Background: The United States is facing a primary care physician shortage that is predicted to continue through the next decade. Determining why graduating medical students pursue a career in family medicine may inform efforts to help address this shortage.
Methods: Medical student responses to the Family Medicine Attitudes Questionnaire (FMAQ), a 14-item validated questionnaire developed to assess student attitudes toward family medicine, were collected at 16 US medical schools and compared to each institution’s proportion of graduates entering family medicine. We also analyzed subscales of the FMAQ, including attitudes toward family medicine lifestyle, research, importance, and shortages, with respect to student choice of family medicine. We used Pearson coefficients to calculate correlations.
Results: Student attitudes toward family medicine careers were strongly correlated with an institution’s proportion of graduates entering family medicine. Positive perceptions of family medicine research by students was the factor most strongly correlated with matching into a family medicine residency.
Conclusion: Strengthening students’ exposures and perceptions of family medicine and family medicine research may create viable opportunities for intervention by departments of family medicine and medical schools seeking to increase the number of graduates entering family medicine.
The ongoing shortage of primary care physicians in the United States is a multifactorial challenge that medical education has not yet effectively addressed. 1-4 Despite efforts to improve the primary care physician shortage, including increasing the number of Medicare-supported graduate medical education (GME) funded spots focused on underserved communities, 5 the Association of American Medical Colleges (AAMC) estimates a shortage of between 17,800 and 48,000 primary care physicians by 2034.5 The lack of primary care is not only driven by a shortage of training spots, but also an inadequate number of graduating US medical students interested in primary care careers. 6 Despite an increase in family medicine (FM) residency positions in the National Resident Matching Program (NRMP) match over the past 5 years, only one-third of available slots were filled by senior medical students graduating from US allopathic medical schools. 6 The America Needs More Family Doctors: 25x2030 initiative outlines strategies to help address this deficit, including pipeline development and fostering high-quality family medicine experiences for students. 7
The formal curriculum of a medical school is defined as the intended, official curriculum of an institution 8, 9 ; the informal curriculum is the values, competencies, and perspectives gained by medical students outside of intended institutional efforts, due to the educational environment. 8-11 Both formal and informal medical school curricula may influence primary care career choice. 12-14 Despite some understanding of how a medical school’s institutional characteristics 15 and curricular elements may influence specialty choice, 16, 17 there are very few multi-institutional studies that explore student attitudes toward family medicine and the influence of this milieu on students’ choice of family medicine careers.
The Family Medicine Attitudes Questionnaire (FMAQ) was developed and refined as a tool to assess students’ attitudes toward family medicine. 18-20 To explore the relationship between the attitudes of institutions’ students toward family medicine and the specialty choice of graduates, we analyzed medical schools’ collective FMAQ scores with respect to the proportion of each school’s graduates choosing family medicine. Exploring this relationship at the institutional level, rather than at the level of individual students, allows for a measure of institutional culture that has otherwise been difficult to study.
We examined the correlation of collective medical student attitudes (informal curriculum) with the proportion of graduates entering FM from 16 study institutions. We chose proportion of graduates entering FM alone as an indicator for PC career choice as the vast majority of FM matched graduates remain in primary care careers, while other specialties often included in PC groupings, such as internal medicine or pediatrics, have variable degrees of primary care career retention. 21, 22
To measure student attitudes toward family medicine on an institutional level, we deployed a secondary data analysis of data collected for the previously published validation study of the Family Medicine Attitudes Questionnaire. 18-20 The survey was originally sent to all students enrolled in 16 medical schools; see Table 1 for school characteristics. Schools were selected through recruitment at the national 2017 Society of Teachers of Family Medicine (STFM) Conference on Medical Student Education (MSE) and via the STFM MSE Collaborative listserv, posting an invitation with follow-up by phone or email as necessary. All 16 schools that responded and agreed to participate were included. The survey was administered to all students in February of 2017 in order to capture students who had just submitted NRMP rank lists. 18-20
|
|
West
|
South
|
Northeast
|
Midwest
|
|
Public
|
0
|
4
|
1
|
6
|
|
Private
|
0
|
0
|
1
|
3
|
|
Osteopathic
|
0
|
0
|
0
|
1
|
We used an average of the aggregate FMAQ score for each study institution as the measure of an institution’s student attitudes toward family medicine careers. Similarly, we calculated an institutional average for each subset of the FMAQ scale. Subscale domains (Table 2) included lifestyle, which was scored from questions reflecting FM physician work enjoyment, whether FM provided enough comfortable income, and control in work quantity; research, which was scored from statements including the frequency of primary care research and whether research-oriented students should pursue FM; importance, which came from questions regarding how much health care FM physicians provide and whether sick patients rely on family physicians; and shortage, which was measured by opinions on the severity of a lack of primary care physicians, the impact of primary care on overall health in the United States, and if family physicians were an integral health care component.
|
FMAQ Subscale
|
Questionnaire Item
|
|
Relationships
|
To give good care, it is important to consider each patient in the context of his or her family.
