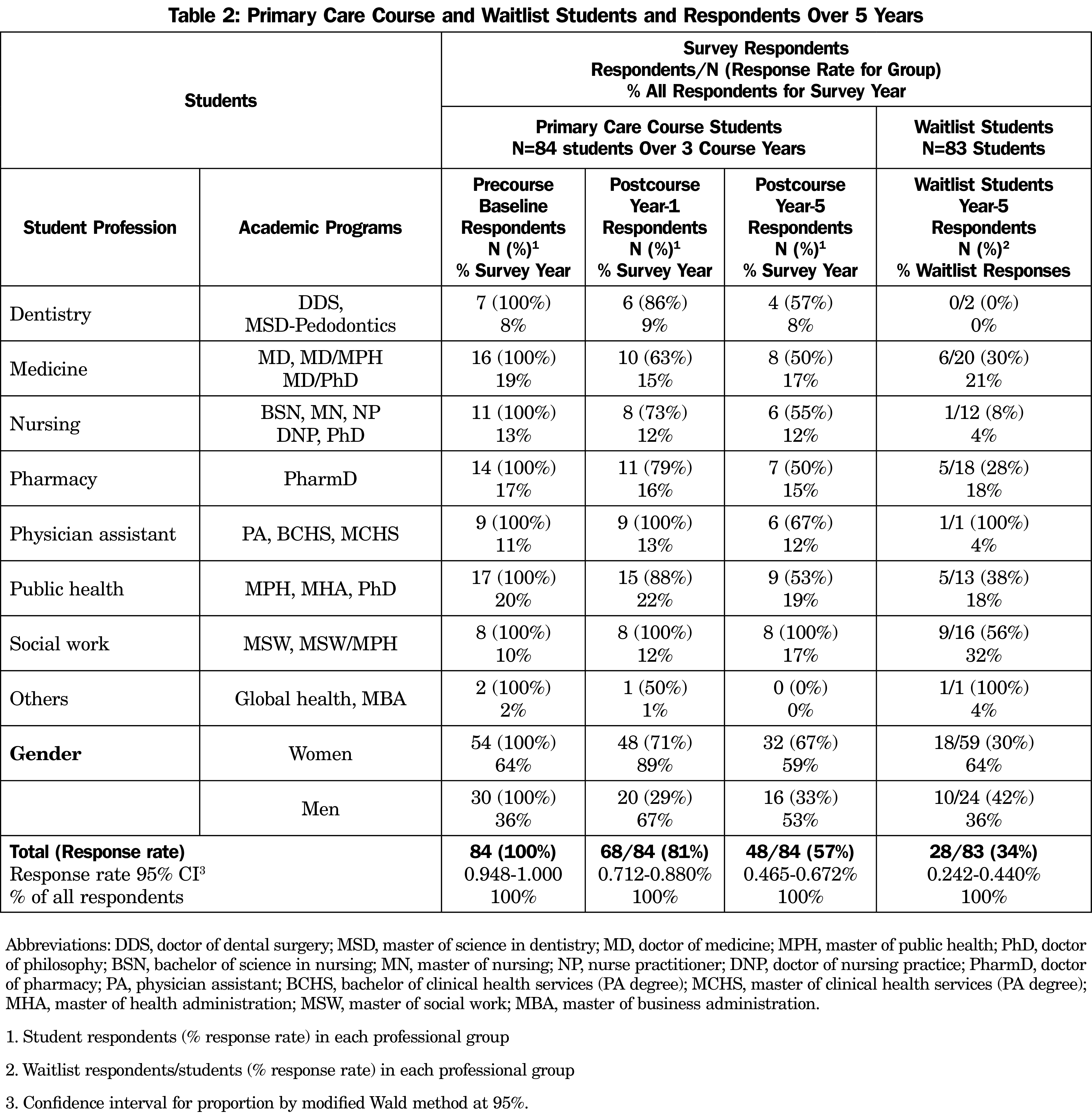
Our PCC student survey response rates were 100% (84) at baseline, 81% (68/84) at year 1, and 57% (48/84) at year 5 (Table 2). Waitlist response rate was 34% (28/83) overall and included all groups (range 8%-100%) except dentistry.
