Background and Objectives: The issue of declining empathy and increasing burnout among residents is of concern for most programs. Numerous studies have shown these changes in both medical students and residents. However, the sequence of empathy decline and increasing burnout is unresolved and most studies have been cross sectional. This paper reports an individually-paired longitudinal analysis intended to clarify the sequence of these changes.
Methods: Beginning in 2017, 35 family medicine residents across all 3 years of training at a rural program completed an established empathy survey and a previously-validated single burnout question at the start of each year and at the midpoint. First, the empathy score for each resident was aligned with the next following burnout measure, and then the reverse sequence was followed, with burnout aligned with the following empathy score.
Results: With 125 responses to 133 survey opportunities, we saw a 94% response rate. Empathy scores across residency years decreased slightly and then improved almost to baseline. However, the analysis of variance test for quadratic trend was not significant. The burnout measure increased significantly over the residency years (J-T Statistic=4.89, P<.001). The correlation of the empathy score changing first showed a nonsignificant correlation (Rs=-.150, P=.133). The Spearman’s ρ of the burnout measure changing first was significant (Rs=-.300, P=.006).
Conclusions: In this group of residents, changes in burnout occurred before changes in empathy. If further research supports this finding, residency programs could focus more on efforts to address burnout to mitigate decreases in empathy.
Most studies show a decline in measured empathy across the clinical years of medical school as well as residency.1–3 Burnout is generally characterized by depersonalization, emotional exhaustion, and loss of a sense of personal accomplishment, all leading to a rise in cynicism.4 The primary source of burnout in residency is seen as stemming from high job demands in the setting of low individual autonomy.5–7 The sequence of these changes is an unresolved issue. Some believe that physicians who connect too strongly with their patients might actually suffer worse burnout.4 The opposing view is that since empathy is viewed as protective against burnout, empathy must decrease before burnout increases.8