Knowledge of family interactions is important in treating individual patients.
Knowledge of patients’ personal background is almost always helpful.
|
|
Competence and Expertise
|
Family physicians have the expertise to deal in-depth with patient problems.
Family medicine requires knowledge that a subspecialist practice may not.
Family physicians’ work is complex and interesting.
Family physicians are particularly capable at providing comprehensive care.
|
|
Lifestyle
|
Enjoying work: family physicians enjoy their work.
Compensation: family medicine provides a physician with enough income to live well.
|
|
Research
|
Research to improve health happens very often in primary care settings.
Most important medical research is conducted by subspecialists.
Research-oriented students should probably not consider family medicine careers.
Primary care physicians are best able to answer many critical research questions.
|
|
Importance
|
Family physicians provide only a small fraction of all health care delivered in the United States.
In the United States people don’t rely on family physicians when they are very sick.
|
|
Shortage
|
The United States has a very serious shortage of primary care physicians.
The United States would provide better for its people if more medical students chose primary care.
The United States health care system can only work well with family physicians playing an integral part.
|
For each study institution, we obtained the 2017 FM graduation rate from published data collected by the American Academy of Family Physicians. 23
We calculated Pearson correlation coefficients between the FM graduation rate and the average student attitude scores for the 16 study institutions. We then conducted a secondary Pearson correlation coefficient analysis to compare FM graduation rate to specific FMAQ data set subset domains including student attitudes toward FM lifestyle, research, importance, and shortage.
This study was considered exempt after review by the Medical College of Wisconsin Institutional Review Board.
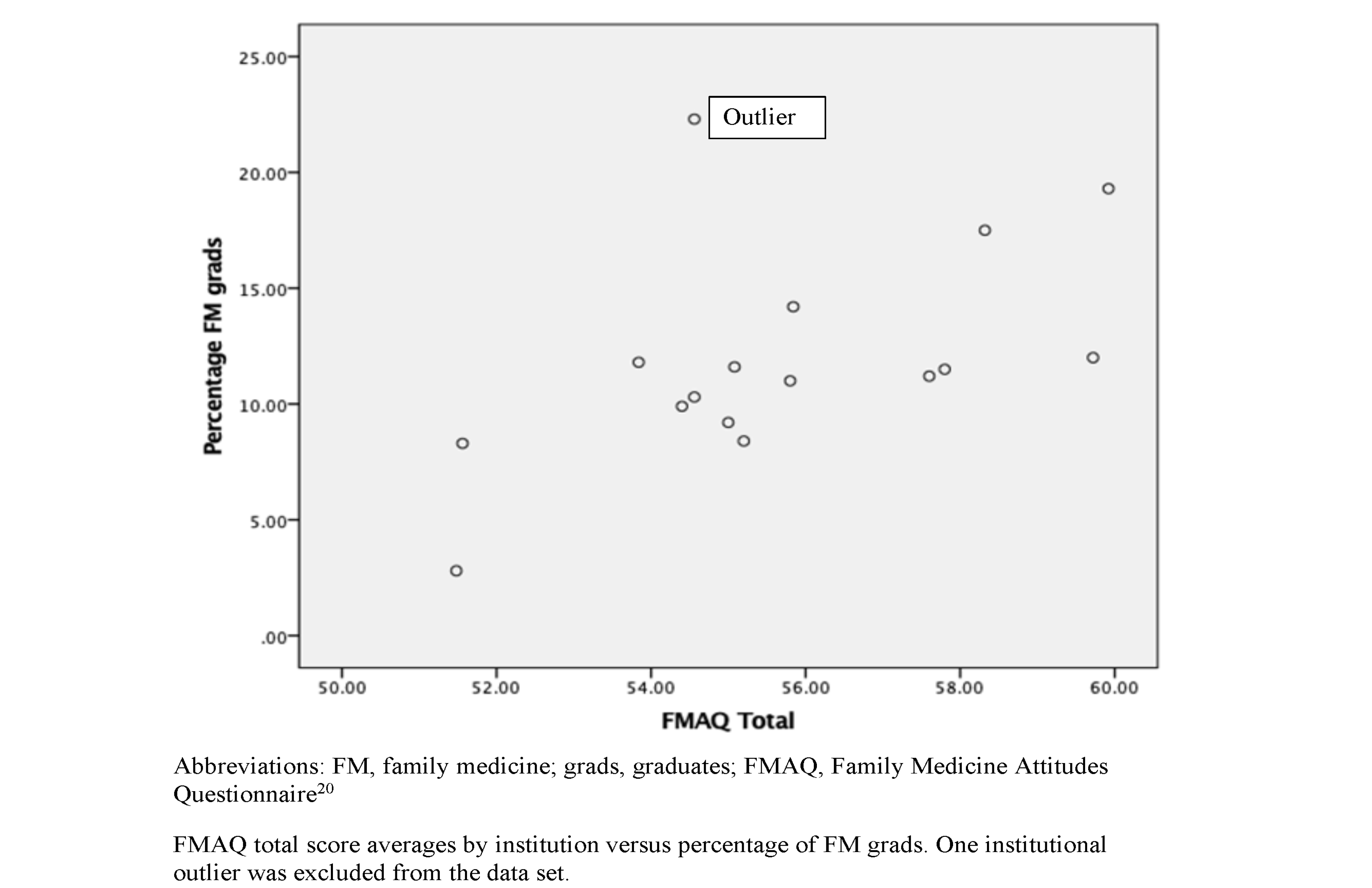
The total FMAQ score (student attitudes) average by school was 55.7 (SD 2.5) with a range of 51.5-59.9. The overall average FM graduation rate was 12.0% (SD 4.6%) with a range of 2.8-22.3%; 1,189 students out of 2,844 completed the survey, for an overall response rate of 41.8%.
Figure 1 shows a scatterplot charting average FMAQ score (x axis) against the percentage of FM graduates (y axis) for the 16 schools. Based on the scatterplot, one school was determined to be an outlier and was removed from further analysis; this was subsequently identified as the only osteopathic school originally included in the data.
Table 3 shows correlations between the FMAQ subscale domains and each school’s percentage of FM graduates. Pearson’s coefficients for each subscale domain were: 0.539 for lifestyle, 0.812 for research, 0.607 for importance, and 0.644 for shortage, respectively. Student attitudes toward FM research was the variable most strongly correlated with an institution’s proportion of FM graduates, as compared to overall FMAQ score and other subdomains.