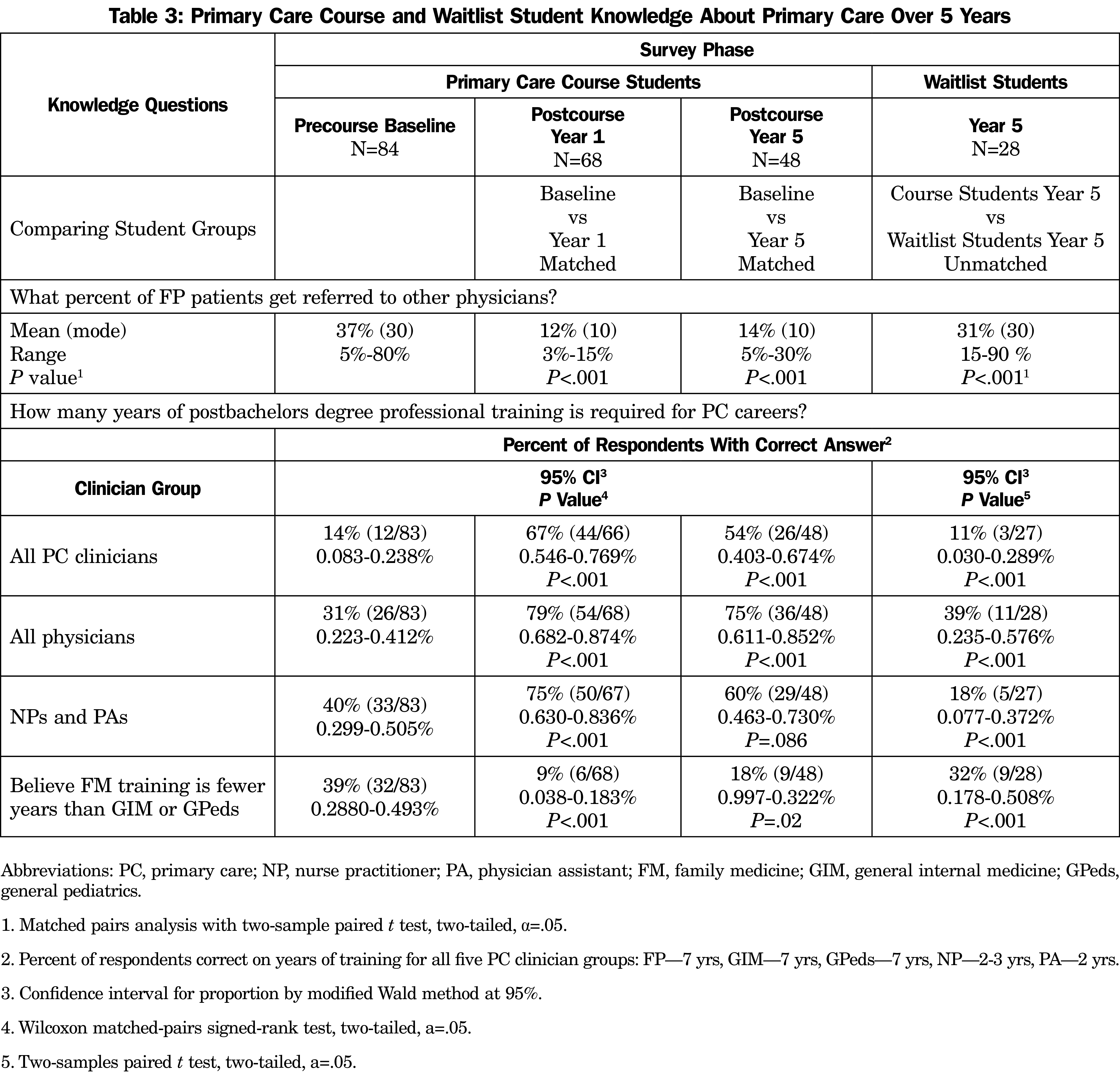
To check for responder bias, we compared response rates at year 5 and found no differences by gender or by initial plans for PC careers. PCC student knowledge increased from baseline to year 1 and was sustained through year 5 (Table 3).