The most comprehensive review comparing empathy and burnout in medical professionals showed a negative relationship.9 All previous studies have been cross-sectional, and without a sequenced, paired longitudinal study, the issue of which comes first could not be addressed.9,10 Our study was designed to address this question of sequence.
Our residency, begun in 1971, is located in a town of 20,000 in a rural area in the upper Southeast United States, with six residents in each year, with no other residencies in town.11 The site is also host for our regional rural medical school campus, with the main campus in a metropolitan community 160 miles away.12
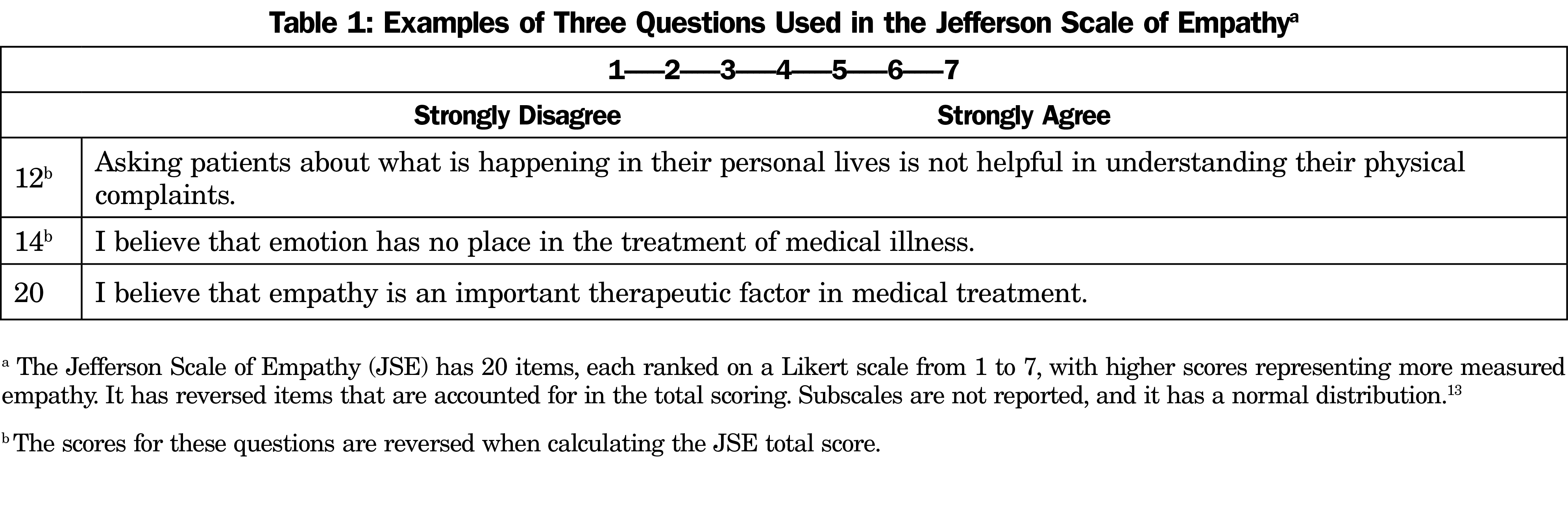
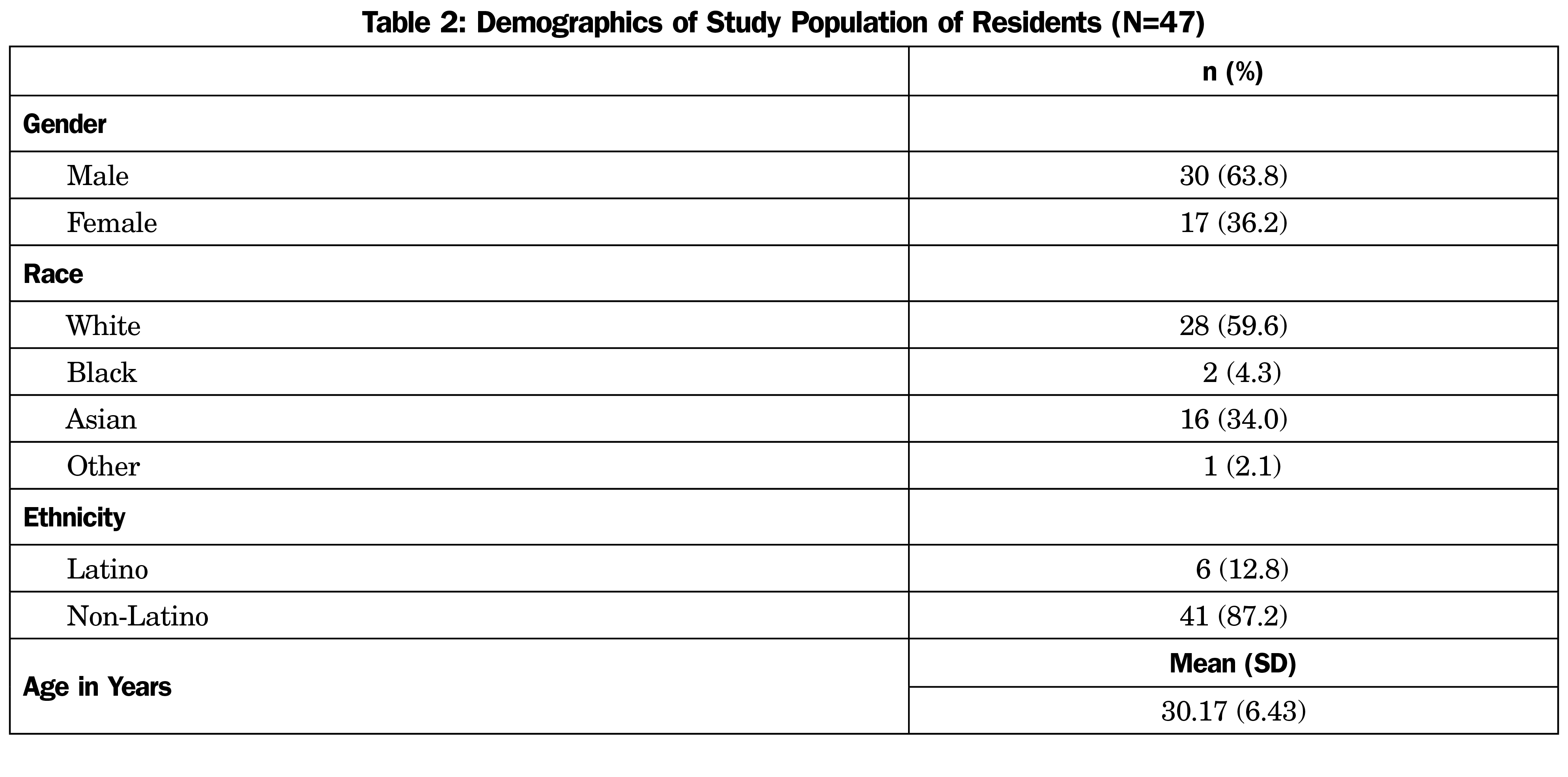
Beginning in 2016, 49 residents completed the empathy survey (Table 1)13 on paper during a regular administrative meeting just as the academic year began or ended, and at the midpoint of the academic year. A single burnout question was added to the back of the page in December 2017 that asked 35 residents to choose one of five statements reporting increasing burnout (Figure 1).14 We used the single-item burnout measure rather than the full Maslach Inventory to increase completion rate that has been reported to be a problem with the longer survey.9 Each survey was matched by individual resident. If a resident completed at least 1 full year (2 surveys) during the study period, regardless of training year, their data were included. Two resident empathy and burnout responses were excluded from the analysis for not following directions. The host hospital institutional review board designated the project as exempt.
First, for the empathy measure, we used analysis of variance where a polynomial test of quadratic trend was performed. For the burnout question, we performed a Jonckheere-Terpstra Test of linear trend. Next, the empathy score for each resident was aligned with the next following burnout measure. For example, a resident’s baseline empathy score was aligned with their midyear PGY-1 burnout measure and a resident’s midyear empathy PGY-1 score was aligned with their post PGY-1 burnout measure, and so forth. If significant, this would support that the empathy score changed first. A similar alignment was created where the resident’s