|
|
Percentage of FM Graduates
|
FMAQ Average Total Score
|
FMAQ FM Lifestyle
|
FMAQ FM Research
|
FMAQ FM Importance
|
FMAQ FM Shortage
|
|
Percentage of FM graduates
|
1
|
0.771
|
0.539
|
0.812
|
0.607
|
0.644
|
Our findings suggest that the attitudes toward family medicine among a medical school’s student body are correlated with the proportion of an institution’s students who seek to match into family medicine residencies. This result is important as medical schools that aim to improve the number of family medicine graduates may consider strategies to impact change at the level of student perceptions, such as positive exposure to family medicine experiences, mentors, and research. 15, 24, 25 AAMC data suggest that about half of students who chose family medicine at graduation had reported a different specialty choice earlier in medical school, which highlights the fluidity of student specialty choice of family medicine and the potential for intervention. 26
The medical student attitude that was most strongly associated with students entering family medicine was a positive perception of family medicine research. At face value, this finding may be surprising, as medical student interest in research has been shown to be inversely correlated with interest in family medicine, 15, 27 and decreased rates of family medicine graduates come from schools that receive higher National Institutes of Health (NIH) funding. 28, 29 However, our study did not measure research output, amount of NIH funding, or a student’s interest in research as was done by previous studies, but rather measured student perceptions of family medicine research, presumably formed from what they have been exposed to through their own medical school experience. Student exposure to family medicine clinician-researchers as role models may support career interest. Institutions with departments that create positive impressions of family medicine research may be influential in creating an institutional environment that supports family medicine career choice. In addition, family medicine departments with strong research records may also be strong in other ways, including education and leadership, which may coalesce to form a reputation for the discipline that is attractive to students. 30, 31
The positive correlation between attitudes toward family medicine research and FM career choice is an important finding for family medicine departments, as the quality and quantity of family medicine research is a modifiable characteristic. Encouraging and supporting family medicine researchers and exposing students to high-quality and impactful research within family medicine departments may be important strategies to bolster the primary care workforce. Additional departmental strategies could include developing enhanced opportunities for medical students to participate in family medicine research projects and emphasizing family physician research during clerkship didactics.