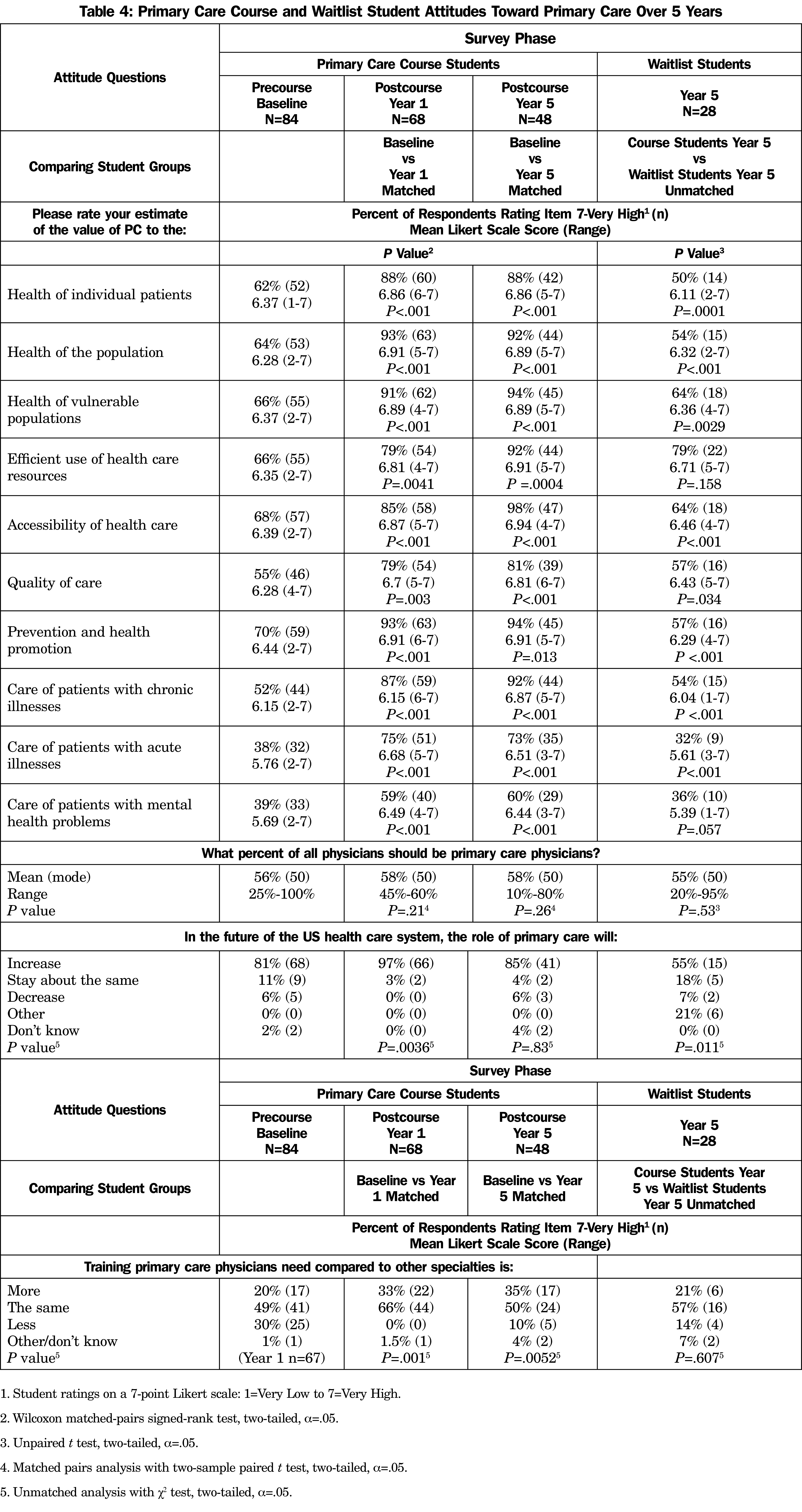
PCC student attitudes and estimates of PC value increased from baseline to year 1 and were sustained through year 5 (Table 4).
Waitlist students scored significantly lower on both PC knowledge and attitudes at year 5 (Tables 3 and 4); their year-5 scores were not significantly different from PPC students at baseline (data not shown).