burnout measure was aligned with the next following empathy score. If significant, this would support that the burnout measure changed first. After the alignment, a Spearman’s ρ was performed correlating empathy score with the following burnout measure, and correlating burnout measure with the following empathy score. We set significance at P<.05 and all tests were 2-tailed. We used SPSS version 27.0 for statistical analysis. We created figures with the R package GGPLOT.15
Of 133 opportunities to complete a survey, 125 responses were usable, for a response rate of 94%. Demographics are shown in Table 2. The empathy scores across the 3 residency years decreased slightly and then improved somewhat back to baseline. The ANOVA test of quadratic trend was not significant. Burnout measure increased significantly over residency years (J-T Statistic=4.89, P<.001; see Table 3 and Figure 1).
The correlation of the empathy score changing first showed a nonsignificant correlation (Rs=-.150 [95% CIs=-.33, .05], P=.133). The Spearman’s ρ of burnout measure changing first was significant (Rs=-.300, [95% CIs=-.49, -.09], P=.006).
Our longitudinal results clearly show that in our residents, burnout increases prior to any decrease in empathy. While methods to maintain empathy including reflective exercises such as composing narratives, participation in organized study of art, film, music and literature, and opportunities to learn and practice mindfulness may be useful,16 scarce residency resources and time may be better spent to address causes of burnout in the individual program. Focus groups with our residents prior to some recent program improvements showed that adequate sleep and minimizing administrative work unassociated with learning were ranked as most important overall, and first-year residents were concerned with learning a new electronic medical record and adapting to a new city.17
A recent national study of 2,509 family medicine residents showed that although burnout scores were not associated with in-training exam scores, they were correlated with failure to meet the professional conduct and accountability milestone. This study also reported that adequate salary given local cost of living is important.18 If our goal is to produce empathetic professionals, attention to local causes of burnout seems wise.