Strategies to improve student perceptions of primary care research should also include increased federal funding for family medicine research. 32, 33, 34 Previous studies have identified the most critical themes of FM research as whole-person, community, lifespan, and population-health; integrating these research themes into medical student FM clerkships, as well as showcasing the scholarship and advocacy work of family physicians and departments, may present a viable means of communicating the value of FM research. 35
Further research is warranted to determine how student attitudes toward FM and FM research may change throughout the course of medical training. Administration of the FMAQ in longitudinal cohorts could help address this question.
Our study did not measure student participation in FM research. Strengths of this study were the multi-institutional nature, use of a validated tool to measure student attitudes, and the inclusion of both primary care interested and noninterested students.
The informal curriculum of a medical school toward primary care, as measured by student attitudes toward family medicine as a career, is correlated with the percentage of a school’s graduates entering family medicine. The most strongly correlated characteristic is a favorable attitude toward family medicine research among responding students. Undergraduate medical institutions and family medicine departments may consider strengthening the support of family medicine research endeavors and increasing the exposure of medical students to family medicine researchers as a strategy to bolster the primary care workforce.
Presentations
This study was previously presented as:
Wendling A, Holihan S, Gomez M, Prunuske J, Phillips J, Kang H. Comparing the Impact of the Formal and Informal Curriculum on Medical Schools’ Contributions to the Primary Care Workforce. STFM Conference on Medical Student Education, Portland, OR; February 2020.
References
-
Ahmed H, Carmody JB. On the Looming Physician Shortage and Strategic Expansion of Graduate Medical Education. Cureus. 2020;12(7):e9216. doi:10.7759/cureus.9216
-
-
Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice.
Acad Med. 2013;88(12):1919-1926.
doi:10.1097/ACM.0000000000000038
-
-
-
-
Prunuske J. America Needs More Family Doctors: The 25x2030 Collaborative Aims to Get More Medical Students into Family Medicine. Am Fam Physician. 2020;101(2):82-83.
-
Ozolins I, Hall H, Peterson R. The student voice: recognising the hidden and informal curriculum in medicine.
Med Teach. 2008;30(6):606-611.
doi:10.1080/01421590801949933
-
Lehmann LS, Sulmasy LS, Desai S; ACP Ethics, Professionalism and Human Rights Committee. Hidden Curricula, Ethics, and Professionalism: Optimizing Clinical Learning Environments in Becoming and Being a Physician: A Position Paper of the American College of Physicians.
Ann Intern Med. 2018;168(7):506-508.
doi:10.7326/M17-2058
-
-
Suchman AL, Williamson PR, Litzelman DK, Frankel RM, Mossbarger DL, Inui TS; Relationship-Centered Care Initiative Discovery Team. Toward an informal curriculum that teaches professionalism. Transforming the social environment of a medical school.
J Gen Intern Med. 2004;19(5 Pt 2):501-504.
doi:10.1111/j.1525-1497.2004.30157.x
-
-
Phillips JP, Petterson SM, Bazemore AW, Phillips RL. A retrospective analysis of the relationship between medical student debt and primary care practice in the United States.
Ann Fam Med. 2014;12(6):542-549.
doi:10.1370/afm.1697
-
Wendling AL, Wudyka AE, Phillips JP, et al. RU4PC? Texting to Quantify Feedback About Primary Care and Its Relationship With Student Career Interest. Fam Med. 2016;48(1):21-29.
-
Seehusen DA, Raleigh MF, Phillips JP, et al. Institutional Characteristics Influencing Medical Student Selection of Primary Care Careers: A Narrative Review and Synthesis.
Fam Med. 2022;54(7):522-530.
doi:10.22454/FamMed.2022.837424
-
Phillips JP, Wendling AL, Prunuske J, et al. Medical School Characteristics, Policies, and Practices That Support Primary Care Specialty Choice: A Scoping Review of 5 Decades of Research.
Fam Med. 2022;54(7):542-554.
doi:10.22454/FamMed.2022.440132
-
Nguyen BM, Liaw W, Polverento ME, et al. Impact of Curricula and Electives on Primary Care Specialty Choice: A Narrative Synthesis.