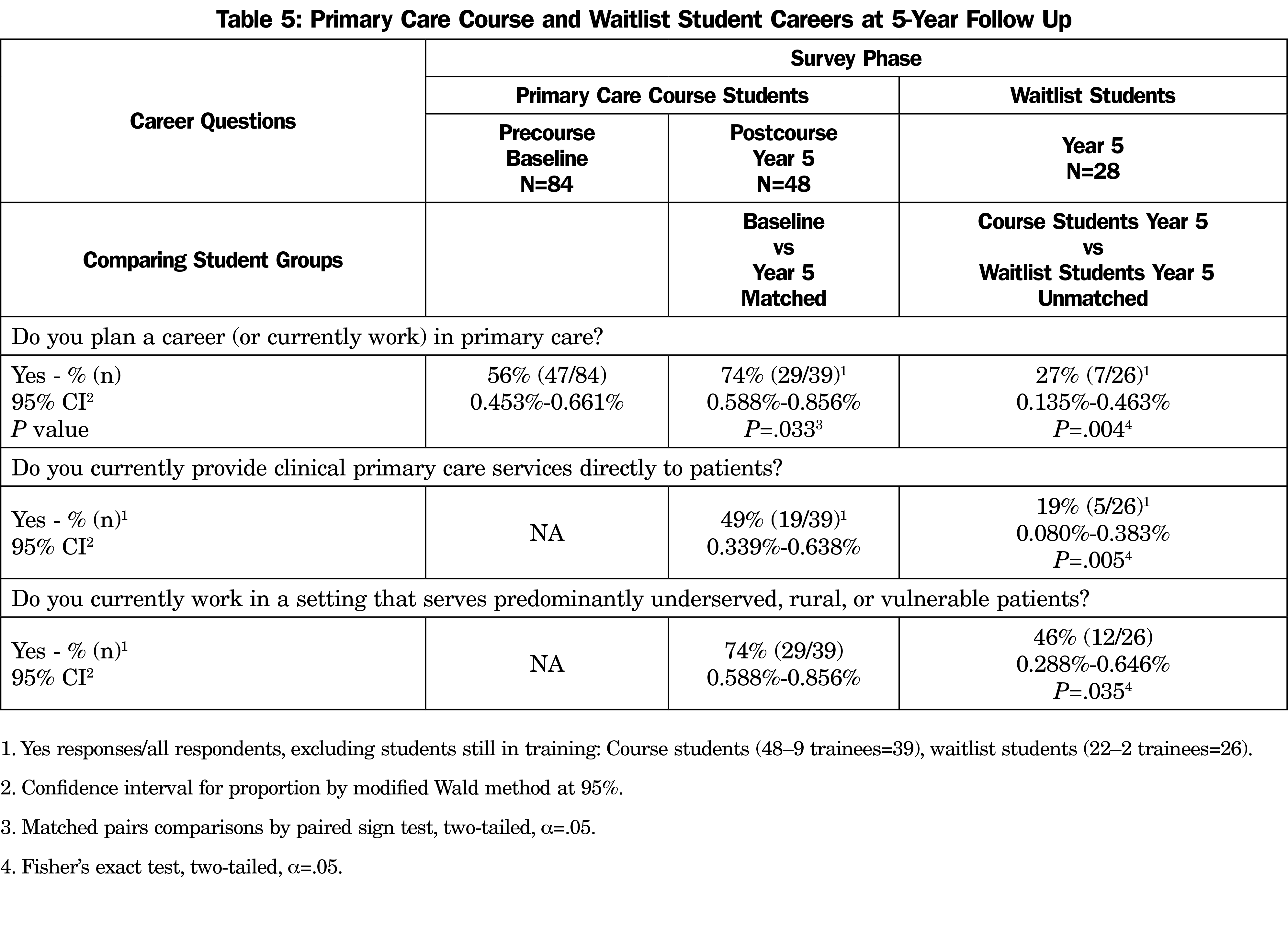
At baseline, 56% (47/84) of PCC students said they planned PC careers. At year 5, significantly more (74%) reported working in PC settings (29/39, 95% CI 0.588-0.856%, P<.033; Table 5). At year 5, 49% (19/39) reported providing clinical PC services directly to patients, and 74% (29/39) reported working in settings that serve predominantly underserved, rural, or vulnerable patients.
Compared to PCC students, waitlist students were less likely to report working in PC settings, delivering direct PC clinical services, or working with underserved, rural, or vulnerable patients (Table 5).
PCC students across professions and levels demonstrated increased PC knowledge and attitudes sustained over 5 years. Our waitlist study shows these gains did not occur in a comparison group of similar students who registered but did not attend.