Limitations and Strengths
As with almost all previous reports on resident empathy and burnout, selection bias and limited generalizability are a concern with reports from a single site. Our findings should be generalized only to similar sites and similar residents. By using a standing meeting for survey administration, we achieved a 94% response rate compared to previous studies that had response rates of 35% to 80%.
Surveys produce quantifiable results, but with concepts as nebulous as empathy and burnout, focus groups are important. We have reported some results from this residency previously, and we will continue those efforts.17 We also invite other programs to replicate our studies and combine results across programs.
In our residents, changes in burnout occur prior to changes in empathy. If similar findings are reported in other sites, strengthened efforts to address program-specific sources of burnout may mitigate the decrease in empathy seen in some residents during training.
Acknowledgments
The authors recognize Debbie Peake, staff support in our residency, for her assistance in getting surveys completed on time.
References
- Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182-1191. doi:10.1097/ACM.0b013e3181b17e55
- Bellini LM, Shea JA. Mood change and empathy decline persist during three years of internal medicine training. Acad Med. 2005;80(2):164-167. doi:10.1097/00001888-200502000-00013
- Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82-85. doi:10.1097/00001888-200601000-00020
- Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99-113. doi:10.1002/job.4030020205
- Thomas NK. Resident burnout. JAMA. 2004;292(23):2880-2889. doi:10.1001/jama.292.23.2880
- Buck K, Williamson M, Ogbeide S, Norberg B. Family physician burnout and resilience: a cross-sectional analysis. Fam Med. 2019;51(8):657-663. doi:10.22454/FamMed.2019.424025
- Lebensohn P, Dodds S, Benn R, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45(8):541-549.
- Zenasni F, Boujut E, Woerner A, Sultan S. Burnout and empathy in primary care: three hypotheses. Br J Gen Pract. 2012;62(600):346-347. doi:10.3399/bjgp12X652193
- Wilkinson H, Whittington R, Perry L, Eames C. Examining the relationship between burnout and empathy in healthcare professionals: A systematic review. Burn Res. 2017;6:18-29. doi:10.1016/j.burn.2017.06.003
- Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7:763. doi:10.3389/fpsyg.2016.00763
- Martin D. A Short History of Trover Clinic with Commentary. Kuttawa, KY: McClanahan Publishing House; 1989.
- Crump WJ, Fricker RS, Ziegler CH, Wiegman DL. Increasing the rural physician workforce: a potential role for small rural medical school campuses. J Rural Health. 2016;32(3):254-259. doi:10.1111/jrh.12156
- Hojat M, Gonnella JS. Eleven years of data on the Jefferson Scale of Empathy-Medical Student Version (JSE-S): proxy norm data and tentative cutoff scores. Med Princ Pract. 2015;24(4):344-350. doi:10.1159/000381954
- Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75-79. doi:10.1002/smi.1002
- Wickham H. Elegant Graphics for Data Analysis Ggplot Website. Accessed February 3, 2021. https://ggplot2.tidyverse.org
- Hojat M. Ten approaches for enhancing empathy in health and human services cultures. J Health Hum Serv Adm. 2009;31(4):412-450.
- Crump W, Ziegler C, Fricker R. Does empathy really decline during residency training? A longitudinal look at changes in measured empathy in a community program. J Reg Med Campuses. 2021;4(4). doi:10.24926/jrmc.v4i4.4206
- Davis C, Krishnasamy M, Morgan ZJ, Bazemore AW, Peterson LE. Academic achievement, professionalism, and burnout in family medicine residents. Fam Med. 2021;53(6):423-432. doi:10.22454/FamMed.2021.541354





There are no comments for this article.