Fam Med. 2022;54(7):572-577.
doi:10.22454/FamMed.2022.638811
-
Phillips J, Prunuske J, Fitzpatrick L, Mavis B. Initial Development and Validation of a Family Medicine Attitudes Questionnaire.
Fam Med. 2018;50(1):47-51.
doi:10.22454/FamMed.2018.293942
-
Kang H, Prunuske J, Wendling AL, Edwards-Johnson J, Phillips JP. FMAQ-S: Development of a Short Form of the Family Medicine Attitudes Questionnaire.
PRiMER Peer-Rev Rep Med Educ Res. 2021;5:21.
doi:10.22454/PRiMER.2021.767096
-
Phillips JP, Prunuske J, Fitzpatrick L, Mavis B. The Family Medicine Attitudes Questionnaire: A Valid Instrument to Assess Student Attitudes Toward Family Medicine. Fam Med. 2019;51(6):493-501. doi:10.22454/FamMed.2019.957692
-
Wendling AL, Short A, Hetzel F, Phillips JP, Short W. Trends in Subspecialization: A Comparative Analysis of Rural and Urban Clinical Education.
Fam Med. 2020;52(5):332-338.
doi:10.22454/FamMed.2020.182557
-
Deutchman M, Macaluso F, Chao J, et al. Contributions of US Medical Schools to Primary Care (2003-2014): Determining and Predicting Who Really Goes Into Primary Care.
Fam Med. 2020;52(7):483-490.
doi:10.22454/FamMed.2020.785068
-
Phillips JP, Wendling A, Bentley A, Marsee R, Morley CP. Trends in US Medical School Contributions to the Family Physician Workforce: 2018 Update From the American Academy of Family Physicians.
Fam Med. 2019;51(3):241-250.
doi:10.22454/FamMed.2019.395617
-
Kost A, Phillips JP, Polverento ME, et al. The Influence of Role Modeling and Mentorship on Primary Care Career Choice: What Can Be Gleaned From 30 Years of Research?
Fam Med. 2022;54(7):555-563.
doi:10.22454/FamMed.2022.980735
-
Lee AL, Erlich DR, Wendling AL, et al. The Relationship Between Medical School Clerkships and Primary Care Specialty Choice: A Narrative Review.
Fam Med. 2022;54(7):564-571.
doi:10.22454/FamMed.2022.857719
-
-
Senf JH, Campos-Outcalt D, Kutob R. Family medicine specialty choice and interest in research. Fam Med. 2005;37(4):265-270.
-
Choi PA, Xu S, Ayanian JZ. Primary care careers among recent graduates of research-intensive private and public medical schools.
J Gen Intern Med. 2013;28(6):787-792.
doi:10.1007/s11606-012-2286-z
-
Mainous AG 3rd, Porter M, Agana DF, Chessman AW. Institutional NIH Research Funding and a Culture of Support for Family Medicine-Their Relationship to Family Medicine Specialty Choice.
Fam Med. 2018;50(5):369-371.
doi:10.22454/FamMed.2018.913629
-
Weidner A, Peterson LE, Mainous AG III, Datta A, Ewigman B. The Current State of Research Capacity in US Family Medicine Departments.
Fam Med. 2019;51(2):112-119.
doi:10.22454/FamMed.2019.180310
-
Weidner A, Peterson LE, Mainous AG III, Ewigman B. Attitudes and Perceptions of Research Among US Family Medicine Department Chairs.
Fam Med. 2021;53(2):98-103.
doi:10.22454/FamMed.2021.611648
-
Cameron BJ, Bazemore AW, Morley CP. Lost in Translation: NIH Funding for Family Medicine Research Remains Limited.
J Am Board Fam Med. 2016;29(5):528-530.
doi:10.3122/jabfm.2016.05.160063
-
Lucan SC, Phillips RL Jr, Bazemore AW. Off the roadmap? Family medicine’s grant funding and committee representation at NIH.
Ann Fam Med. 2008;6(6):534-542.
doi:10.1370/afm.911
-
Westfall JM, Wittenberg HR, Liaw W. Time to Invest in Primary Care Research-Commentary on Findings from an Independent Congressionally Mandated Study.
J Gen Intern Med. 2021;36(7):2117-2120.
doi:10.1007/s11606-020-06560-0
-
Hester CM, Jiang V, Bartlett-Esquilant G, et al. Supporting Family Medicine Research Capacity: The Critical Role and Current Contributions of US Family Medicine Organizations.
Fam Med. 2019;51(2):120-128.
doi:10.22454/FamMed.2019.318583



There are no comments for this article.