We are unaware of previous reports of similar experience. Our PCC was a simple 10-week class that enrolled balanced cohorts of learners from seven professions. Our evaluation also assessed student career plans and outcomes at 1 and 5 years and added a controlled waitlist study. Our findings document increases in student entry into PC careers, not a falloff in student interest, as documented among medical students.4,5
Interpretation must consider study limitations. The course ran 3 years across multiple professional schools but only one institution. Influences on career choices are more complex than course experiences. Selection bias might influence which students choose the course, though our waitlist study offers some reassurance. We measured limited PC knowledge and attitudes. Likert scales cannot fully assess complex issues. Student answers skewed high on scales creating ceiling effects. Despite our high response rates, response bias was possible, particularly at the year-5 follow-up surveys, with 57% response rate for PCC students and 34% for waitlist students. The PCC highlighted positive attributes of PC, so social desirability bias might have influenced student responses. The questionnaire did not define “PC career” and relied on student self-report of their work settings, which may have differed between professional groups or over time. Survey anonymity prevented collection of detailed respondent information, and numbers were too small to allow subgroup analysis.
Further research should examine trajectories into PC careers for health professions students, especially nonphysicians. Longer follow-up studies should track graduates further into careers.
These findings document the potential of this interprofessional PCC model, which requires few resources and is more adaptable to educational challenges and opportunities than most clinical PC training programs. It is appropriate for all health professionals at all levels of training. We recommend this alternative to help recruit and prepare the PC workforce necessary to meet the needs of our patients and communities.
Acknowledgments
The authors thank Audrey Lew for course management, Jaime Grocock Fitch, MEd, for coordinating student activities, and Amanda Kost, MD, MEd, for manuscript critique.
Funding Statement: Dr Phillips was supported by the Theodore J. Phillips Professorship in Family Medicine. Part of his time was supported by the Helen Riaboff Whiteley Center, Friday Harbor Laboratories, University of Washington.
Previous Presentations: This study was previously presented as: Keys T, Phillips WR. Long-term impact of the University of Washington primary care course on primary care knowledge, attitudes, and careers across health professions. (Poster and oral presentation). Department of Family Medicine 50th Anniversary Annual Scholarship Forum. University of Washington; Seattle, WA. April 14, 2021.
References
- Phillips RL Jr, McCauley LA, Koller CF. Implementing high-quality primary care: a report from the National Academies of Sciences, Engineering, and Medicine. JAMA. 2021;325(24):2437-2438. doi:10.1001/jama.2021.7430
- Macinko J, Starfield B, Erinosho T. The impact of primary healthcare on population health in low- and middle-income countries. J Ambul Care Manage. 2009;32(2):150-171. doi:10.1097/JAC.0b013e3181994221
- Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005-2015. JAMA Intern Med. 2019;179(4):506-514. doi:10.1001/jamainternmed.2018.7624
- Compton MT, Frank E, Elon L, Carrera J. Changes in U.S. medical students’ specialty interests over the course of medical school. J Gen Intern Med. 2008;23(7):1095-1100. doi:10.1007/s11606-008-0579-z
- Deutchman M, Macaluso F, Chao J, et al. Contributions of US medical schools to primary care (2003-2014): determining and predicting who really goes into primary care. Fam Med. 2020;52(7):483-490. doi:10.22454/FamMed.2020.785068
- Pfarrwaller E, Sommer J, Chung C, et al. Impact of interventions to increase the proportion of medical students choosing a primary care career: a systematic review. J Gen Intern Med. 2015;30(9):1349-1358. doi:10.1007/s11606-015-3372-9
- Ford CD, Patel PG, Sierpina VS, Wolffarth MW, Rowen JL. Longitudinal continuity learning experiences and primary care career interest: outcomes from an innovative medical school curriculum. J Gen Intern Med. 2018;33(10):1817-1821. doi:10.1007/s11606-018-4600-x
- Kost A, Benedict J, Andrilla CH, Osborn J, Dobie SA. Primary care residency choice and participation in an extracurricular longitudinal medical school program to promote practice with medically underserved populations. Acad Med. 2014;89(1):162-168. doi:10.1097/ACM.0000000000000075
- Zink T, Center B, Finstad D, et al. Efforts to graduate more primary care physicians and physicians who will practice in rural areas: examining outcomes from the university of Minnesota-duluth and the rural physician associate program. Acad Med. 2010;85(4):599-604. doi:10.1097/ACM.0b013e3181d2b537
- Chung C, Maisonneuve H, Pfarrwaller E, et al. Impact of the primary care curriculum and its teaching formats on medical students’ perception of primary care: a cross-sectional study. BMC Fam Pract. 2016;17(1):135. doi:10.1186/s12875-016-0532-x
- Phillips WR, Keys T. Interprofessional primary care course curriculum and evaluation. Fam Med. 2018;50(3):217-222. doi:10.22454/FamMed.2018.998057